Case Presentation
A 32-year-old male with no significant past medical history presents to the emergency department with abdominal pain. He states the pain began a few days ago in the right lower quadrant of the abdomen and now feels as though it is spreading to the mid-abdomen.
He describes the pain as coming on suddenly and sharp in nature. Since the onset, his pain started to improve until the morning of his presentation to the emergency department, when it acutely worsened. He says that the pain is much worse with movement.
The patient is concerned about a possible hernia as he does heavy lifting at work. Review of systems is negative, including no anorexia, no nausea or vomiting, no testicular pain or swelling, no urinary or bowel complaints, and no fevers or chills.
The patient denies prior abdominal surgeries. He does smoke a half pack of cigarettes a day, drinks alcohol socially, and denies any recreational drug use. He notes no inherited medical conditions in his family.
Vital signs on arrival:
- Blood pressure (BP) 120/73
- Heart rate (HR) 60
- RR 18
- Temperature: 35.6 C
- Oxygen saturation: 98% on room air
- Height 5'10" (178 cm)
- Weight 154 lbs (70 kg)
Physical Exam
- General: Alert and oriented, in no apparent distress, although ambulates into the emergency room holding his abdomen.
- HEENT: Normocephalic, atraumatic, sclera anicteric. Mucus membranes are moist.
- Cardiovascular (CV): Regular rate and rhythm, no murmurs, rubs, gallops
- Pulmonary: clear to auscultation bilaterally
- Abdomen: moderate tenderness to palpation in the right lower quadrant without rebound, guarding, or rigidity. Bowel sounds are present throughout. Negative psoas and obturator signs.
- Genitourinary (GU): genitalia examined in a standing position with a normal external exam, no masses felt with a cough, intact cremasteric reflex
- Back: No cerebrovascular (CVA) tenderness
- Neurological: No focal deficits
- Skin: Warm and dry, no rashes
Initial Evaluation
Initial tests were performed, including blood testing consisting of a complete blood count (CBC), basic metabolic panel (BMP), lipase, and liver function test (LFT), as well as a urinalysis. Lab work was remarkable for no acute abnormalities except for a mild leukocytosis of 12.4.
CBC
- WBC 12.4 x 10 /mcl (81% neutrophils, 11% lymphocytes, 6% monocytes, 2% eosinophils, no bands)
- HGB/HCT 14.6/44.6 g/dl
- PLT 356 x 10 /mcl
BMP
- Gluc 93 mg/dl
- BUN/CR 17/1.08 mg/dl
- Na 138 mmol/L
- K 4.4 mmol/L
- Cl 107 mmol/L
- CO2 25 mmol/L
- Ca 9.7 mg/dl
Lipase
LFT
- Total bilirubin 0.3 (0.07 direct) mg/dl
- AST 17 Intl U/L
- ALT 15 Intl U/L
- AlkPhos 64 Intl U/L
- Total protein 6.76 g/dl
Urinalysis
- Clear yellow
- Negative for glucose, bilirubin, blood, protein, urobilinogen, nitrite, leukocyte esterase
- Trace ketones
- Sp gravity 1.027
- pH 5.0
Differential Diagnosis
In a young, healthy adult male presenting with right lower quadrant abdominal pain, the differential diagnosis includes appendicitis, typhlitis, epiploic appendagitis, perforated viscous, inflammatory bowel disease, diverticulitis, small bowel obstruction, testicular torsion, epididymitis, hernia, urinary tract infection, and pyelonephritis. Extra-abdominal causes such as abdominal muscle strain or a hernia and skin disorders such as herpes zoster viral infection are less likely.[1]
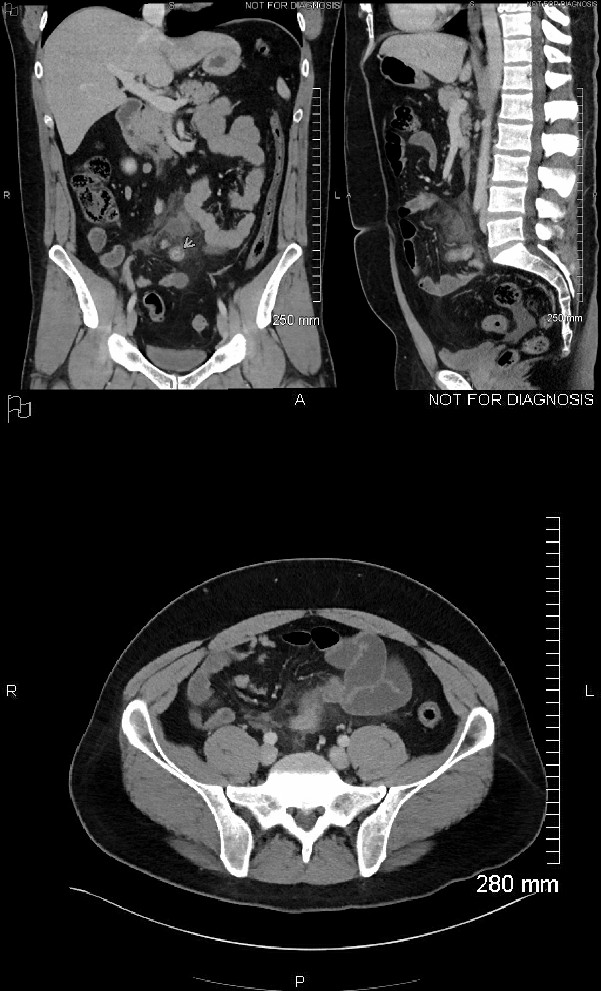
Confirmatory Evaluation
A CT scan with intravenous contrast was ordered. This was interpreted by the radiologist noting a blind ending. The inflamed appendage is emanating from the small bowel, with an incomplete superior wall and fluid layering in the deep pelvis, concerning for perforated Meckel diverticulum. Surgical consultation was initiated in the emergency department, and the patient was taken to the operating room for an exploratory laparotomy confirming the diagnosis of perforated Meckel's diverticulum. The subsequent pathology report also noted Meckel's diverticulum with gastric heterotopia and feature consistent with perforation and serositis.
Diagnosis
Meckel’s diverticulum is a congenital anomaly resulting from the abnormal embryonic separation of the omphalomesenteric duct. Meckel’s diverticulum is a true diverticulum comprised of all 3 layers of the gastrointestinal (GI) tract, including mucosa, submucosa, and adventitia.[2] Meckel’s diverticulum usually consists of heterotopic tissue, most commonly gastric mucosa, due to the pluripotential cell line of the omphalomesenteric duct. Other heterotopic tissue found on pathological specimens of Meckel's diverticulum may include pancreatic, jejunal, duodenal, and, less commonly, colonic, rectal, or endometrial. Epidemiologically, Meckel’s diverticulum tends to follow the rule of 2s:[2]
- Occurs in 2% of the population
- Located within 2 feet of the ileocecal valve
- Two centimeters in length
- Two times as likely to be symptomatic in young boys as compared to young girls
- Symptoms often present before the age of 2
Although Meckel's diverticulum is usually asymptomatic and may never be identified until autopsy reports, it can lead to serious complications, most notably hemorrhage, obstruction, perforation, or infection. Hemorrhage occurs secondary to acid secretion from the gastric mucosa that forms ulcerations along the intestinal mucosa and can lead to painless rectal bleeding, typically in children. Bleeding can be substantial and may require transfusions.[2]
The diverticulum can also serve as a lead point for an ileocolic or ileoileal intussusception, as well as a turning point for a volvulus. If symptomatic, patients typically complain of crampy, right lower quadrant abdominal pain. Finally, erosion of nearby intestinal mucosa or inflammation of the diverticulum itself can lead to perforation, or the diverticulum itself can become inflamed, leading to diverticulitis.[3]
Evaluation of a patient with suspected complications from Meckel's diverticulum includes multiple options. Lab testing is largely unremarkable, but hemoglobin and hematocrit should be checked as mild to moderate anemia may develop if there is bleeding. If there is significant bleeding, transfusions may be necessary. Electrolyte levels and kidney function testing are not helpful for diagnosis but can help guide treatment options.[1]
Multiple imaging modalities exist to evaluate suspected Meckel's diverticulum. If a patient, especially a young child, presents with GI bleeding, the test of choice is a technetium-99 pertechnetate scintiscan. The pertechnetate will be absorbed by the gastric mucosa and will be detected when scanned by a gamma camera. This is the preferred scan due to ease and accuracy; however, false negative tests do occur if the diverticulum is comprised of other tissue other than gastric mucosa.[4]
If intestinal obstruction or perforation of Meckel's diverticulum is suspected, then a CT scan may be helpful, whereas ultrasonography has been useful if the clinical picture suggests intussusception. Overall, Meckel's diverticulum may be found incidentally on routine imaging or during a surgical procedure or may only be recognized when complications arise.[1]
Management
In many cases, the diverticulum is found incidentally on laparotomy or laparoscopy, and it becomes the surgeon’s decision on whether or not to remove the diverticulum to prevent future complications. The lifetime risk of complications is 4.2%, and the risk decreases with age.[1] Therefore, the decision for diverticulectomy is favored in asymptomatic patients who are young and have a long diverticulum (typically greater than 2 cm) with a narrow neck and fibrous banding or if it appears to be comprised of gastric mucosa and is inflamed or thickened. However, in a symptomatic patient, medical management is limited to supportive care, including possible antibiotic administration, and surgical resection is required for definitive treatment.[1]
Discussion
Abdominal pain is an extremely common complaint in the emergency department, with a large differential ranging from very benign etiologies to life-threatening emergencies. Keeping a large differential can help guide diagnosis and treatment options. Although relatively rare, serious complications can arise in someone with Meckel's diverticulum and the definitive treatment is a surgical intervention for removal and repair. Meckel's diverticulum is often an incidental finding, and if found during surgery, removal is typically up to the discretion of the surgeon. Surgeons have determined certain guidelines to drive their decision to remove an asymptomatic diverticulum to prevent future complications.[1]
These parameters are listed above but include younger age, diverticulum lengths greater than 2 centimeters, presence of gastric mucosa, and male gender. However, there is no significant evidence to determine whether or not this approach changes morbidity or mortality. If painless rectal bleeding is the presenting symptom, a technetium-99 scan may be appropriate for diagnosis. However, for patients that present with abdominal pain and physical exam concerning for perforation, intestinal obstruction, or intra-abdominal abscess, a CT scan is more appropriate for diagnosis. After diagnosis, prompt surgical consultation and operative management are necessary.[4]
Pearls of Wisdom
Meckel's diverticulum is a rare diagnosis in adults but should always be on the differential of patients who present with lower abdominal bleeding or abdominal pain.
Meckel's diverticulum, which contains gastric tissue, may be detected with a technetium-99 scan, which is an appropriate first imaging test in patients with painless lower abdominal bleeding.
Remember "the rule of 2s:"
- Occurs in 2% of the population
- Located within 2 feet of the ileocecal valve
- Two centimeters in length
- Two times as likely to be symptomatic in young boys as compared to young girls
- Symptoms often present before the age of 2