[1]
Chowdhury F, Ross AG, Islam MT, McMillan NAJ, Qadri F. Diagnosis, Management, and Future Control of Cholera. Clinical microbiology reviews. 2022 Sep 21:35(3):e0021121. doi: 10.1128/cmr.00211-21. Epub 2022 Jun 21
[PubMed PMID: 35726607]
[2]
Dick MH, Guillerm M, Moussy F, Chaignat CL. Review of two decades of cholera diagnostics--how far have we really come? PLoS neglected tropical diseases. 2012:6(10):e1845. doi: 10.1371/journal.pntd.0001845. Epub 2012 Oct 11
[PubMed PMID: 23071851]
[3]
Schaetti C, Sundaram N, Merten S, Ali SM, Nyambedha EO, Lapika B, Chaignat CL, Hutubessy R, Weiss MG. Comparing sociocultural features of cholera in three endemic African settings. BMC medicine. 2013 Sep 18:11():206. doi: 10.1186/1741-7015-11-206. Epub 2013 Sep 18
[PubMed PMID: 24047241]
[4]
Kanungo S, Azman AS, Ramamurthy T, Deen J, Dutta S. Cholera. Lancet (London, England). 2022 Apr 9:399(10333):1429-1440. doi: 10.1016/S0140-6736(22)00330-0. Epub
[PubMed PMID: 35397865]
[6]
Legros D, Partners of the Global Task Force on Cholera Control. Global Cholera Epidemiology: Opportunities to Reduce the Burden of Cholera by 2030. The Journal of infectious diseases. 2018 Oct 15:218(suppl_3):S137-S140. doi: 10.1093/infdis/jiy486. Epub
[PubMed PMID: 30184102]
[7]
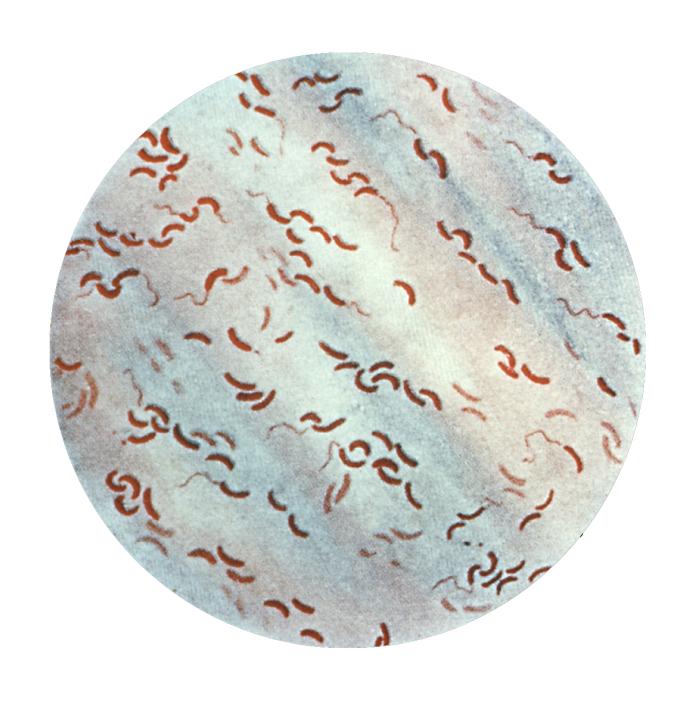
Baron S, Finkelstein RA. Cholera, Vibrio cholerae O1 and O139, and Other Pathogenic Vibrios. Medical Microbiology. 1996:():
[PubMed PMID: 21413330]
[8]
Merrell DS, Butler SM, Qadri F, Dolganov NA, Alam A, Cohen MB, Calderwood SB, Schoolnik GK, Camilli A. Host-induced epidemic spread of the cholera bacterium. Nature. 2002 Jun 6:417(6889):642-5
[PubMed PMID: 12050664]
[9]
Dutta D, Chowdhury G, Pazhani GP, Guin S, Dutta S, Ghosh S, Rajendran K, Nandy RK, Mukhopadhyay AK, Bhattacharya MK, Mitra U, Takeda Y, Nair GB, Ramamurthy T. Vibrio cholerae non-O1, non-O139 serogroups and cholera-like diarrhea, Kolkata, India. Emerging infectious diseases. 2013 Mar:19(3):464-7. doi: 10.3201/eid1903.121156. Epub
[PubMed PMID: 23622872]
[10]
Somboonwit C, Menezes LJ, Holt DA, Sinnott JT, Shapshak P. Current views and challenges on clinical cholera. Bioinformation. 2017:13(12):405-409. doi: 10.6026/97320630013405. Epub 2017 Dec 31
[PubMed PMID: 29379258]
[11]
Oprea M, Njamkepo E, Cristea D, Zhukova A, Clark CG, Kravetz AN, Monakhova E, Ciontea AS, Cojocaru R, Rauzier J, Damian M, Gascuel O, Quilici ML, Weill FX. The seventh pandemic of cholera in Europe revisited by microbial genomics. Nature communications. 2020 Oct 22:11(1):5347. doi: 10.1038/s41467-020-19185-y. Epub 2020 Oct 22
[PubMed PMID: 33093464]
[12]
Waldor MK, Mekalanos JJ. Lysogenic conversion by a filamentous phage encoding cholera toxin. Science (New York, N.Y.). 1996 Jun 28:272(5270):1910-4
[PubMed PMID: 8658163]
[13]
Siddique AK, Cash R. Cholera outbreaks in the classical biotype era. Current topics in microbiology and immunology. 2014:379():1-16. doi: 10.1007/82_2013_361. Epub
[PubMed PMID: 24368696]
[14]
Raslan R, El Sayegh S, Chams S, Chams N, Leone A, Hajj Hussein I. Re-Emerging Vaccine-Preventable Diseases in War-Affected Peoples of the Eastern Mediterranean Region-An Update. Frontiers in public health. 2017:5():283. doi: 10.3389/fpubh.2017.00283. Epub 2017 Oct 25
[PubMed PMID: 29119098]
[15]
Davies HG, Bowman C, Luby SP. Cholera - management and prevention. The Journal of infection. 2017 Jun:74 Suppl 1():S66-S73. doi: 10.1016/S0163-4453(17)30194-9. Epub
[PubMed PMID: 28646965]
[16]
Nelson EJ, Harris JB, Morris JG Jr, Calderwood SB, Camilli A. Cholera transmission: the host, pathogen and bacteriophage dynamic. Nature reviews. Microbiology. 2009 Oct:7(10):693-702. doi: 10.1038/nrmicro2204. Epub
[PubMed PMID: 19756008]
[17]
Reidl J, Klose KE. Vibrio cholerae and cholera: out of the water and into the host. FEMS microbiology reviews. 2002 Jun:26(2):125-39
[PubMed PMID: 12069878]
[18]
Hartley DM, Morris JG Jr, Smith DL. Hyperinfectivity: a critical element in the ability of V. cholerae to cause epidemics? PLoS medicine. 2006 Jan:3(1):e7
[PubMed PMID: 16318414]
[19]
Harris JB, Khan AI, LaRocque RC, Dorer DJ, Chowdhury F, Faruque AS, Sack DA, Ryan ET, Qadri F, Calderwood SB. Blood group, immunity, and risk of infection with Vibrio cholerae in an area of endemicity. Infection and immunity. 2005 Nov:73(11):7422-7
[PubMed PMID: 16239542]
[20]
Czerwiński M. [Blood groups - minuses and pluses. Do the blood group antigens protect us from infectious diseases?]. Postepy higieny i medycyny doswiadczalnej (Online). 2015 Jun 25:69():703-22. doi: 10.5604/17322693.1158795. Epub 2015 Jun 25
[PubMed PMID: 26206987]
[21]
Levine MM, Black RE, Clements ML, Cisneros L, Nalin DR, Young CR. Duration of infection-derived immunity to cholera. The Journal of infectious diseases. 1981 Jun:143(6):818-20
[PubMed PMID: 7252264]
[22]
De Keukeleire S, Hoste P, Crivits M, Hammami N, Piette A. Atypical manifestation of Vibrio cholerae: fear the water! Acta clinica Belgica. 2018 Dec:73(6):462-464. doi: 10.1080/17843286.2018.1483563. Epub 2018 Jun 19
[PubMed PMID: 29916306]
[23]
Knirel YA, Widmalm G, Senchenkova SN, Jansson PE, Weintraub A. Structural studies on the short-chain lipopolysaccharide of Vibrio cholerae O139 Bengal. European journal of biochemistry. 1997 Jul 1:247(1):402-10
[PubMed PMID: 9249053]
[24]
Lippi D, Gotuzzo E, Caini S. Cholera. Microbiology spectrum. 2016 Aug:4(4):. doi: 10.1128/microbiolspec.PoH-0012-2015. Epub
[PubMed PMID: 27726771]
[25]
Harris JB, LaRocque RC, Qadri F, Ryan ET, Calderwood SB. Cholera. Lancet (London, England). 2012 Jun 30:379(9835):2466-2476. doi: 10.1016/S0140-6736(12)60436-X. Epub
[PubMed PMID: 22748592]
[27]
Wang F, Butler T, Rabbani GH, Jones PK. The acidosis of cholera. Contributions of hyperproteinemia, lactic acidemia, and hyperphosphatemia to an increased serum anion gap. The New England journal of medicine. 1986 Dec 18:315(25):1591-5
[PubMed PMID: 3785323]
[28]
Ma T, Thiagarajah JR, Yang H, Sonawane ND, Folli C, Galietta LJ, Verkman AS. Thiazolidinone CFTR inhibitor identified by high-throughput screening blocks cholera toxin-induced intestinal fluid secretion. The Journal of clinical investigation. 2002 Dec:110(11):1651-8
[PubMed PMID: 12464670]
[29]
Dube A, Moffatt M, Davison C, Bartels S. Health Outcomes for Children in Haiti Since the 2010 Earthquake: A Systematic Review. Prehospital and disaster medicine. 2018 Feb:33(1):77-88. doi: 10.1017/S1049023X17007105. Epub 2017 Dec 18
[PubMed PMID: 29248034]
[30]
Barzilay EJ, Schaad N, Magloire R, Mung KS, Boncy J, Dahourou GA, Mintz ED, Steenland MW, Vertefeuille JF, Tappero JW. Cholera surveillance during the Haiti epidemic--the first 2 years. The New England journal of medicine. 2013 Feb 14:368(7):599-609. doi: 10.1056/NEJMoa1204927. Epub 2013 Jan 9
[PubMed PMID: 23301694]
[31]
Boncy J, Rossignol E, Dahourou G, Hast M, Buteau J, Stanislas M, Moffett D, Bopp C, Balajee SA. Performance and utility of a rapid diagnostic test for cholera: notes from Haiti. Diagnostic microbiology and infectious disease. 2013 Aug:76(4):521-3. doi: 10.1016/j.diagmicrobio.2013.03.010. Epub
[PubMed PMID: 23886437]
[32]
Hasan JA, Huq A, Nair GB, Garg S, Mukhopadhyay AK, Loomis L, Bernstein D, Colwell RR. Development and testing of monoclonal antibody-based rapid immunodiagnostic test kits for direct detection of Vibrio cholerae O139 synonym Bengal. Journal of clinical microbiology. 1995 Nov:33(11):2935-9
[PubMed PMID: 8576349]
[33]
Ontweka LN, Deng LO, Rauzier J, Debes AK, Tadesse F, Parker LA, Wamala JF, Bior BK, Lasuba M, But AB, Grandesso F, Jamet C, Cohuet S, Ciglenecki I, Serafini M, Sack DA, Quilici ML, Azman AS, Luquero FJ, Page AL. Cholera Rapid Test with Enrichment Step Has Diagnostic Performance Equivalent to Culture. PloS one. 2016:11(12):e0168257. doi: 10.1371/journal.pone.0168257. Epub 2016 Dec 19
[PubMed PMID: 27992488]
[34]
Debes AK, Ateudjieu J, Guenou E, Ebile W, Sonkoua IT, Njimbia AC, Steinwald P, Ram M, Sack DA. Clinical and Environmental Surveillance for Vibrio cholerae in Resource Constrained Areas: Application During a 1-Year Surveillance in the Far North Region of Cameroon. The American journal of tropical medicine and hygiene. 2016 Mar:94(3):537-543. doi: 10.4269/ajtmh.15-0496. Epub 2016 Jan 11
[PubMed PMID: 26755564]
[35]
Sayeed MA, Islam K, Hossain M, Akter NJ, Alam MN, Sultana N, Khanam F, Kelly M, Charles RC, Kováč P, Xu P, Andrews JR, Calderwood SB, Amin J, Ryan ET, Qadri F. Development of a new dipstick (Cholkit) for rapid detection of Vibrio cholerae O1 in acute watery diarrheal stools. PLoS neglected tropical diseases. 2018 Mar:12(3):e0006286. doi: 10.1371/journal.pntd.0006286. Epub 2018 Mar 14
[PubMed PMID: 29538377]
[36]
Matias WR, Julceus FE, Abelard C, Mayo-Smith LM, Franke MF, Harris JB, Ivers LC. Laboratory evaluation of immunochromatographic rapid diagnostic tests for cholera in Haiti. PloS one. 2017:12(11):e0186710. doi: 10.1371/journal.pone.0186710. Epub 2017 Nov 1
[PubMed PMID: 29091945]
[37]
Banwell JG. Worldwide impact of oral rehydration therapy. Clinical therapeutics. 1990:12 Suppl A():29-36; discussion 36-7
[PubMed PMID: 2187610]
[38]
Liamis G, Filippatos TD, Elisaf MS. Correction of hypovolemia with crystalloid fluids: Individualizing infusion therapy. Postgraduate medicine. 2015 May:127(4):405-12. doi: 10.1080/00325481.2015.1029421. Epub 2015 Mar 26
[PubMed PMID: 25812486]
[39]
Mahalanabis D, Wallace CK, Kallen RJ, Mondal A, Pierce NF. Water and electrolyte losses due to cholera in infants and small children: a recovery balance study. Pediatrics. 1970 Mar:45(3):374-85
[PubMed PMID: 5442912]
[40]
Nalin DR, Cash RA, Islam R, Molla M, Phillips RA. Oral maintenance therapy for cholera in adults. Lancet (London, England). 1968 Aug 17:2(7564):370-3
[PubMed PMID: 4173788]
[41]
Murphy C, Hahn S, Volmink J. Reduced osmolarity oral rehydration solution for treating cholera. The Cochrane database of systematic reviews. 2004 Oct 18:(4):CD003754
[PubMed PMID: 15495063]
[42]
Lebenthal E, Khin-Maung-U, Khin-Myat-Tun, Tin-Nu-Swe, Thein-Thein-Myint, Jirapinyo P, Visitsuntorn N, Ismail R, Bakri A, Firmansyah A. High-calorie, rice-derived, short-chain, glucose polymer-based oral rehydration solution in acute watery diarrhea. Acta paediatrica (Oslo, Norway : 1992). 1995 Feb:84(2):165-72
[PubMed PMID: 7538837]
[43]
Pierce NF, Fontaine O, Sack RB. Amylase-resistant starch plus oral rehydration solution for cholera. The New England journal of medicine. 2000 Jun 29:342(26):1995-6
[PubMed PMID: 10877651]
[44]
Gregorio GV, Gonzales ML, Dans LF, Martinez EG. Polymer-based oral rehydration solution for treating acute watery diarrhoea. The Cochrane database of systematic reviews. 2016 Dec 13:12(12):CD006519. doi: 10.1002/14651858.CD006519.pub3. Epub 2016 Dec 13
[PubMed PMID: 27959472]
Level 1 (high-level) evidence
[45]
Bhattacharyya AK, Hati AK. WHO formula of ORS and home made ORS. Journal of the Indian Medical Association. 1994 Feb:92(2):69-70
[PubMed PMID: 8071565]
[46]
Butler T. Treatment of severe cholera: a review of strategies to reduce stool output and volumes of rehydration fluid. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2017 May 1:111(5):204-210. doi: 10.1093/trstmh/trx041. Epub
[PubMed PMID: 28957470]
[47]
Wright EM, Loo DD, Hirayama BA. Biology of human sodium glucose transporters. Physiological reviews. 2011 Apr:91(2):733-94. doi: 10.1152/physrev.00055.2009. Epub
[PubMed PMID: 21527736]
[48]
Centers for Disease Control and Prevention (CDC). Update on cholera --- Haiti, Dominican Republic, and Florida, 2010. MMWR. Morbidity and mortality weekly report. 2010 Dec 24:59(50):1637-41
[PubMed PMID: 21178947]
[49]
Leibovici-Weissman Y, Neuberger A, Bitterman R, Sinclair D, Salam MA, Paul M. Antimicrobial drugs for treating cholera. The Cochrane database of systematic reviews. 2014 Jun 19:2014(6):CD008625. doi: 10.1002/14651858.CD008625.pub2. Epub 2014 Jun 19
[PubMed PMID: 24944120]
[50]
GREENOUGH WB 3rd, GORDON RS Jr, ROSENBERG IS, DAVIES BI, BENENSON AS. TETRACYCLINE IN THE TREATMENT OF CHOLERA. Lancet (London, England). 1964 Feb 15:1(7329):355-7
[PubMed PMID: 14090856]
Level 3 (low-level) evidence
[51]
Bhandari N, Mazumder S, Taneja S, Dube B, Agarwal RC, Mahalanabis D, Fontaine O, Black RE, Bhan MK. Effectiveness of zinc supplementation plus oral rehydration salts compared with oral rehydration salts alone as a treatment for acute diarrhea in a primary care setting: a cluster randomized trial. Pediatrics. 2008 May:121(5):e1279-85. doi: 10.1542/peds.2007-1939. Epub
[PubMed PMID: 18450870]
[52]
Imdad A, Mayo-Wilson E, Herzer K, Bhutta ZA. Vitamin A supplementation for preventing morbidity and mortality in children from six months to five years of age. The Cochrane database of systematic reviews. 2017 Mar 11:3(3):CD008524. doi: 10.1002/14651858.CD008524.pub3. Epub 2017 Mar 11
[PubMed PMID: 28282701]
[53]
Li ST, Grossman DC, Cummings P. Loperamide therapy for acute diarrhea in children: systematic review and meta-analysis. PLoS medicine. 2007 Mar 27:4(3):e98
[PubMed PMID: 17388664]
[54]
Shane AL, Mody RK, Crump JA, Tarr PI, Steiner TS, Kotloff K, Langley JM, Wanke C, Warren CA, Cheng AC, Cantey J, Pickering LK. 2017 Infectious Diseases Society of America Clinical Practice Guidelines for the Diagnosis and Management of Infectious Diarrhea. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2017 Nov 29:65(12):e45-e80. doi: 10.1093/cid/cix669. Epub
[PubMed PMID: 29053792]
Level 1 (high-level) evidence
[55]
Hsiao A, Hall AH, Mogasale V, Quentin W. The health economics of cholera: A systematic review. Vaccine. 2018 Jul 16:36(30):4404-4424. doi: 10.1016/j.vaccine.2018.05.120. Epub 2018 Jun 12
[PubMed PMID: 29907482]
[56]
Hsiao A, Desai SN, Mogasale V, Excler JL, Digilio L. Lessons learnt from 12 oral cholera vaccine campaigns in resource-poor settings. Bulletin of the World Health Organization. 2017 Apr 1:95(4):303-312. doi: 10.2471/BLT.16.175166. Epub 2017 Feb 21
[PubMed PMID: 28479625]
[57]
Schwerdtle P, Onekon CK, Recoche K. A Quantitative Systematic Review and Meta-Analysis of the Effectiveness of Oral Cholera Vaccine as a Reactive Measure in Cholera Outbreaks. Prehospital and disaster medicine. 2018 Feb:33(1):2-6. doi: 10.1017/S1049023X17007166. Epub 2018 Jan 10
[PubMed PMID: 29317005]
[58]
Desai SN, Pezzoli L, Alberti KP, Martin S, Costa A, Perea W, Legros D. Achievements and challenges for the use of killed oral cholera vaccines in the global stockpile era. Human vaccines & immunotherapeutics. 2017 Mar 4:13(3):579-587. doi: 10.1080/21645515.2016.1245250. Epub
[PubMed PMID: 27813703]
[59]
Poncin M, Zulu G, Voute C, Ferreras E, Muleya CM, Malama K, Pezzoli L, Mufunda J, Robert H, Uzzeni F, Luquero FJ, Chizema E, Ciglenecki I. Implementation research: reactive mass vaccination with single-dose oral cholera vaccine, Zambia. Bulletin of the World Health Organization. 2018 Feb 1:96(2):86-93. doi: 10.2471/BLT.16.189241. Epub 2017 Oct 19
[PubMed PMID: 29403111]
[60]
Cho JY, Liu R, Macbeth JC, Hsiao A. The Interface of Vibrio cholerae and the Gut Microbiome. Gut microbes. 2021 Jan-Dec:13(1):1937015. doi: 10.1080/19490976.2021.1937015. Epub
[PubMed PMID: 34180341]
[61]
. Responding to the global cholera pandemic. Bulletin of the World Health Organization. 2023 Apr 1:101(4):234-235. doi: 10.2471/BLT.23.020423. Epub
[PubMed PMID: 37008267]
[62]
Taylor DL, Kahawita TM, Cairncross S, Ensink JH. The Impact of Water, Sanitation and Hygiene Interventions to Control Cholera: A Systematic Review. PloS one. 2015:10(8):e0135676. doi: 10.1371/journal.pone.0135676. Epub 2015 Aug 18
[PubMed PMID: 26284367]
[63]
Lund AJ, Keys HM, Leventhal S, Foster JW, Freeman MC. Prevalence of cholera risk factors between migrant Haitians and Dominicans in the Dominican Republic. Revista panamericana de salud publica = Pan American journal of public health. 2015 Mar:37(3):125-32
[PubMed PMID: 25988248]
[64]
Bwire G, Munier A, Ouedraogo I, Heyerdahl L, Komakech H, Kagirita A, Wood R, Mhlanga R, Njanpop-Lafourcade B, Malimbo M, Makumbi I, Wandawa J, Gessner BD, Orach CG, Mengel MA. Epidemiology of cholera outbreaks and socio-economic characteristics of the communities in the fishing villages of Uganda: 2011-2015. PLoS neglected tropical diseases. 2017 Mar:11(3):e0005407. doi: 10.1371/journal.pntd.0005407. Epub 2017 Mar 13
[PubMed PMID: 28288154]
[65]
Idoga PE, Toycan M, Zayyad MA. Analysis of Factors Contributing to the Spread of Cholera in Developing Countries. The Eurasian journal of medicine. 2019 Jun:51(2):121-127. doi: 10.5152/eurasianjmed.2019.18334. Epub
[PubMed PMID: 31258350]