Structure and Function
Common Bone Markings
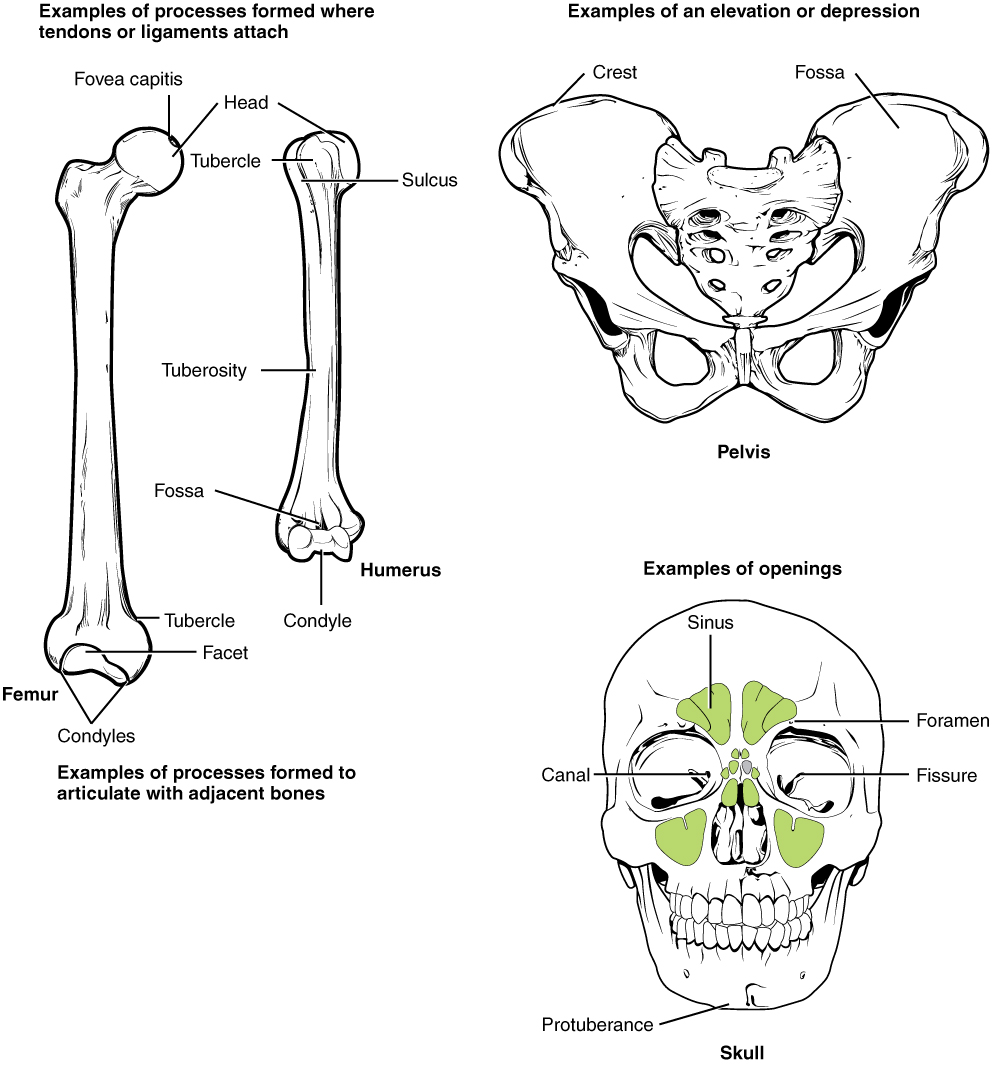
Common bone markings are distinctive features on bone surfaces that serve various anatomical, functional, and developmental roles. These markings provide essential reference points for understanding skeletal structure, identifying specific bones, and comprehending their interactions within the body (see Image. Labeled Bone Markings). The following are common bone markings:
- Angles: Sharp bony angulations that may serve as bony or soft tissue attachments but are often used for precise anatomical description. Examples include the scapula's superior, inferior, and acromial angles and the occiput's superior, inferior, and lateral angles.
- Body: The bone's largest, most prominent segment. Examples include the diaphysis or shaft of long bones like the femur and humerus.
- Condyle: Refers to a large prominence that provides structural support to the overlying hyaline cartilage. Condyles bear the brunt of the force exerted by a muscle about a joint. Examples include the knee, a hinge joint uniting the femoral lateral and medial condyles with the tibial lateral and medial condyles. The occiput also has an occipital condyle that articulates with the atlas (1st cervical vertebra or C1) and accounts for approximately 25° of cervical flexion and extension.[4]
- Crest: A bone edge's raised or prominent part. Crests provide sites for muscle and connective tissue attachments. The iliac crest is found on the ilium.
- Diaphysis: Refers to a long bone's shaft. Examples of long bones include the femur, humerus, and tibia.
- Epicondyle: A prominence superior to a condyle. The epicondyle provides muscle and connective tissue attachment sites. Examples include the femoral and humeral medial and lateral epicondyles.
- Epiphysis: The bone's articulating segment, usually at the bone's proximal and distal poles. The epiphysis typically has a larger diameter than the diaphysis. This segment is critical to bone growth, as it sits adjacent to the physeal line (growth plate).
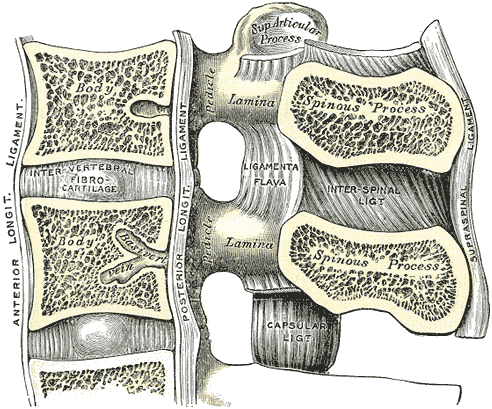
- Facet: A facet is a smooth, flat surface that forms a gliding joint with another flat bone or facet. Examples may be seen in the vertebrae's facet joints, which allow for spinal flexion and extension.
- Fissure: An open slit in a bone that usually houses nerves and blood vessels. Examples include the skull's superior and inferior orbital fissures.[5]
- Foramen: A hole through which nerves and blood vessels pass. Examples include the supraorbital, infraorbital, and mental foramina in the cranium.[6]
- Fossa: A shallow depression on the bone surface, which may receive an articulating bone or act to support soft tissue structures. Examples include the trochlear and the posterior, middle, and anterior cranial fossae.
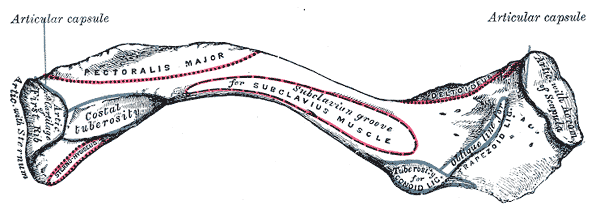
- Groove: A furrow on the bone surface that houses long blood vessel or nerve segments for protection against compression by adjacent structures (see Image. Anterior Surface of Clavicle). Examples include the radial and transverse sinus grooves.
- Head: A rounded, prominent, bony extension that forms part of a joint. The head is separated from the bone shaft by the neck. The head is usually covered in hyaline cartilage and a synovial capsule. This part comprises a bone's main articulating surface in ball-and-socket joints. An example is the femoral head in the hip joint.
- Margin: A flat bone's edge. Margins may be used to define a bone's borders accurately. For example, the part of the temporal bone articulating with the occipital bone is called the "occipital margin" of the temporal bone." Similarly, the part of the occipital bone articulating with the temporal bone is called the occipital bone's "temporal margin."
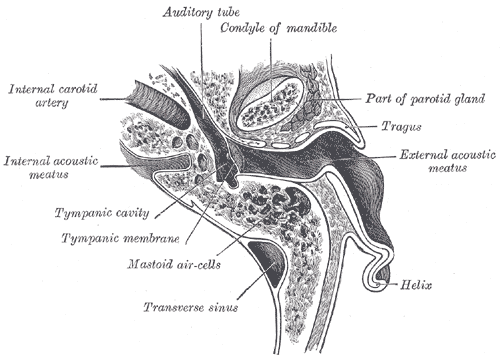
- Meatus: A tube-like channel that extends within the bone, which may provide passage and protection to nerves and vessels. The external and internal acoustic meatus accommodate sound transmission (see Image. External Ear, Horizontal Section).
- Neck: The segment between a bone's head and shaft. This part is often demarcated from the head by the physeal line in pediatric patients and physeal scar (or physeal line remnant) in adults. The neck is often separated into surgical and anatomical necks. The anatomical neck, representing the old epiphyseal plate, is often demarcated by its attachment to capsular ligaments. The surgical neck is often more distal than the anatomical neck and is a commonly fractured location. For example, the humeral anatomical neck runs obliquely from the greater tuberosity to the humeral head's inferior aspect. The surgical neck runs horizontally and a few centimeters distal to the humeral tuberosities.
- Notch: A bony depression that often, but not always, stabilizes an adjacent articulating bone. The articulating bone slides into and out of the notch, which guides the joint's range of motion. Examples include the ulna's trochlear and radial notches and the suprasternal and mandibular notches.
- Ramus: The curved part of a bone that gives structural support to the rest of the bone. Examples include the superior and inferior pubic and mandibular rami.
- Sinus: A hollow cavity housing air, fluid, or blood. Examples include paranasal and dural venous sinuses.
- Spinous process: A raised, sharp bony elevation where muscles and connective tissues attach. Spinous processes are more pronounced than other bony processes (see Image. Lumbar Vertebral Anatomy).
- Trochanter: A large prominence on one side of a bone. Some of the largest muscle groups and most dense connective tissues attach to the trochanter. The most notable examples are the femur's greater and lesser trochanters.
- Tuberosity: A moderate prominence where muscles and connective tissues attach. Tuberosities function similarly to trochanters. Examples include the tibial, deltoid, and ischial tuberosities.
- Tubercle: A small, rounded prominence where connective tissues attach. Examples include the greater and lesser humeral tubercles.
Bone Markings in the Upper Limb
The upper limb is involved in a wide range of movements essential for daily activities and physical function. Thus, the upper limb's bone markings are particularly relevant for clinical and anatomical study.
Scapula
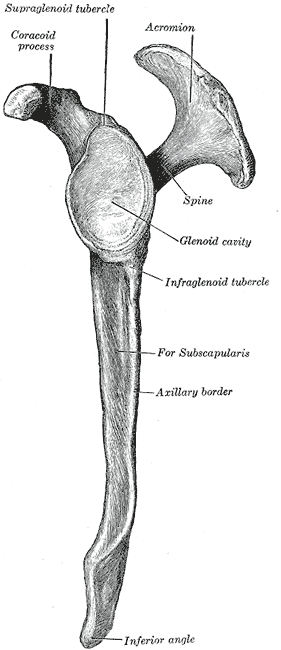
The scapula serves as the upper limb's mobile platform. One can think of this bone as a massive construction crane with jacks that anchor the cab to the ground, like how muscles and connective tissues attach the scapula to the body. The crane also has a long, mobile arm, resembling the upper limb. The scapula has medial, lateral, and superior borders. The inferior pole is the junction of the medial and lateral borders.
The dorsal scapular surface contains the bone's prominent spine. The trapezius inserts on the scapular spine. The deltoid muscle arises from the scapular spine's lateral aspect, the acromion, and the lateral clavicle.[7] The supraspinous fossa above the scapular spine is the supraspinatus muscle's origin. This muscle inserts on the greater humeral tubercle's “S” facet (see below). The infraspinous fossa below the scapular spine is where the infraspinatus muscle originates. This muscle inserts on the “I” (middle) facet of the greater humeral tubercle.
The acromion (acromial process) lies at the scapular spine's lateral end. The acromial process is one of the deltoid muscle's proximal insertion sites. The deltoid is a triangular muscle named after the capital Greek letter delta. The scapula's medial border is an insertion site for the rhomboid minor and major muscles. The teres minor originates from the scapula's lateral border, while the teres major arises from the inferior scapular angle.
The scapula's anterior surface contains the prominent coracoid process, which resembles a crow’s beak. This process acts as a pectoralis minor attachment point. The coracoid process is also where the biceps brachii's short head and coracobrachialis muscles arise. The subscapular fossa houses the subscapularis' proximal insertion point. The subscapularis distally inserts on the lesser humeral tubercle.
The glenoid fossa receives the humeral head at the scapulohumeral articulation or shoulder joint (see Image. Scapula, Lateral View).[8]
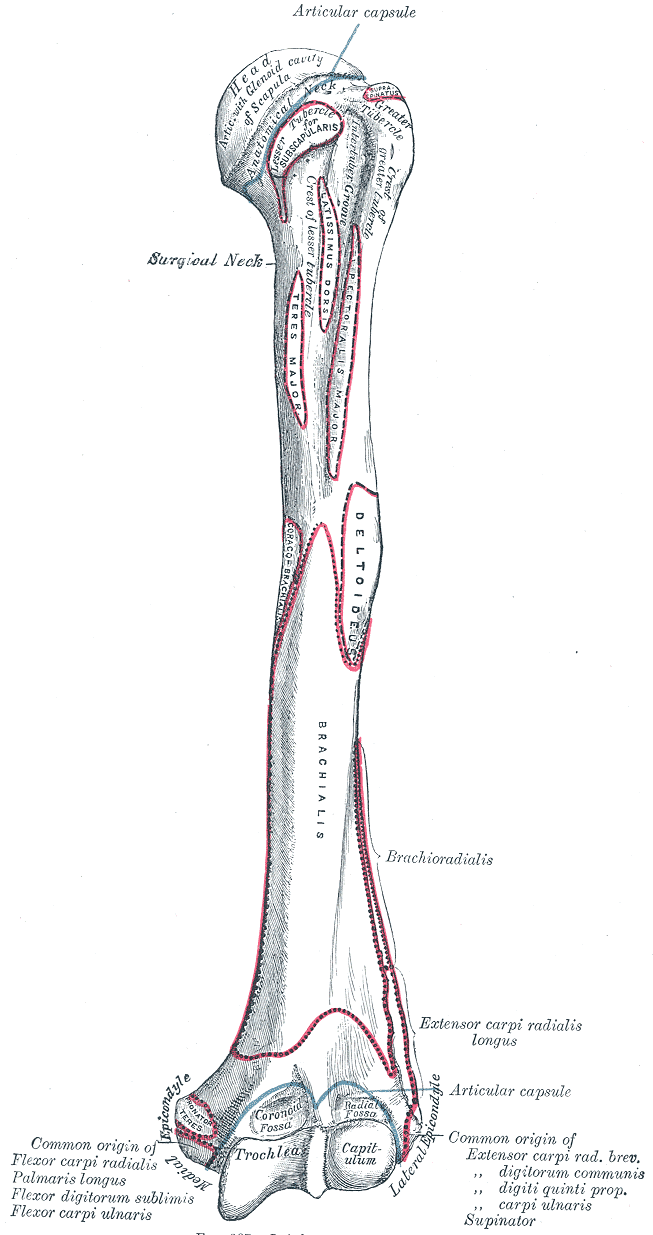
Humerus
The humerus is the arm bone (see Image. Upper Arm Anatomy). The greater and lesser tubercles lie on the superior aspect of this bone. The greater tubercle is located laterally and has 3 prominent facets termed the “S,” “I,” and “T” facets. The superior or "S" facet serves as the distal insertion site for the supraspinatus muscle, which initiates arm abduction. The muscle acts as the primary arm abductor for the first 15° to 20° of abduction. The deltoid becomes the primary abductor beyond this angle. The middle or "I" facet houses the infraspinatus insertion site. This muscle is a lateral arm rotator. The lower or "T" facet contains the teres minor insertion point. The teres minor is another lateral arm rotator.[9]
The lesser humeral tubercle contains the subscapularis muscle's distal insertion point. The subscapularis is a major arm adductor, preventing arm dislocation at the shoulder.[9]
The humeral midshaft's lateral surface exhibits the deltoid tuberosity, the deltoid insertion site. This muscle abducts the arm beyond the first 15° to 20°. The deltoid's anterior fibers rotate the arm medially, while the posterior fibers laterally rotate the arm.[10]
The humeral midshaft's posterior aspect demonstrates the radial spiral groove, which ordinarily lies between the triceps brachii's lateral and medial heads. This groove transmits the radial nerve and profunda brachii artery.
The arm bone's inferior aspect contains the lateral and medial epicondyles. The lateral supracondylar ridge, which contains the proximal insertion point of the brachioradialis and extensor carpi radialis longus, flows into the lateral epicondyle. The lateral epicondyle is a bony prominence where the extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris originate.
The olecranon fossa lies on the arm bone's posterior aspect between the lateral and medial epicondyles. This region receives the ulna's olecranon process at the elbow joint. The distal humeral articulating surfaces include the laterally located capitulum (Latin for "little head") and the trochlea (Greek for "pulley").[11]
Radius
The head comprises the proximal radial end and articulates with the capitulum, allowing rotation for supination (palm up) and pronation (palm down). This mobility, while beneficial, makes the radius susceptible to dislocation, as in "nursemaid's elbow." The radial tuberosity serves as an insertion site for the biceps brachii. The radial shaft leads to the large styloid process at the distal end, where the brachioradialis muscle inserts. The radius articulates with the scaphoid and lunate at the radiocarpal joint.[12]
Ulna
The proximal ulnar end contains the coronoid process, which articulates with the humeral trochlea. This articulation is strong, only permitting flexion and extension. The ulnar tuberosity is where the brachialis muscle distally inserts. This muscle is a pure forearm flexor.[13] The distally located ulnar head articulates with the radius.
Wrist bones, metacarpals, and fingers
The 8 carpal bones are divided into proximal and distal rows. The proximal wrist bones articulate with the radius. The proximal row includes the scaphoid, which resembles the prow of a ship and articulates with the trapezium distally. The trapezium then connects to the 1st metacarpal bone that supports the thumb. Moving from lateral to medial, the proximal row continues with the lunate (resembling the moon), triquetrum (which has 3 corners), and the rounded pisiform. The pisiform can be palpated on the hand's anterior aspect. This bone moves with hand motion, confirming its location within the wrist rather than the forearm.
The distal carpal row starts with the laterally located trapezium (which resembles a 4-sided figure with 2 parallel sides), articulating with the thumb and index finger metacarpals. Medial to the trapezium is the trapezoid, shaped similarly to the trapezium, and capitate, the largest wrist bone. The hamate is medially located and features a prominent hook. The Guyon canal is the space between the pisiform and the hamate's hook that transmits the ulnar nerve. A hamate hook fracture can damage this nerve.
The 14 finger bones are known as the phalanges, a term derived from the military formation "phalanx." Each finger has 3 phalanges, except the thumb, which has 2. Finger movements include flexion (forward), extension (backward), abduction (finger separation), and adduction (fingers coming together). Metacarpal bones, 1 for each finger, connect the wrist bones to the fingers. The thumb's carpometacarpal articulation is rotated 90° compared to the other fingers, allowing flexion and extension along the plane of the hand. Abduction leads the thumb away from the palm, while adduction brings it toward the palm.[14]
Bone Markings in the Lower Limb
The lower limb bone markings serve as attachment sites for muscles, ligaments, and tendons, influencing joint stability and function important for weight-bearing and ambulation. Lower limb bone markings aid healthcare professionals in diagnosing injuries, planning surgical procedures, and guiding rehabilitation efforts.
Hip bone
The hip bone (innominate bone), consisting of the ilium (superior), ischium (posteroinferior), and pubis (anteroinferior), forms a sturdy basin that supports the trunk and provides attachment for lower limb muscles and ligaments. The iliac crest is located along the superior iliac border and acts as a thoracoabdominopelvic, hip, and thigh muscle attachment site. The acetabulum is a deep socket formed by the fusion of the 3 hip bones that receives the femoral head to form the hip joint. The greater sciatic notch on the ilium's posterior aspect allows for the sciatic nerve's passage. The inferoposteriorly located ischial tuberosity is an important weight-bearing structure that also acts as a hip and thigh muscle attachment site. The pubic symphysis is a fibrocartilaginous joint (secondary cartilaginous joint) that unites the pubic bones and stabilizes the hip.[15]
Femur
As the body's longest and strongest bone, the femur (thigh bone) transmits the upper body's weight to the lower limbs when standing and ambulating. The proximal femoral end features the femoral head, articulating with the hip's acetabulum to form the hip joint. The femoral neck unites the head to the shaft and is a common fracture site, particularly in older individuals. The greater and lesser trochanters act as attachment points for hip and thigh muscles. The intertrochanteric line and crest provide additional hip and thigh muscle attachment areas. The linea aspera is a ridge on the posterior surface of the femoral diaphysis that acts as an attachment site for various muscles, including the adductor magnus and vastus lateralis.[16]
Patella
The patella (kneecap) is a sesamoid bone embedded within the quadriceps tendon. This bone forms crucial articulations primarily with the femur and tibia, which are vital in knee stability and motion. The patella glides over the femoral condyles at the patellofemoral joint during flexion and extension.[17]
Tibia
The tibia is the stronger and larger of the 2 leg bones. This bone significantly contributes to weight-bearing and serves as an attachment site for thigh, leg, and extrinsic foot muscles. The tibia's proximal end features medial and lateral condyles, which unite with the femoral condyles to form the knee joint. The tibial tuberosity on the anterior diaphyseal surface provides an attachment site for the patellar ligament. The tibial shaft is relatively flat on its anterior surface, essential for protecting the underlying structures, including the anterior tibial vessels, deep fibular nerve, and leg extensor tendons. The medial malleolus at the distal end forms the prominence of the ankle's inner aspect and provides stability to the ankle joint.[18]
Fibula
The fibula is thinner and more slender than the tibia. This bone does not bear weight, though it provides stability to the ankle joint and is an attachment site for leg and extrinsic foot muscles. The fibular head articulates with the tibia, contributing to the stability of the proximal tibiofibular joint. The lateral malleolus at the fibula's distal end forms the prominence of the ankle's outer aspect and provides additional ankle stability.[19]
Tarsals, metatarsals, and phalanges
The foot consists of multiple bones arranged in intricate arches to support body weight and facilitate movement. The tarsal bones, including the calcaneus, talus, navicular, cuboid, and cuneiforms, form the proximal part of the foot and provide stability and flexibility. The metatarsals, numbered 1 through 5 from medial to lateral, articulate with the tarsal bones proximally and the phalanges distally. The phalanges, similar to those in the hand, consist of proximal, middle, and distal phalanges. The big toe (hallux) has only 2 phalanges. The metatarsophalangeal and interphalangeal joints allow for movement and flexibility during walking and running.[20]
Bone Markings in the Axial Skeleton
The axial skeleton forms the human body's central axis and is comprised of the skull, vertebral column, ribs, and sternum. Numerous bone markings in this region serve diverse anatomical, biomechanical, and clinical functions.
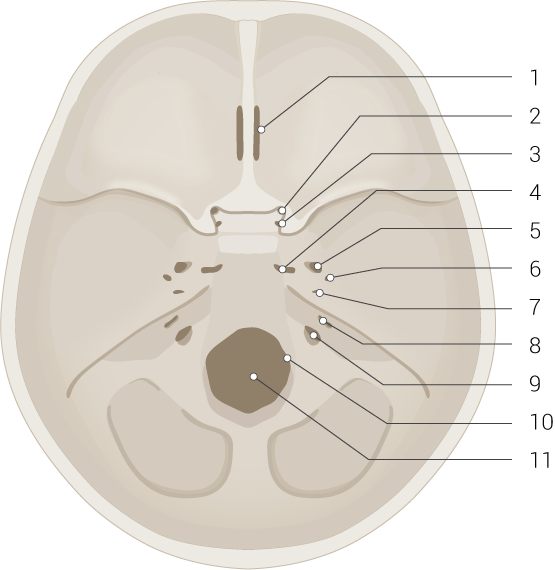
Skull
The craniofacial bones exhibit various markings. The superior orbital fissure lies between the lesser and greater sphenoid wings. The inferior orbital fissure is situated between the maxilla, zygomatic bone, and greater sphenoid wing. The cranial base exhibits various foramina, including the cribriform, anterior and posterior ethmoidal, and jugular foramina (see Image. Skull Base and Foramina). Paranasal sinuses, such as the maxillary sinus, are hollow cavities in craniofacial bones (see Image. Paranasal Sinuses). The transverse sinus groove on the occipital bone's inner surface runs horizontally near the tentorium cerebelli attachment.
The cranial fossae include the anterior, middle, and posterior cranial fossae, which are cranial base depressions supporting the brain, cranial nerves, and head and neck blood vessels. The occipital condyle articulates with the cervical atlas, contributing to the stability and mobility of the head and neck. The temporal bone's external and internal acoustic meatus accommodate sound transmission.
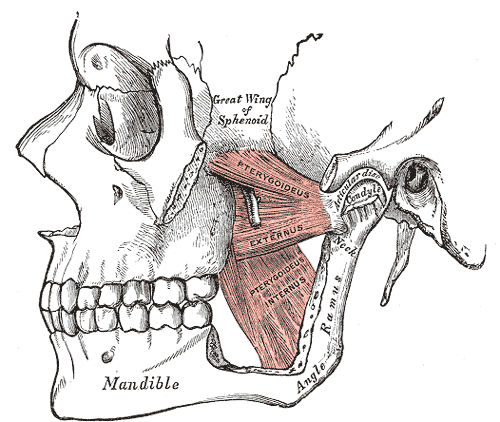
The mandibular body is the bone's horizontal portion that forms the lower jawline. Rami are vertical mandibular extensions on each side, consisting of the ascending ramus and the condylar and coronoid processes. The condylar process connects with the temporal bone to form the temporomandibular joint (see Image. Pterygoids). The coronoid process provides an attachment site for the mastication muscles.
The angle of the mandible is where the mandible body meets the ramus, forming a distinct corner or angle. The mandibular notch (sigmoid notch) is a depression between the condylar and coronoid processes on the ramus' superior border. The mandibular foramen on the ramus' internal surface transmits the inferior alveolar vessels and nerves, supplying the lower teeth and the mandible. The mandibular symphysis is where the 2 halves of the mandible fuse anteriorly at the midline.[21]
Vertebral column
Each vertebra has a body, the main segment that provides structural support. Facet joints between adjacent vertebrae allow spinal flexion and extension. Intervertebral foramina enable thoracic nerves and blood vessels to pass between adjacent vertebrae. The vertebral neck is the segment between the body and vertebral processes. Intervertebral notches on the superior and inferior aspects of adjacent vertebrae form the intervertebral foramina, where spinal nerves traverse from the cord to the body. Spinous processes are raised bony elevations where trunk muscles and connective tissues attach.[22]
Ribs
The rib has superior and inferior angles where the rib curves. These structures also serve as trunk muscle and ligament attachment sites. Ribs also have superior and inferior crests, which are raised edges for thoracic muscle and connective tissue attachment. The body is the rib's main segment. The costal grooves inside the ribs provide passage for intercostal vessels and nerves, supporting thoracic function.
Ribs have facets on their heads that articulate with the thoracic vertebrae, forming the costovertebral joints. The head of the rib is a rounded, prominent extension that articulates with the thoracic vertebrae. Costal margins define rib borders and serve as thoracic muscle attachment sites. The rib's neck is the segment between the head and the body. Costal notches articulate with the vertebrae or sternum. Ribs have articular and nonarticular tubercles, the latter serving as trunk muscle attachment points.[23]
Sternum
The sternomanubrial angle (or sternal angle or angle of Louis) is the junction between the manubrium and sternal body (see Image. Sternum Anatomy). This angle is palpable as a slight elevation and serves as a landmark for locating the 2nd rib and the T4-T5 intervertebral disk. The sternal body (or gladiolus or gladiolus sterni) is the sternum's largest and central segment. The sternal margins provide attachment points for the ribs' costal cartilages. The jugular notch (suprasternal notch) is a U-shaped depression at the sternum's superior aspect, serving as a palpable landmark for anatomical reference and facilitating the identification of cervical structures. Clavicular notches on the manubrium's superior border articulate with the clavicles.[24][25]
Blood Supply and Lymphatics
Blood vessels permeate bone tissue, except in cartilaginous regions like the growth plate. Arteries supply oxygenated blood to bones, while veins carry blood away, connected by capillary networks. Long bones such as the tibia and femur feature various artery types, including the principal nutrient artery, which splits into ascending and descending central arteries, supplying the medulla and cortical layers.[28] Additionally, periosteal and Haversian arteries traverse the bone's outer and cortical surfaces, respectively, with Volkmann arteries acting as bridges between these vessels.[29] Veins exit bones via periosteal veins, and epiphyseal and metaphyseal arteries supply blood to bone ends. Flat bones like cranial bones are perfused primarily by periosteal arteries, while irregular bones like the mandible have complex vascular arrangements.
The bone capillary network fills the marrow cavity, predominantly comprising dense, fenestrated, and branched sinusoidal vessels. Linear columnar vessels predominate in the metaphysis and endosteum, interconnected by loops or arches. These vessels drain into a central vein in long bone diaphyses, with smaller veins branching off to periosteal veins. Type H vessels, expressing markers like endomucin and CD31, exhibit higher oxygen levels and blood velocity due to direct arteriolar connections, influencing tissue microenvironments. Various cell types surrounding blood vessels, like pericytes and stromal cells, show distinct characteristics depending on the vessel type and share similarities with mesenchymal progenitor cells, suggesting a role in tissue repair. These cells contribute to bone lineage during development and adulthood, supporting diverse cellular environments within bone tissue.
Transcortical vessels traverse cortical bone, providing direct arteriovenous connections in the endosteum. The distribution and heterogeneity of perivascular cells in bone contribute to tissue homeostasis and repair. Different cell types associated with specific vessel subtypes, such as Nestin-expressing cells around type H vessels and LepR-expressing cells near type L vessels, exhibit multilineage potential. These cells contribute to bone marrow stroma, hematopoiesis, and adipogenesis, playing crucial roles in bone health and repair. Additionally, recent studies highlight the role of new adipogenic lineage cells called "marrow adipogenic lineage precursors" in maintaining marrow vasculature and modulating bone formation.[30]
Clinical Significance
Uses of Bone Markings
Nearly all medical providers use bony landmarks to approximate injection sites, localize the targeted tissue, or guide medical imaging. Spinous processes are palpated and used as anatomic guides during epidural steroid injections or lumbar punctures (spinal tap). Tibial and femoral condyles are palpated to approximate the meniscal sites during the McMurray test, which evaluates the menisci's structural integrity. Bony landmarks of the elbow are used to orient the operator and locate areas of interest for targeted medical imaging like ultrasound. These applications underscore the importance of these osteological features.
Nursemaid’s Elbow
Nursemaid's elbow, also known as radial head subluxation, typically occurs in young children when a sudden traction force on the extended arm causes the radius to partially dislocate from the annular ligament. The patient holds the affected arm in a flexed and pronated position, demonstrating pain and reluctance to use the arm. The condition can impair arm supination.[35]
Greater Humeral Tubercular Fracture
Fracture of the greater humeral tubercle damages the insertions of the supraspinatus (“S” facet), infraspinatus (“I” facet), and teres minor (“T”) facet. Supraspinatus weakness impairs arm abduction. This condition may be tested by holding the patient’s arm and having them initiate abduction against resistance. The more powerful deltoid muscle can abduct the arm past the supraspinatus' range (15° to 20° degrees). Without testing against resistance, the patient may bump the arm enough to appear to be able to abduct it completely. Having the patient abduct the arm against resistance reveals the deficit. Lateral arm rotation weakness due to infraspinatus and teres minor impairment may be observed. However, the stronger posterior fibers of the deltoid muscle can compensate. Another injury indicator is pain experienced upon palpation of the greater tubercle.[36][37].
Lesser Humeral Tubercular Fracture
Fracture of the lesser tubercle of the humerus may damage the subscapularis insertion. Arm adduction and medial rotation subsequently weaken. Pain often worsens upon lesser tubercle palpation.[38][39][40]
Humeral Surgical Neck Fracture
Fracture of the humeral surgical neck damages the axillary nerve, weakening the deltoid and teres minor. The axillary nerve terminates as the arm's upper lateral cutaneous nerve. Injury to this nerve may cause pain or anesthesia over the proximal lateral arm region.[41][42]
Lateral Epicondylar Fracture
This injury damages the radial nerve, which innervates the forearm and hand extensors. Radial nerve injury produces a wrist drop or the inability to extend the hand. Testing involves flexing the forearm in a pronated position, with the examiner holding the forearm and hand dorsum. The patient is then instructed to extend the fingers against resistance.[43]
Medial Epicondylar Fracture
This condition damages the ulnar nerve, resulting in forearm flexion weakness and radial deviation of the wrist's medial side. A “claw hand” may also develop, with the 3rd and 4th fingers flexed due to impairment of the 3rd and 4th lumbricals and the interossei. Sensory loss over the hand's medial 1-1/2 side may also be observed.[44][45]
Hamate Hook Fracture
Fracture of the hook of the hamate causes swelling in the surrounding soft tissue that can compress the ulnar nerve at the Guyon canal. Muscles that may weaken include the abductor, flexor, and opponens digiti minimi, the 3rd and 4th lumbricals, interossei, and adductor pollicis brevis. Palpation of the pisiform and hook of the hamate bone produces pain. To test adductor pollicis weakness, the patient may be instructed to hold a piece of paper or the examiner's index finger tightly without letting it slip. Ulnar nerve injury weakens this muscle, leading to the inability to maintain the grip and compensatory flexion of the thumb's distal phalanx, known as the Froment sign.[46][47][48]
Scaphoid Fracture
The scaphoid is located in the depths of the anatomical snuffbox, formed by the tendons of the abductor pollicis longus and extensor pollicis longus anteriorly and the tendon of the extensor pollicis longus posteriorly. A scaphoid injury produces pain, tenderness, and bruising over the anatomical snuffbox. Palpation over this area worsens the pain. The injury may not be detected on radiography until a week postinjury. The wrist should be splinted to prevent displacing the fractured scaphoid. Allowing the fractured scaphoid segment to move freely may cause nonunion, which may become permanent due to the area's poor vascularity.[49][50][51]
Femoral Neck Fracture
Fractures of the femoral neck are common in older adults and can lead to significant morbidity and mortality. Other risk factors for femoral neck fractures include female sex, lower body mass index (<18.5), reduced bone mineral density, smoking, poor nutrition, medications, and sedentariness. Complications of these injuries include avascular necrosis, nonunion, malunion, posttraumatic arthritis, and loss of mobility and function.[52][53]
Iliotibial Band Syndrome
The iliotibial band inserts onto the lateral tibial condyle. Repetitive friction over this bony prominence during activities like swimming or cycling can lead to inflammation and lateral knee pain. This condition, known as iliotibial band syndrome, often presents as lateral knee pain aggravated by repetitive flexion and extension.[54]
Jumper's Knee
Patellar tendonitis or jumper's knee involves patellar tendon inflammation. Excessive stress on this attachment site at the tibial tuberosity, such as during repetitive jumping or running, can lead to pain, swelling, and tenderness over the tibial tuberosity.[55]
Medial Tibial Stress Syndrome
Shin splints involve tibial periosteal inflammation, particularly along the medial border where muscles attach. Medial stress syndrome arises from repetitive stress on the tibial attachment sites of leg muscles, eg, the tibialis posterior and soleus, presenting with pain and tenderness along the tibia's medial aspect.[56]
Achilles Tendinopathy
The Achilles tendon insertion onto the calcaneus (heel bone) is vulnerable to inflammation and degeneration, a condition known as Achilles tendonitis. This disorder commonly affects athletes involved in running or jumping sports and can manifest as pain, swelling, and stiffness at the back of the heel.[57]
Atlantoaxial Instability
Various ligaments and bony structures stabilize the atlantoaxial joint (C1-C2 joint), including C2's odontoid process (dens). Pathologies such as rheumatoid arthritis, trauma, or congenital abnormalities can lead to atlantoaxial instability, where excessive movement between C1 and C2 occurs. The condition can result in the compression of the spinal cord or surrounding nerves and produce neurological deficits, neck pain, and potentially life-threatening complications.[58]
Temporal Bone Fracture
The temporal bone contains several notable landmarks, including the mastoid process and external auditory meatus. Temporal bone fractures typically result from significant head trauma, such as motor vehicle crashes or falls from height. These injuries can disrupt the integrity of the middle and inner ear structures, potentially leading to hearing loss, vertigo, facial nerve paralysis (Bell palsy), or cerebrospinal fluid leakage.[59]
Cervical Rib
A cervical rib is an additional rib that arises from C7 and may extend to T1.[60] This anatomical variation can compress nearby nerves and blood vessels, leading to thoracic outlet syndrome. Symptoms include pain, numbness, upper extremity weakness, arm swelling, and discoloration.[61]
Spinous Process Fracture
Trauma or repetitive stress can lead to spinous process fractures. These injuries most frequently affect the vertebral column's thoracic and lumbar regions. Falls, motor vehicle collisions, and sports injuries are the usual causes. Symptoms include localized pain, tenderness, and restricted spinal mobility.[62]
Sternal Fracture
Sternal fractures commonly arise from blunt chest trauma, eg, from motor vehicle accidents or direct blows to the chest. Fractures may involve the manubrium, body, or xiphoid process and may produce severe chest pain, difficulty breathing, and potential damage to underlying structures such as the heart or lungs.[63]