Stentless Autograft/Homograft Aortic Valve Replacement
Stentless Autograft/Homograft Aortic Valve Replacement
Introduction
A valve is a mobile, thin sheet of tissue present in a pathway, and maintains a unidirectional flow through the passage. The heart valves become insufficient, or they get stenosed. Patients with damaged aortic valves are managed with medicines, aortic valve repair, surgical or transcatheter aortic valve replacement.[1][2] Prosthetic heart valves used for replacement of damaged aortic valves are of two types, mechanical and bioprosthetic. Three common types of mechanical heart valves are disc valves, bi-leaflet valves, and ball and cage valves. Bioprosthetic valves are further divided into xenografts (from animals), homografts (from the same species), and autografts (from the same individual). Bioprosthetic valves can be stented on metallic support or can be attached directly to the aorta.[3]
Stent placement reduces the lumen of the aortic valve and is not favorable hemodynamically, but there is no difference in the clinical outcomes of two types of valves.[4] The selection of prosthetic valves depends upon the patient's choice, age, anticoagulation tolerance, risk of valve deterioration, anticoagulation status, future pregnancy plans, etc.[5] Different types of bioprosthetic valves have similar mortality and reoperation outcomes.[6] Transcatheter aortic valve replacement is a comparatively safer option for patients who cannot undergo an open-heart valve replacement procedure.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The aortic valve consists of three cusps that prevent the backflow of blood from the aorta to the left ventricle. Mostly the three cusps have different sizes.[7] Aortic valve insufficiency or stenosis leads to turbulence in the flow of blood and are identified by murmurs. Aortic stenosis leads to a crescendo-decrescendo systolic murmur in the right second intercostal space that radiates to the carotids. Calcification of the aortic valves in old age, chronic rheumatic heart disease, and congenital bicuspid aortic valves are common causes of aortic stenosis.
Aortic stenosis can present with shortness of breath, chest pain, fatigue, dizziness, etc. Aortic regurgitation leads to a diastolic blowing type murmur in the third intercostal space on the left side along the sternal border. Aortic valve calcification, bicuspid valve, rheumatic heart disease, and root dilatation are common causes of regurgitation. Palpitations and shortness of breath are common symptoms of aortic regurgitation.[8] Any damage to the heart valves put them at risk for endocarditis. Characteristic features of endocarditis are fever, pulmonary infarcts, arterial emboli, Janeway lesions, splinter hemorrhages, conjunctival hemorrhages, painful Osler nodes, Roth spots, glomerulonephritis, new-onset heart murmur, and positive blood cultures. Duke criteria are used to assess the probability of endocarditis.[9]
In the Ross procedure, the pulmonary valve of the patient is used to replace the defected aortic valve. The pulmonic valve is replaced with a bovine jugular vein conduit in patients less than six years. Decellular pulmonary homograft is preferred for older patients.[10] Homografts are obtained from cadaveric or brain dead heart donors. The heart valve, along with peri-annular tissue from a donor, is used to replace the valve and close the defect in the peri-annular tissue. Route of coronary arteries, along with their branches, are kept in mind while doing the valve replacement procedure.[11]
Indications
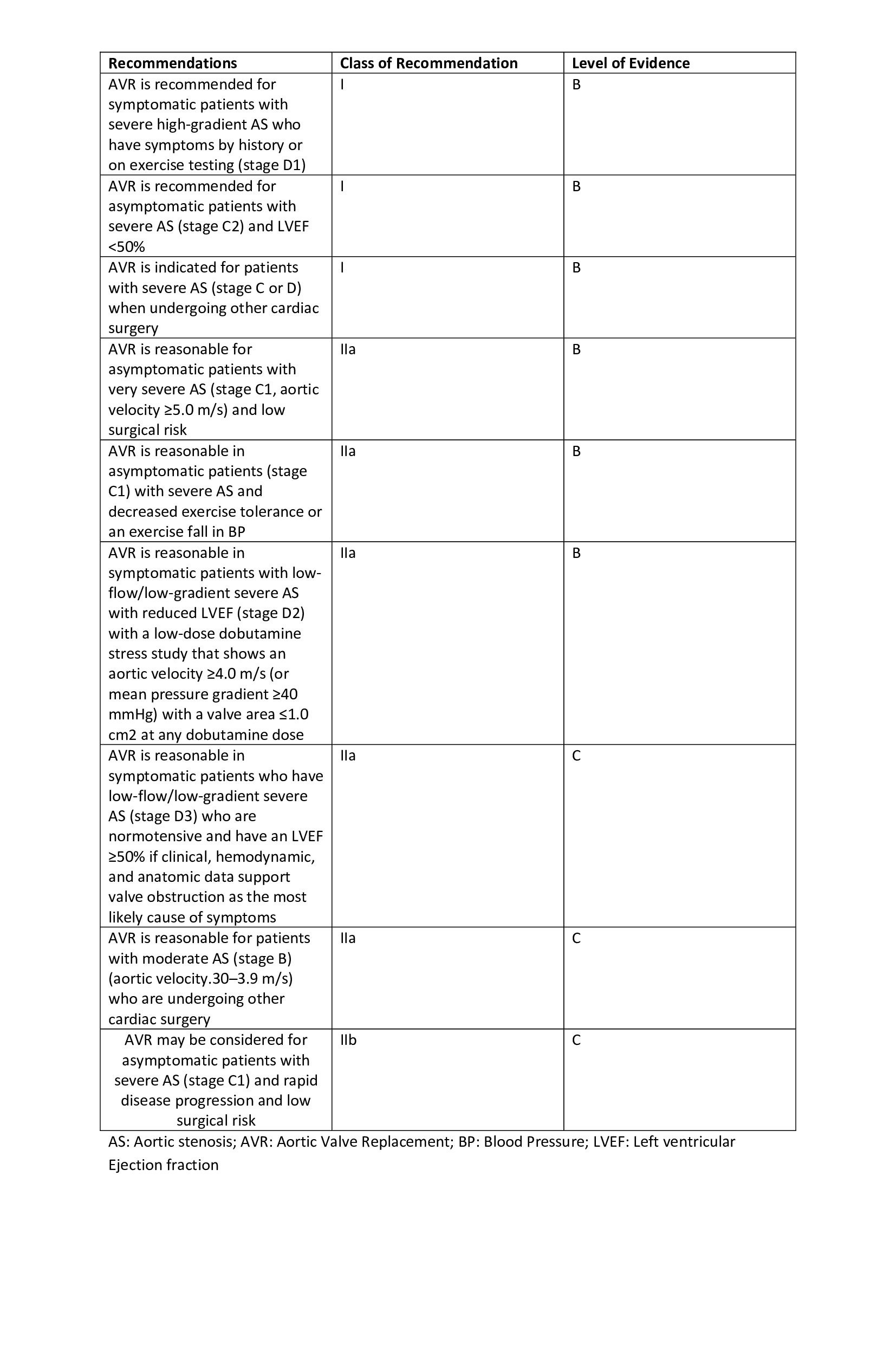
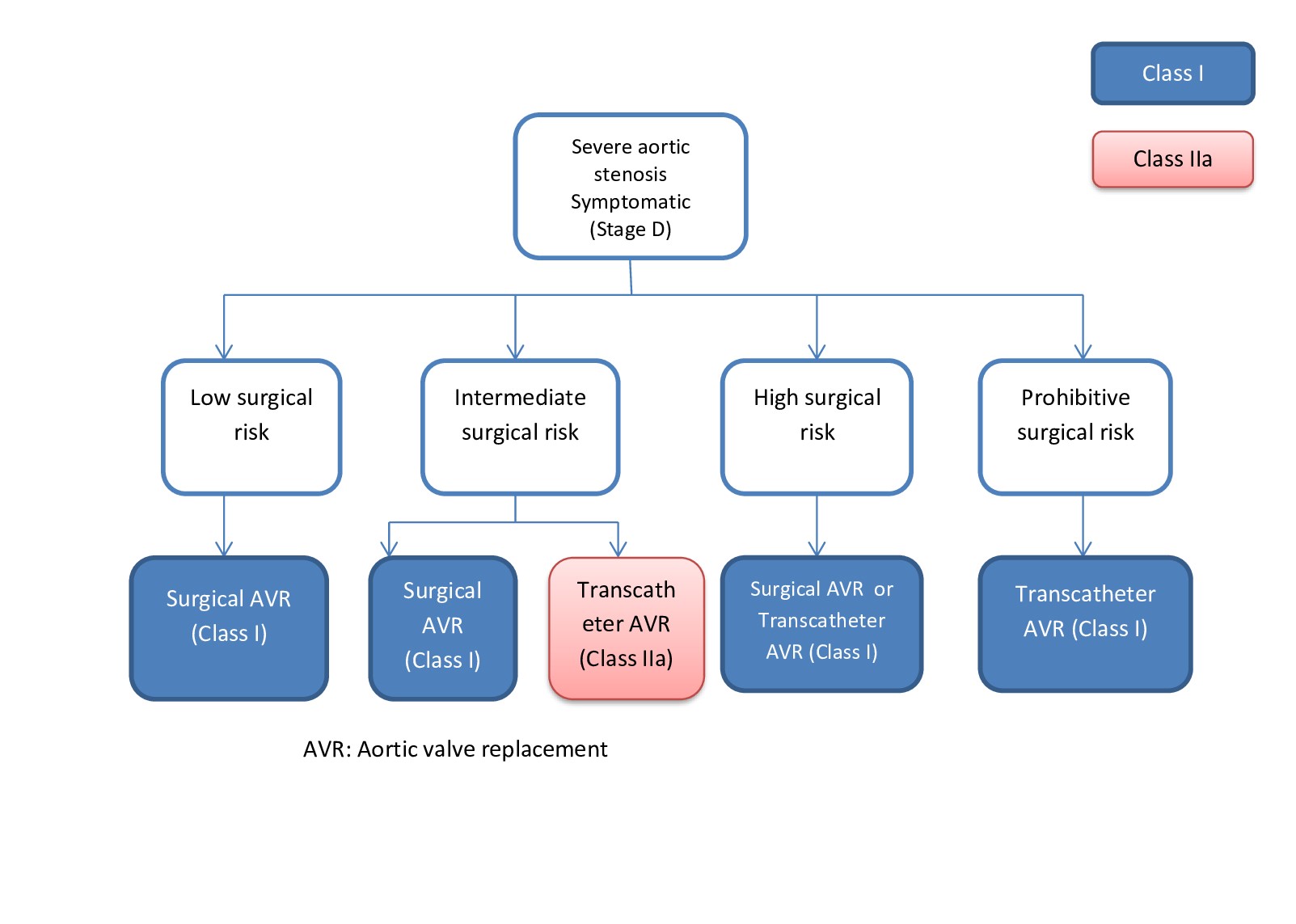
Aortic stenosis is managed symptomatically with beta-blockers (atenolol, nebivolol, etc.), calcium channel blockers (verapamil, diltiazem), or diuretics (furosemide, thiazides, angiotensin-converting enzyme (ACE) inhibitors, etc.). The following are commonly used indications for aortic valve replacement.
- Patients with stage D1 aortic stenosis (symptomatic high grade).
- Patients with stage C2 aortic stenosis (aymptomatic high grade) with < 50% left ventricular ejection fraction.
- Patients with stage C1 aortic stenosis (asymptomatic severe) with low exercise tolerance.
- Patients with stage C1 aortic stenosis (asymptomatic severe) and aortic velocity > 4.5 m/s with low surgical risk.
- Patients with stage C or D aortic stenosis undergoing any other cardiac surgery.[12]
Similarly, for aortic regurgitation, diuretics, and vasodilators (nifedipine, ACE inhibitors, etc.) are used for symptomatic management, the following are common indications for valve replacement,
- Patients with stage D aortic regurgitation (symptomatic severe).
- Patients with stage C2 aortic regurgitation (asymptomatic severe) with < 50% ejection fraction or > 50 mm end-systolic dimension or > 65mm end-diastolic diameter.
- Patients with stage B, C, or D undergoing any other cardiac surgery.[2]
There is insufficient data to indicate a specific type of prosthesis for aortic valve replacement. But the following points favor a bioprosthetic heart valve.
- Contraindications, non-compliance, or refractory to anticoagulant drugs.
- Fully informed patients' desire.
- Patients with mechanical valve thrombosis.
- Low risk of valve redo-operations.
- Future pregnancy plans.
- Age of more than 65 years.[5]
Autograft aortic valve replacement is done with the Ross procedure. This technique is preferred in children, and young adults as pulmonic valves used as graft have the potential to grow and regenerate and have a lower risk for endocarditis.[10] Homografts are preferred in case of aortic valve endocarditis, especially in case of peri-annular abscess as peri-annular graft tissue can also be used to path these defects. Homografts are also preferred in patients with a history of intravenous (IV) drug abuse and resultant endocarditis as they have a higher risk of reoperations.[11] Xenografts are readily available in all sizes.[13]
Contraindications
Common contraindications for Ross procedure are connective tissue diseases (Marfan disease, Ehlers-Danlos syndrome, etc.) and inflammatory disorders. Inflammatory disorders commonly include rheumatoid arthritis, systemic lupus erythematosus, etc. These diseases frequently involve pulmonary aorta or pulmonary valve. Other contraindications are multiple vessel coronary artery disease, a severe decrease in left ventricular function, or any pulmonary valve pathology. There are no specific contraindications for aortic valve homografts depending upon the availability of donor, and preference of the surgeon and the patient. Young age is considered a relative contraindication for homograft valve replacement.[13][14]
Equipment
Aortic heart valve replacement is done via open median sternotomy. Heart valves are first assessed with echocardiography. Other types of equipment used in the procedure are Hegar dilator (to measure the autografts) and polypropylene sutures (to attach the graft valve). Dacron tube is used in the Ross procedure to extend the pulmonary valve.[15][16]
Personnel
A team consisting of an anesthesiologist, cardiac surgeon, cardiologist, surgery assistants, operation room assistant, a radiologist, and additional staff members is required to perform an aortic heart valve replacement surgery.[17]
Preparation
The main goal of preparation is sterility. Before starting the procedure, the whole chest is shaved and sterilized. The patient is draped based on the institution protocols, and other general anesthesia-related preparations are done. Important landmarks (like jugulum, xiphoid process) are identified and marked before starting the procedure.[17][18]
Technique or Treatment
Aortic valve replacement by Ross procedure is done with median sternotomy and bicaval and aortic cannulation. Cardioplegia is obtained mostly with cold intermittence. Warm reperfusion is done before the aortic clamp is released. Common adventitia between pulmonary root and aorta is dissected to reach muscular infundibulum. Both the aortic and pulmonary valves are inspected first before any extraction. The pulmonary valve is extracted while making sure that the valve is in good shape, and the first septal coronary artery is preserved. The Hegar dilated is then used for the measurement of autograft. The next step is the removal of the diseased valve. The annulus is then measured to match it with the graft. Annuloplasty is done in case of any mismatch. Valve leaflets are then attached to the aorta with the help of polypropylene sutures. After the autograft implantation, the left coronary button is anastomosed first, others later. Then the surgeon performs distal anastomosis of pulmonary graft first and distal anastomosis of aortic graft later. The final part is to secure the proximal portion of the pulmonary graft with a running suture.[16][19]
Homograft aortic valve replacement is also done with a median sternotomy followed by cardioplegia. During the procedure, the surgeon makes sure to remove all the infected tissue along with a damaged aortic valve. Debridement procedure may lead to mitro-aortic junction defect. Anterior mitral leaflet or a part of a leaflet from the graft is used to fil this defect. Then the atrium is sutured along with a pericardial patch if needed.[15]
Complications
About 30% of patients face pulmonary autograft dilatation after the Ross procedure. After the Ross procedure, patients with age < 25years almost always require autograft reintervention at some time in life. For older patients, there is a risk of 32% to 68% for reintervention due to graft valve-related complications. Younger age is also associated with right ventricular outflow tract conduit degeneration. Ross procedure is associated with a comparatively lower number of bleeding, thrombosis, and endocarditis related complications as compared to other types of graft replacements. Lesser number of early and late mortality is associated with this procedure.[20][21]
Homograft aortic valve replacement may lead to early mortality, but the incidence is low. Structural deterioration of graft may occur in about 20 years due to the rupture of graft leaflet, calcification of graft valve, or poor coaptation of leaflets. Early reinfection rate is low, but late infections may occur in 4 months to 5 years. Valve deterioration and reinfections may lead to reinterventions.[22]
Clinical Significance
Ross procedure was first described in 1947. It has the advantage that surgeons use viable autograft that can grow, regenerate, and has a low risk of endocarditis. These characteristics make them ideal for pediatric and young patients. Pediatric Ross procedure has lower mortality and a lower rate of reinterventions as compared to other graft procedures.[10] Homograft aortic valve replacement is a complex procedure but has good clinical outcomes in adults and patients with future pregnancy plans.[23]
Enhancing Healthcare Team Outcomes
The aortic valve replacement procedure is major cardiac surgery. There should not be any communication gap between the team members. A thorough assessment of the patient before, during, and after the procedure leads to better outcomes. Negligence can lead to preventable adverse events. Appropriate care provides better results after heart valve replacement. Phase 2 randomized clinical trial has shown better VO2 max (maximum oxygen utilized during exercise) in patients with cardiac rehabilitation.[24] [Level 2]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Fleisher LA, Jneid H, Mack MJ, McLeod CJ, O'Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017 Jun 20:135(25):e1159-e1195. doi: 10.1161/CIR.0000000000000503. Epub 2017 Mar 15 [PubMed PMID: 28298458]
Level 1 (high-level) evidenceNishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O'Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM 3rd, Thomas JD, ACC/AHA Task Force Members. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014 Jun 10:129(23):2440-92. doi: 10.1161/CIR.0000000000000029. Epub 2014 Mar 3 [PubMed PMID: 24589852]
Level 1 (high-level) evidenceMathew P, Kanmanthareddy A. Prosthetic Heart Valve. StatPearls. 2024 Jan:(): [PubMed PMID: 30725672]
Shultz BN, Timek T, Davis AT, Heiser J, Murphy E, Willekes C, Hooker R. A propensity matched analysis of outcomes and long term survival in stented versus stentless valves. Journal of cardiothoracic surgery. 2017 May 31:12(1):45. doi: 10.1186/s13019-017-0608-2. Epub 2017 May 31 [PubMed PMID: 28569201]
Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Muñoz D, Rosenhek R, Sjögren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL, ESC Scientific Document Group. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. European heart journal. 2017 Sep 21:38(36):2739-2791. doi: 10.1093/eurheartj/ehx391. Epub [PubMed PMID: 28886619]
Dagenais F, Cartier P, Voisine P, Desaulniers D, Perron J, Baillot R, Raymond G, Métras J, Doyle D, Mathieu P. Which biologic valve should we select for the 45- to 65-year-old age group requiring aortic valve replacement? The Journal of thoracic and cardiovascular surgery. 2005 May:129(5):1041-9 [PubMed PMID: 15867778]
Silver MA, Roberts WC. Detailed anatomy of the normally functioning aortic valve in hearts of normal and increased weight. The American journal of cardiology. 1985 Feb 1:55(4):454-61 [PubMed PMID: 3155899]
Thomas SL, Heaton J, Makaryus AN. Physiology, Cardiovascular Murmurs. StatPearls. 2024 Jan:(): [PubMed PMID: 30247833]
Topan A, Carstina D, Slavcovici A, Rancea R, Capalneanu R, Lupse M. Assesment of the Duke criteria for the diagnosis of infective endocarditis after twenty-years. An analysis of 241 cases. Clujul medical (1957). 2015:88(3):321-6. doi: 10.15386/cjmed-469. Epub 2015 Jul 1 [PubMed PMID: 26609264]
Level 3 (low-level) evidenceHerrmann JL, Stram AR, Brown JW. Ross Procedure: How to Do It and How to Teach It. World journal for pediatric & congenital heart surgery. 2019 Sep:10(5):624-627. doi: 10.1177/2150135119852324. Epub [PubMed PMID: 31496411]
Byrne JG, Rezai K, Sanchez JA, Bernstein RA, Okum E, Leacche M, Balaguer JM, Prabhakaran S, Bridges CR, Higgins RS. Surgical management of endocarditis: the society of thoracic surgeons clinical practice guideline. The Annals of thoracic surgery. 2011 Jun:91(6):2012-9. doi: 10.1016/j.athoracsur.2011.01.106. Epub [PubMed PMID: 21620012]
Level 1 (high-level) evidenceNishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O'Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM 3rd, Thomas JD, American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014 Jun 10:63(22):2438-88. doi: 10.1016/j.jacc.2014.02.537. Epub 2014 Mar 3 [PubMed PMID: 24603192]
Level 1 (high-level) evidenceLuciani GB, Santini F, Mazzucco A. Autografts, homografts, and xenografts: overview on stentless aortic valve surgery. Journal of cardiovascular medicine (Hagerstown, Md.). 2007 Feb:8(2):91-6 [PubMed PMID: 17299289]
Level 3 (low-level) evidenceOury JH. Clinical aspects of the Ross procedure: indications and contraindications. Seminars in thoracic and cardiovascular surgery. 1996 Oct:8(4):328-35 [PubMed PMID: 8899918]
Solari S, Mastrobuoni S, De Kerchove L, Navarra E, Astarci P, Noirhomme P, Poncelet A, Jashari R, Rubay J, El Khoury G. Over 20 years experience with aortic homograft in aortic valve replacement during acute infective endocarditis. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2016 Dec:50(6):1158-1164. doi: 10.1093/ejcts/ezw175. Epub 2016 May 26 [PubMed PMID: 27229671]
Concha M, Aranda PJ, Casares J, Merino C, Alados P, Muñoz I, Gonzalez JR, Ribes R, Villalba R. The Ross procedure. Journal of cardiac surgery. 2004 Sep-Oct:19(5):401-9 [PubMed PMID: 15383050]
Brown KN, Kanmanthareddy A. Ross Procedure for Aortic Valve Replacement. StatPearls. 2024 Jan:(): [PubMed PMID: 30725934]
Reser D, Caliskan E, Tolboom H, Guidotti A, Maisano F. Median sternotomy. Multimedia manual of cardiothoracic surgery : MMCTS. 2015:2015():. pii: mmv017. doi: 10.1093/mmcts/mmv017. Epub 2015 Jul 17 [PubMed PMID: 26188337]
Conklin LD, Reardon MJ. Technical aspects of the Ross procedure. Texas Heart Institute journal. 2001:28(3):186-9 [PubMed PMID: 11678251]
Berdajs D. Ross procedure for everyone. Swiss medical weekly. 2012:142():w13641. doi: 10.4414/smw.2012.13641. Epub 2012 Jul 23 [PubMed PMID: 22826114]
Etnel JRG, Grashuis P, Huygens SA, Pekbay B, Papageorgiou G, Helbing WA, Roos-Hesselink JW, Bogers AJJC, Mokhles MM, Takkenberg JJM. The Ross Procedure: A Systematic Review, Meta-Analysis, and Microsimulation. Circulation. Cardiovascular quality and outcomes. 2018 Dec:11(12):e004748. doi: 10.1161/CIRCOUTCOMES.118.004748. Epub [PubMed PMID: 30562065]
Level 2 (mid-level) evidenceFukushima S, Tesar PJ, Pearse B, Jalali H, Sparks L, Fraser JF, Pohlner PG. Long-term clinical outcomes after aortic valve replacement using cryopreserved aortic allograft. The Journal of thoracic and cardiovascular surgery. 2014 Jul:148(1):65-72.e2. doi: 10.1016/j.jtcvs.2013.07.038. Epub 2013 Sep 8 [PubMed PMID: 24021951]
Level 2 (mid-level) evidenceNappi F, Nenna A, Petitti T, Spadaccio C, Gambardella I, Lusini M, Chello M, Acar C. Long-term outcome of cryopreserved allograft for aortic valve replacement. The Journal of thoracic and cardiovascular surgery. 2018 Oct:156(4):1357-1365.e6. doi: 10.1016/j.jtcvs.2018.04.040. Epub 2018 Apr 18 [PubMed PMID: 29759737]
Sibilitz KL, Berg SK, Rasmussen TB, Risom SS, Thygesen LC, Tang L, Hansen TB, Johansen PP, Gluud C, Lindschou J, Schmid JP, Hassager C, Køber L, Taylor RS, Zwisler AD. Cardiac rehabilitation increases physical capacity but not mental health after heart valve surgery: a randomised clinical trial. Heart (British Cardiac Society). 2016 Dec 15:102(24):1995-2003. doi: 10.1136/heartjnl-2016-309414. Epub 2016 Aug 4 [PubMed PMID: 27492941]
Level 1 (high-level) evidenceYokoyama Y, Kuno T, Toyoda N, Fujisaki T, Takagi H, Itagaki S, Ibrahim M, Ouzounian M, El-Hamamsy I, Fukuhara S. Ross Procedure Versus Mechanical Versus Bioprosthetic Aortic Valve Replacement: A Network Meta-Analysis. Journal of the American Heart Association. 2023 Jan 3:12(1):e8066. doi: 10.1161/JAHA.122.027715. Epub 2022 Dec 24 [PubMed PMID: 36565200]
Level 1 (high-level) evidenceAndreeva A, Coti I, Werner P, Scherzer S, Kocher A, Laufer G, Andreas M. Aortic Valve Replacement in Adult Patients with Decellularized Homografts: A Single-Center Experience. Journal of clinical medicine. 2023 Oct 24:12(21):. doi: 10.3390/jcm12216713. Epub 2023 Oct 24 [PubMed PMID: 37959179]
Helder MR, Kouchoukos NT, Zehr K, Dearani JA, Maleszewski JJ, Leduc C, Heins CN, Schaff HV. Late durability of decellularized allografts for aortic valve replacement: A word of caution. The Journal of thoracic and cardiovascular surgery. 2016 Oct:152(4):1197-9. doi: 10.1016/j.jtcvs.2016.03.050. Epub 2016 Mar 31 [PubMed PMID: 27131847]
Coti I, Wenda S, Andreeva A, Kocher A, Laufer G, Fischer G, Andreas M. Donor-specific HLA antibodies after fresh decellularized vs cryopreserved native allograft implantation. HLA. 2020 Nov:96(5):580-588. doi: 10.1111/tan.14077. Epub 2020 Oct 13 [PubMed PMID: 32975376]
Skillington PD, Mokhles MM, Takkenberg JJ, Larobina M, O'Keefe M, Wynne R, Tatoulis J. The Ross procedure using autologous support of the pulmonary autograft: techniques and late results. The Journal of thoracic and cardiovascular surgery. 2015 Feb:149(2 Suppl):S46-52. doi: 10.1016/j.jtcvs.2014.08.068. Epub 2014 Sep 17 [PubMed PMID: 25439787]