Introduction
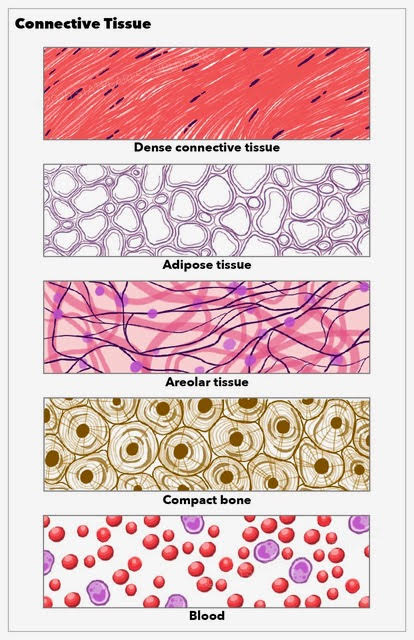
Connective tissue is one of the basic tissue types of the body. As its name implies, "connective tissue" refers to several body tissues that connect, support, and help bind other tissues. While the various connective tissues of the body are diverse, they share numerous structural and functional features that explain why they are subsumed into a single tissue category. Connective tissue can be broken down into two primary categories: connective tissue proper and specialized connective tissue. Connective tissue proper is further subdivided into loose and dense connective tissues. Specialized connective tissues are diverse as they comprise varying specialized cells and ground substances. Specialized connective tissues include adipose, cartilage, bone, blood, and reticular tissues. See Image. Connective Tissue.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Connective tissue contributes to numerous body functions, including supporting organs and cells, transporting nutrients and wastes, defending against pathogens, storing fat, and repairing damaged tissues (see Image. Transverse Section of the Ureter). Connective tissue is composed primarily of an extracellular matrix and a limited number of cells. Most connective tissues are composed of ground substances, fibers, and cells, although blood and lymph are specialized fluid connective tissues without fiber.
Connective tissue is largely organized into subcategories based on its nonliving components. While numerous subcategorizations are published in the literature, connective tissue can be organized into two main types: connective tissue proper and specialized connective tissue.
Connective Tissue Proper
Connective tissue proper includes both loose (or areolar) connective tissue and dense connective tissue. Loose connective tissue previously included areolar, reticular, and adipose tissues, although this system has been revised only to include areolar tissue. Loose connective tissue generally holds organs, anatomic structures, and tissues in place. The extracellular matrix is the most significant feature of loose connective tissue with large spaces between fibers. Dense connective tissue proper is composed of a higher density of fibers, which may be regular (with parallel fibers such as that of tendons and ligaments) or irregular (with multidirectional fibers such as that of the pericardium), or elastic (with significant embedded elastin such as that of arteries).
The extracellular matrix of both loose and dense connective tissue proper is composed of amorphous ground substance, extracellular fluid, and collagen and elastic fibers. The amorphous ground substance is a gelatinous material surrounding the fibers and permitting extracellular fluid to diffuse through. The collagen and elastic fibers of connective tissue proper are histologically distinguishable as three fiber types: collagen, reticular, and elastic fibers.
Collagen fibers form approximately 20-25% of the protein content of humans. They are nonelastic and have variable bundle thicknesses. They are made up of closely packed thin collagen fibrils that run a wavy course in tissues. These parallel fibrils form bundles with flexible proteoglycans to offer an essential mechanical property. They offer flexible but powerful resistance to pulling force. Specifically, collagen runs in a parallel course in loose connective tissue and then joins to form a larger bundle. They split from each other and join back together at varying locations, creating a three-dimensional meshwork. Dense connective tissue, such as ligaments and tendons, is composed mainly of densely packed collagen fibers.[1]
Reticular fibers are generally recognized as one type of collagen fiber. They are also called argyrophilic fibers, which have a restricted abundance in the human body. They are primarily present in basement epithelial tissue, adipose cells, Schwann and muscle cells, lymphoid tissue, and endothelium of hepatic sinusoids. Under microscopy, these reticular fibers are fine, dark fibrils that are continuous with the college fibers described above. The arrangement of these fibers forms a network that underlies the basal lamina layer. A firm attachment of these fibers to the basal lamina indicates that these fibers, along with the collagen fibers, create a functional and structural unit that supports tissues. The loose arrangement of these fibers also provides space for molecular movement within the extracellular fluid.[1]
Elastic fibers have the characteristic property of elastic recoil; each fiber can be stretched to approximately 150% of its resting length. These fibers are composed of elastin surrounded by fibrillin. Typically, in loose connective tissue, elastin is a loose network. Their organization and distribution depend on the type of tissue. Concentric elastin fibers are present in the vascular wall to help maintain uniform blood pressure. Fibers are also present in distensible and contractible organs such as the lungs and urinary bladder.[1]
Specialized Connective Tissue
Specialized connective tissue includes a variety of distinct tissues with specialized cells and unique ground substances that result in wide-ranging properties. Specialized connective tissues include adipose, cartilage, bone, blood, and lymphatic tissues. These tissues contribute to diverse functions. Adipose tissue is a loose, specialized connective tissue that functions primarily in energy storage and release, temperature insulation, organ protection, and hormone secretion. Cartilage functions as a flexible but strong connective tissue that protects the bones and joints by reducing friction and working as a shock absorber. Bone is a rigid and strong connective tissue with mineralized extracellular components that contribute to numerous body functions, including support, protection of organs, enabling movement, fat and mineral storage, and hematopoiesis.[2] Blood and lymph are considered fluid connective tissues, with their cells circulating in a fluid extracellular matrix. Blood is considered a specialized connective tissue as it connects all systems of the body and transports oxygen, nutrients, and wastes. Lymph is a specialized connective tissue that connects the body systems and primarily functions to maintain fluid levels, transport substances, and participate in the immune response.
Embryology
Embryonic connective tissue is present in the umbilical cord and the embryo. Embryonic connective tissue includes mucoid connective tissue and mesenchyme. Mucoid connective tissue is located within the umbilical cord as Wharton's jelly and is a gelatinous tissue primarily composed of a ground substance with few collagen or reticular fibers.[3] Mesenchyme is a loosely organized embryonic connective tissue with undifferentiated cells that produce most of the tissues of the body. Mesenchyme arises from the mesodermal layer of the trilaminar embryonic disc of the early embryo. As a result, most connective tissues arise from mesoderm. For instance, tendons arise from the somatic mesoderm.
During the development of tendons, inductive signals from nearby sclerotome and myotome cause an upregulation expression of a key transcription factor in tenogenic and ligamentogenic differentiation called scleraxis. Several fibroblast factors, as well as transforming growth factor-beta, have involvement in regulating tendon development. Tendon progenitor cells begin to lay down collagenous fibrils, and these fibrils grow in different directions and begin to form the tendon fascicle. Tendon fibroblasts reside between collagen fibers. A connective tissue layer called the epitenon surrounds these tendon fascicles to form the complete tendon tissue.[4]
Blood Supply and Lymphatics
Different types of connective tissue have considerable variation in blood supply, although most are well vascularized. Cartilage is an exception as it is avascular with no direct blood supply, although chondrocytes within cartilage are supplied by blood via diffusion. Tendons and ligaments are composed mainly of densely packed collagen fibers, which undergo no metabolic activity and do not require a blood supply. While living cells are hidden within the collagen fibers of tendons and ligaments that require a blood supply, their volume is minimal.[5]
Nerves
All peripheral nerve fibers consist of three connective tissue layers, which serve as a protective connective sheath. The epineurium is the outermost layer of dense connective tissue that encloses the entire peripheral nerve. Within the epineurium, there are several nerve fascicles that are individually surrounded by the perineurium. These fascicles are made up of myelinated individual nerve fibers surrounded by endoneurium.[6]
Muscles
Individual muscle cells are grouped to form a fiber. These fibers are further bundled together to form a fascicle, and several of these fascicles get further grouped to create the entire muscle. Connective tissue exists between every muscle cell, fiber, and fascicle. At a molecular level, each muscle cell is connected to other muscle cells by a collagenous basement membrane called an endomysium. The fascicles are surrounded by perimysium, which further connects to the epimysium, which encompasses the entire skeletal muscle and is continuous with the tendon. The collagenous network beginning at the level of the endomysium is continuous with the perimysium and the tendon, which allows for an effective and powerful muscle contraction.[7]
Collagen and elastin compose the dry mass of tendon connective tissue.[8] Tendons are connective tissue structures comprised of a hierarchical arrangement of collagen molecules that arrange into collagen fibrils and then collagen fibers, which can be grouped into primary, secondary, and tertiary bundles.[9] The tendon is surrounded by the epitenon, a fine connective tissue sheath. The complex multidimensional arrangement of the collagen fibers of tendons makes its function possible during the longitudinal, rotational, and transverse forces exerted upon tendons.[9]
Clinical Significance
Given the considerable variation in connective tissue types, numerous pathologies and surgical considerations relate to these tissues. Such conditions include tendon tears, bony fractures, muscular compartment syndromes, cartilaginous injury, surgical disruption, and direct inflammation of connective tissues. In addition, there are five currently identified autoimmune connective tissue diseases: systemic lupus erythematosus, scleroderma, myositis, rheumatoid arthritis, and Sjogren syndrome.[10] In addition, individuals who demonstrate select features of autoimmune diseases without clear antibodies or the full suite of symptoms are said to have undifferentiated connective tissue disease. Other individuals who display symptoms of more than one connective tissue disorder may be diagnosed with overlap syndrome.[10] Beyond these autoimmune diseases, several conditions cause abnormalities in connective tissues due to gene defects. Patients who demonstrate joint involvement are typical in systemic connective tissue disease, which may involve destructive or non-destructive arthritis.[11]
Autoimmune Connective Tissue Disease
Five currently recognized autoimmune connective tissue diseases exist, and each is relatively rare: systemic lupus erythematosus, scleroderma, myositis, rheumatoid arthritis, and Sjogren syndrome. Systemic lupus erythematosus is an autoimmune disease involving the inability to form and the loss of self-tolerance of nuclear autoantigens and immune complexes and causes inflammation of multiple organ systems.[12] Due to an abnormal immune response, patients may present with widely varying serological abnormalities and symptoms that may involve the skin, joints, nervous system, lungs, kidneys, or blood vessels and are more common in female and non-white individuals.[13][12] Scleroderma, or systemic sclerosis, is a rare autoimmune disease that is more common in males and is characterized by autoantibodies, abnormal vascular structures, and fibrosis of the skin and various organs due to excess collagen production.[14]
Myositis is another rare autoimmune disease involving autoantibodies and variable patient presentations involving muscle tissue inflammation.[15] Rheumatoid arthritis (RA) is an autoimmune connective tissue disease that results in chronic inflammation of body tissues, typically the joints, and may result in disability.[16] Sjogren syndrome is a rare autoimmune disease characterized by peri epithelial lymphocyte infiltrates in which patients may present with dry eyes and dry mouth as well as damage to other organ systems such as the liver, lungs, kidneys, and central nervous system.[17]
Undifferentiated Connective Tissue Disease
Individuals with symptoms of connective tissue disease and laboratory findings that suggest connective tissue disease but do not meet the criteria for classification for a specific connective tissue disease are said to have undifferentiated connective tissue disease.[10] These patients' symptoms may remain in this undifferentiated state, or they may eventually meet the criteria for diagnosis with a specific autoimmune disease.[18][11][19] Typically, a specific connective tissue disease develops relatively quickly from initial symptoms. Those individuals who do not advance beyond a diagnosis of undifferentiated connective tissue disease generally do not have related organ pathology.[20][21]
Overlap Syndromes
Patients are considered to have overlap syndrome when they meet the criteria for multiple defined autoimmune connective tissue diseases either concurrently or in sequence.[18] Mixed connective tissue disease (MCTD) is a condition that is considered by many to be an overlap syndrome.[10] This condition is characterized by an autoantibody to ribonucleoprotein (RNP) and presents clinically as systemic lupus erythematosus, systemic sclerosis, and polymyositis.[18][22] Diagnostic criteria are based on anti-RNP serology with myositis or synovitis plus two of the following: edema of hands, Raynaud phenomenon, sclerodactyly, and acrosclerosis. Pulmonary symptoms are prevalent in patients with mixed connective tissue disease. Patients may complain of cough, dyspnea, or pleuritic chest pain. Pulmonary hypertension is the most severe pulmonary consequence and often leads to premature death.[10]
Gene Defect-Related Connective Tissue Disease
Defective genes may sometimes cause abnormalities in the formation or strength of connective tissue. Several conditions fall within this category and impact multiple organ systems, including Ehlers-Danlos syndrome, most commonly characterized by hyperflexible joints and elastic skin; Marfan syndrome, associated with tall and thin individuals with long limbs; epidermolysis bullosa involving delicate and easily injured or blistered skin, and osteogenesis imperfecta involving brittle and easily fractured bone. Each of these conditions is complex, highly variable in patient presentation, may include damage to multiple organs and organ systems, and may range from mild to severe health-related quality of life reduction to the patient.
Media
(Click Image to Enlarge)
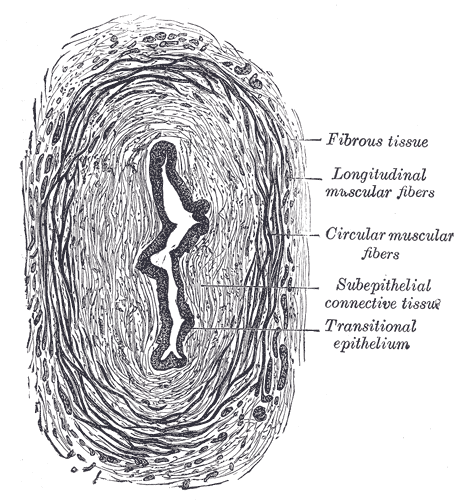
Transverse Section of the Ureter. The transverse section of the ureter's anatomy includes fibrous tissue, longitudinal muscular fibers, circular muscular fibers, subepithelial connective tissue, and transitional epithelium.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Ushiki T. Collagen fibers, reticular fibers and elastic fibers. A comprehensive understanding from a morphological viewpoint. Archives of histology and cytology. 2002 Jun:65(2):109-26 [PubMed PMID: 12164335]
Level 3 (low-level) evidenceWeatherholt AM, Fuchs RK, Warden SJ. Specialized connective tissue: bone, the structural framework of the upper extremity. Journal of hand therapy : official journal of the American Society of Hand Therapists. 2012 Apr-Jun:25(2):123-31; quiz 132. doi: 10.1016/j.jht.2011.08.003. Epub 2011 Nov 1 [PubMed PMID: 22047807]
Davies JE, Walker JT, Keating A. Concise Review: Wharton's Jelly: The Rich, but Enigmatic, Source of Mesenchymal Stromal Cells. Stem cells translational medicine. 2017 Jul:6(7):1620-1630. doi: 10.1002/sctm.16-0492. Epub 2017 May 10 [PubMed PMID: 28488282]
Yang G, Rothrauff BB, Tuan RS. Tendon and ligament regeneration and repair: clinical relevance and developmental paradigm. Birth defects research. Part C, Embryo today : reviews. 2013 Sep:99(3):203-222. doi: 10.1002/bdrc.21041. Epub [PubMed PMID: 24078497]
Level 3 (low-level) evidenceEDWARDS DA. The blood supply and lymphatic drainage of tendons. Journal of anatomy. 1946 Jul:80():147-52 [PubMed PMID: 20996686]
Liu Q, Wang X, Yi S. Pathophysiological Changes of Physical Barriers of Peripheral Nerves After Injury. Frontiers in neuroscience. 2018:12():597. doi: 10.3389/fnins.2018.00597. Epub 2018 Aug 23 [PubMed PMID: 30210280]
Light N, Champion AE. Characterization of muscle epimysium, perimysium and endomysium collagens. The Biochemical journal. 1984 May 1:219(3):1017-26 [PubMed PMID: 6743238]
Level 3 (low-level) evidenceKannus P. Structure of the tendon connective tissue. Scandinavian journal of medicine & science in sports. 2000 Dec:10(6):312-20 [PubMed PMID: 11085557]
Franchi M, Trirè A, Quaranta M, Orsini E, Ottani V. Collagen structure of tendon relates to function. TheScientificWorldJournal. 2007 Mar 30:7():404-20 [PubMed PMID: 17450305]
Level 3 (low-level) evidencePepmueller PH. Undifferentiated Connective Tissue Disease, Mixed Connective Tissue Disease, and Overlap Syndromes in Rheumatology. Missouri medicine. 2016 Mar-Apr:113(2):136-40 [PubMed PMID: 27311225]
Kardas T, Wielosz E, Majdan M. Methods of assessment of joint involvement in various systemic connective tissue diseases. Reumatologia. 2022:60(1):53-62. doi: 10.5114/reum.2022.114186. Epub 2022 Feb 28 [PubMed PMID: 35645418]
Durcan L, O'Dwyer T, Petri M. Management strategies and future directions for systemic lupus erythematosus in adults. Lancet (London, England). 2019 Jun 8:393(10188):2332-2343. doi: 10.1016/S0140-6736(19)30237-5. Epub 2019 Jun 6 [PubMed PMID: 31180030]
Level 3 (low-level) evidenceRose J. Autoimmune Connective Tissue Diseases: Systemic Lupus Erythematosus and Rheumatoid Arthritis. Emergency medicine clinics of North America. 2022 Feb:40(1):179-191. doi: 10.1016/j.emc.2021.09.003. Epub 2021 Oct 29 [PubMed PMID: 34782087]
Calderon LM, Pope JE. Scleroderma epidemiology update. Current opinion in rheumatology. 2021 Mar 1:33(2):122-127. doi: 10.1097/BOR.0000000000000785. Epub [PubMed PMID: 33481429]
Level 3 (low-level) evidenceCarstens PO, Schmidt J. Diagnosis, pathogenesis and treatment of myositis: recent advances. Clinical and experimental immunology. 2014 Mar:175(3):349-58. doi: 10.1111/cei.12194. Epub [PubMed PMID: 23981102]
Level 3 (low-level) evidenceSmolen JS, Aletaha D, McInnes IB. Rheumatoid arthritis. Lancet (London, England). 2016 Oct 22:388(10055):2023-2038. doi: 10.1016/S0140-6736(16)30173-8. Epub 2016 May 3 [PubMed PMID: 27156434]
Kyriakidis NC, Kapsogeorgou EK, Tzioufas AG. A comprehensive review of autoantibodies in primary Sjögren's syndrome: clinical phenotypes and regulatory mechanisms. Journal of autoimmunity. 2014 Jun:51():67-74. doi: 10.1016/j.jaut.2013.11.001. Epub 2013 Dec 13 [PubMed PMID: 24333103]
Level 3 (low-level) evidenceLeRoy EC, Maricq HR, Kahaleh MB. Undifferentiated connective tissue syndromes. Arthritis and rheumatism. 1980 Mar:23(3):341-3 [PubMed PMID: 7362686]
Martin Calderon L, Pope JE. Precursors to Systemic Sclerosis and Systemic Lupus Erythematosus: From Undifferentiated Connective Tissue Disease to the Development of Identifiable Connective Tissue Diseases. Frontiers in immunology. 2022:13():869172. doi: 10.3389/fimmu.2022.869172. Epub 2022 May 5 [PubMed PMID: 35603174]
Bodolay E, Csiki Z, Szekanecz Z, Ben T, Kiss E, Zeher M, Szücs G, Dankó K, Szegedi G. Five-year follow-up of 665 Hungarian patients with undifferentiated connective tissue disease (UCTD). Clinical and experimental rheumatology. 2003 May-Jun:21(3):313-20 [PubMed PMID: 12846049]
Level 2 (mid-level) evidenceVaz CC, Couto M, Medeiros D, Miranda L, Costa J, Nero P, Barros R, Santos MJ, Sousa E, Barcelos A, Inês L. Undifferentiated connective tissue disease: a seven-center cross-sectional study of 184 patients. Clinical rheumatology. 2009 Aug:28(8):915-21. doi: 10.1007/s10067-009-1175-2. Epub 2009 Apr 24 [PubMed PMID: 19390908]
Level 2 (mid-level) evidenceLee CT, Strek ME. The other connective tissue disease-associated interstitial lung diseases: Sjogren's syndrome, mixed connective tissue disease, and systemic lupus erythematosus. Current opinion in pulmonary medicine. 2021 Sep 1:27(5):388-395. doi: 10.1097/MCP.0000000000000791. Epub [PubMed PMID: 34127620]
Level 3 (low-level) evidence