Continuing Education Activity
Lupus pernio is a rare cutaneous manifestation of sarcoidosis. Lupus pernio is a predictive factor for systemic sarcoidosis with thoracic and extra-thoracic involvement. This activity reviews the etiology, evaluation, and management of lupus pernio and highlights the role of the interprofessional team in the care of patients with this condition.
Objectives:
- Identify the etiology of lupus pernio.
- Review the pathogenesis and histopathology of lupus pernio and sarcoidosis.
- Review the treatment and management options available for lupus pernio.
- Explain the role of interprofessional teams in the management of patients with lupus pernio.
Introduction
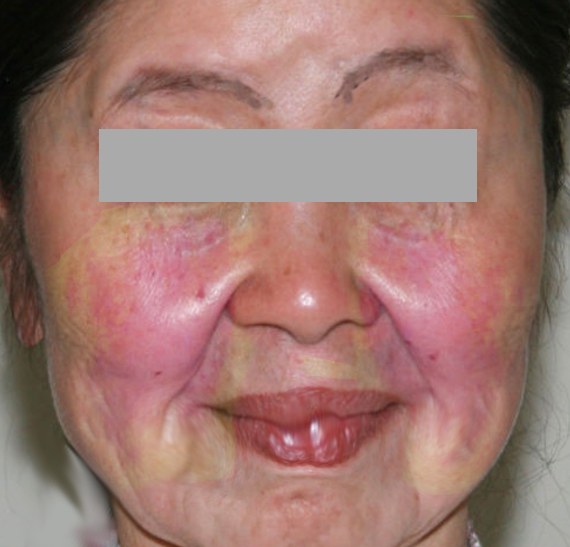
Lupus pernio is a cutaneous manifestation of sarcoidosis, which was first described in 1889 by Ernest Besnier. It presents as a violaceous lesion or shiny nodules over the head and neck but is predominantly localized to the nose, cheeks, and ears.[1] Cutaneous manifestations of sarcoidosis are estimated to occur in approximately 25 percent of patients and the skin lesions help establish the diagnosis of sarcoidosis. Lupus pernio can present either as an isolated skin lesion or it can be an early manifestation of systemic sarcoidosis. Lupus pernio is often a predictor of systemic sarcoidosis, which warrants thorough workup. Patients with lupus pernio have a higher risk for pulmonary disease, which was confirmed in a retrospective study of 516 patients with sarcoidosis. Pulmonary parenchymal involvement was present more often in patients with lupus pernio or sarcoidosis involving scar tissue (64 and 40 percent, respectively) compared to patients with erythema nodosum or other skin lesions of sarcoidosis.[2]
Etiology
The etiology of cutaneous sarcoidosis remains poorly understood. The widely accepted hypothesis suggests sarcoidosis results from a complex interaction between genetic susceptibility, immune dysregulation, and environmental triggers. The granulomatous inflammation is thought to result from an exaggerated cell-mediated immune response to one or more unidentified antigens.[3] Exposure to metals such as beryllium, zirconium, and aluminum is associated with the development of granulomas that are similar to sarcoid granulomas, which suggests a possible role of environmental exposure in the etiology of sarcoidosis. A few microorganisms, most notably mycobacteria and cutibacteria (formerly propionibacteria), have been implicated as possible etiologic agents of sarcoidosis.[4]
Epidemiology
Skin involvement is common in sarcoidosis and it is estimated to occur in approximately 25 percent of patients. The skin lesions are further divided into specific and nonspecific lesions based upon histopathologic features. The annual incidence varies between 1 and 64 per 100,000 depending on the patient population. The real incidence of the disease remains difficult to determine, due to a highly variable clinical presentation and the large proportion of asymptomatic cases. Studies report a greater prevalence of the disease in northern Europe with a reported prevalence of 64 persons per 100,000 population in Sweden.[5] Sarcoidosis is more common among African women and commonly affects individuals aged between 25- to 40-years. Lupus pernio is characterized by a later age of onset and is common in Black females.[6][7]
Pathophysiology
Lupus pernio is characterized by activation of the cell-mediated immune system, typically CD4+ T lymphocytes. The pathogenesis involves autoimmune dysregulation with activation of the Th1 immune pathway in response to one or more extrinsic antigens. CD4+ helper T lymphocytes amplify the immune response through the release of interferon-gamma, interleukin (IL)-2, and other cytokines, aided by T regulatory cells (Tregs). The release of cytokines interferon-gamma and tumor necrosis factor (TNF) alpha promotes macrophage accumulation, activation, and aggregation, resulting in granulomatous inflammation.
Histopathology
The presence of non-caseating epithelioid cell granulomas with a variety of Langerhans giant cells is the histopathologic hallmark of lupus pernio. Immunohistochemical staining predominantly demonstrates CD4+ Th1 lymphocytes within the granuloma. However, the periphery of the granuloma is composed of CD4+ as well as CD8+ T cells. The proportions of lymphocytic infiltrate and fibrosis in the granulomas vary depending on the patient and disease duration. In some patients, the giant cells have intracytoplasmic inclusions like asteroid bodies, Schaumann bodies, and birefringent crystalline particles.
History and Physical
Lupus pernio is characterized by violaceous or erythematous, indurated plaques that are primarily distributed on the central face involving the nose and cheeks. Lesions can also involve the ears and very rarely the dorsum of hands and feet. Lupus pernio can present as a few small nodules on the nose to exuberant plaques spreading across both cheeks.[8] The lesions of lupus pernio start insidiously but progressively infiltrate and indurate into the underlying cartilage and bone, causing disfigurement. Lupus pernio is associated with an increased risk of extracutaneous involvement particularly the respiratory tract. In a study of 35 patients with lupus pernio, systemic sarcoidosis with intrathoracic involvement was observed in 74% of cases, and upper respiratory tract disease was reported in 54% of patients.[7] Therefore, a workup for systemic sarcoidosis should be considered in patients with lupus pernio.
Evaluation
The diagnosis of cutaneous sarcoidosis is often made by the recognition of compatible clinical features and the detection of classic histopathologic findings. Lupus pernio is associated with a higher risk of extracutaneous sarcoidosis and most commonly involves the respiratory tract. Dermatoscopic examination of the skin lesions may assist in identifying granulomatous skin lesions but it is a non-specific study. All skin lesions concerning lupus pernio should be biopsied to confirm the histopathologic diagnosis.
A thorough history and physical examination should be done to identify extra-cutaneous involvement. An initial evaluation should include a chest x-ray and pulmonary function tests to look for any involvement of the respiratory tract. Laboratory analysis may show elevated C-reactive protein level and erythrocyte sedimentation rate. A high serum angiotensin-converting enzyme level, although not specific to sarcoidosis and increased in only 60% of patients with sarcoidosis,[9] can aid in the diagnosis.
In some patients, further imaging should be considered including high resolution computed tomography (HRCT) chest, echocardiogram, or hand and feet radiographs based on clinical suspicion. In patients with no systemic involvement at initial evaluation, a long-term follow-up with close clinical and radiological supervision is warranted, as patients may develop systemic symptoms later on the course of the disease.
Treatment / Management
Lupus pernio is a rare form of cutaneous sarcoidosis, which is resistant to therapy compared to other skin manifestations of sarcoidosis and can result in scarring and disfiguration. There have been very few randomized trials in sarcoidosis that have evaluated therapies, and current evidence on most treatments was derived from small uncontrolled prospective studies, retrospective analyses, and case reports. The choice of initial therapy is based on the location, extent, and severity of skin involvement.
Topical or intralesional corticosteroids are often the first choice in the treatment of cutaneous sarcoidosis. But intralesional steroid injections like triamcinolone are preferred due to better therapeutic response in lupus pernio.[10] Treatment often must be more aggressive to achieve good results and avoid scarring. Injections are repeated every 3-4 weeks until there is clinical remission.
Topical calcineurin inhibitors like tacrolimus 0.1% ointment or pimecrolimus 1% cream are used in conjunction with steroids to reduce corticosteroid use in patients requiring long-term or frequent use to maintain remission.
Systemic glucocorticoids like oral prednisone are only considered in patients with rapidly progressing skin lesions or those with lesions with disfiguration and the initial dose is prednisone 0.5 - 1 mg/kg. Once there is a clinical response the prednisone dose is tapered slowly by 5 mg every week. If the lesions recur with prednisone taper, patients should be started on methotrexate.
Systemic agents like hydroxychloroquine, methotrexate, and minocycline are used for patients with extensive skin involvement, and patients who did not respond to initial therapies like corticosteroids. Hydroxychloroquine and methotrexate have immunomodulatory effects and the selection of the agent is based on the patient's comorbidities, contraindications, and medication tolerance. Hydroxychloroquine 200 mg or 400 mg once a day is the usual dose and patients require once a year eye exam for toxicity monitoring.
The methotrexate dose varies from 5 mg to 25 mg orally once a week based on the severity of the lesions. It has a faster therapeutic response compared to hydroxychloroquine but warrants frequent lab monitoring for methotrexate toxicity. Patients need blood tests every 3 months to monitor complete blood count and comprehensive metabolic panel.
Tumor necrosis factor-alpha inhibitors like adalimumab and infliximab are indicated in patients with lupus pernio who are resistant to treatments like methotrexate, hydroxychloroquine, and oral prednisone. Adalimumab 40 mg subcutaneous injection once a week was shown to be effective compared to placebo in a small randomized controlled trial (RCT) of patients with cutaneous sarcoidosis.[11][12] A systematic review of non-randomized studies showed infliximab infusions were superior to placebo and demonstrate partial or complete response in patients with cutaneous sarcoidosis.[13]
Thalidomide is also an option for patients with resistant lupus pernio and its use is based on case reports and non-randomized studies. However, the potential toxicities and teratogenic side effects limit its utility. The patient and provider must enroll in the thalidomide risk evaluation and mitigation strategy (REMS) program before thalidomide can be prescribed and dispensed.
Surgical excision of cutaneous sarcoidosis lesions is not recommended as there is a high risk of recurrence in the surgical scars. However, reconstructive surgery can be considered for improvement in cosmetic appearance in patients with severely disfiguring lesions on the nose.
Differential Diagnosis
The distinctive appearance of lupus pernio makes it an easily recognizable manifestation of sarcoidosis. However, a few differential diagnoses can mimic its clinical presentation, including fungal infection, lupus vulgaris, berylliosis, lymphoma cutis, lupus erythematosus, and tuberculoid leprosy that have a similar pattern of distribution. The cutaneous examination is usually enough to differentiate most of these lesions, but in some cases, a biopsy is necessary for a definitive diagnosis.
Prognosis
Lupus pernio lesions can insidiously infiltrate and indurate into the underlying cartilage and cause disfigurement. It is also very resistant to treatments compared to other forms of cutaneous sarcoidosis. Lupus pernio is a predictive factor of more progressive sarcoidosis with a prolonged course and a more severe thoracic and extra-thoracic involvement.[14] Early diagnosis and prompt treatment are recommended to prevent induration and disfiguring lesions.
Complications
Lupus pernio lesions over the face can infiltrate and indurate the cartilage causing disfigurement. Granulomatous infiltration of the nasal mucosa and bone results in ulceration and septal perforation. However, the most severe complications result from systemic organ involvement, including pulmonary, cardiac, or central nervous system involvement.
Deterrence and Patient Education
Patients with cutaneous sarcoidosis should be educated about their diagnosis, its chronicity, and the increased association with pulmonary sarcoidosis. The health care providers should convey the importance of regular follow-ups for disease monitoring and medication toxicity monitoring. Patients should be educated about the common symptoms of specific organ involvement as some of them may develop symptoms several years after the initial presentation.
Patients on medications like methotrexate should be educated about contraception to avoid pregnancy while taking it. They should receive age-appropriate vaccines prior to initiating anti-TNF-alfa antagonists.
Enhancing Healthcare Team Outcomes
Lupus pernio is a rare form of cutaneous sarcoidosis which often requires the expertise of multiple providers including a dermatologist and a pathologist in establishing the diagnosis. Sarcoidosis is a multisystem disease with potentially life-threatening complications that warrants the importance of coordinated care provided by an interprofessional team. Patients would benefit from pharmacy education regarding potential medication side effects and possible drug interactions. The choice of therapy is often decided by the interprofessional team after assessing the severity and the extent of sarcoidosis. Patients with cosmetic disfigurement should be referred to plastic surgeons for reconstructive surgery.