Anatomy, Head and Neck: Ascending Palatine Artery
Anatomy, Head and Neck: Ascending Palatine Artery
Introduction
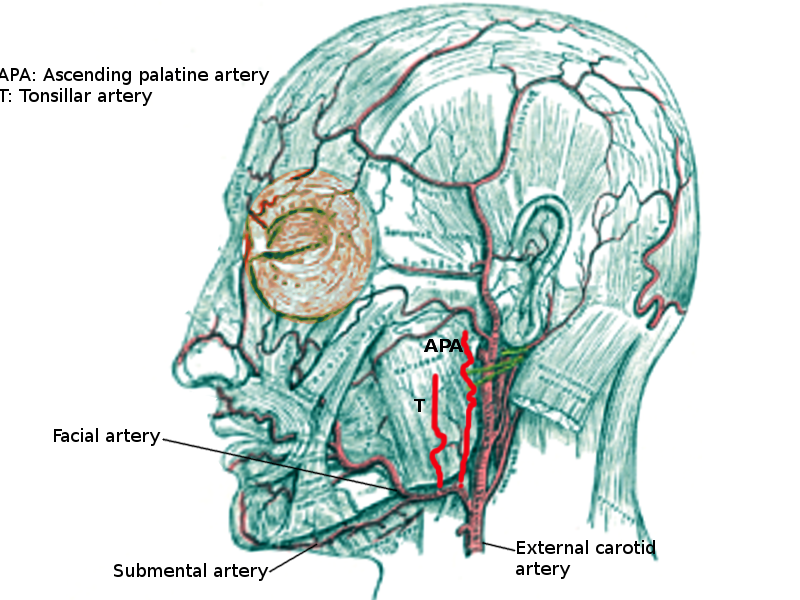
The ascending palatine artery most commonly originates from the facial artery and runs alongside the pharynx and passes between the styloglossus and the stylopharyngeus muscles. Its location is with the levator veli palatini where it divides into two branches to supply the soft palate and palatine glands. It later anastomoses with the descending palatine artery; which is a branch of the maxillary artery.
The ascending palatine artery can be divided into anterior and posterior branches as they supply the soft palate. However, this division may not be present in all individuals. The anterior branch without the posterior branch occurs in 25% of individuals, posterior branch without the anterior branch is present in 35%, and both anterior and posterior are the arrangement in 40% of individuals.[1] It is important to note that when the anterior branch is absent, the ascending palatine artery terminates close to the uvula.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The ascending palatine artery branches off of the facial artery and anastomoses with the tonsillar artery, ascending pharyngeal artery, and descending palatine artery. The artery goes on to supply the eustachian tube, palatine tonsils, and the soft palate; palatoglossus, palatopharyngeus, tensor veli palatini, musculus uvulae, and the levator veli palatini.[1][2] During surgery, the blood supply to the soft palate may be cut off due to damage to the ascending palatine artery; this is especially so in patients with absent anterior branches and posterior branches that stop close to the uvula.[1] The anterior branch has a mean diameter of 0.73 +/- 0.09 mm, as where the posterior branch measures 0.48 +/- 0.08 mm in diameter.[1]
Embryology
The development of the ascending palatine artery in utero begins during the 4th and 5th weeks. The aortic arches arise from the aortic sac which allows for the development of the external carotid artery from the 3rd arch, which gives rise to the facial artery which later gives rise to the ascending palatine artery.[3]
Blood Supply and Lymphatics
Blood Supply
The blood supply begins in the external carotid artery from which the facial artery branches. The facial artery then gives rise to the ascending palatine artery which then anastomoses with the tonsillar artery, ascending pharyngeal artery, and the descending palatine artery. The blood then continues to supply the soft palate; palatoglossus, palatopharyngeus, tensor veli palatini, musculus uvulae, and the levator veli palatine, as well as the eustachian tube, and palatine tonsils.[1][2] The prestyloid compartment, also known as the parapharyngeal space, receives the majority of its blood supply from the ascending palatine artery.[4]
Lymphatics
The palatine tonsils are known for supplying blood to the palatine tonsils, which are responsible for filtering bacteria and viruses while producing white blood cells and antibodies. The retropharyngeal lymph nodes also receive blood supply from the ascending palatine artery and the ascending pharyngeal artery. Therefore it is targeted in cases of head and neck squamous cell carcinoma when radiotherapy is necessary.[5]
Nerves
The ascending palatine artery arises in between the mylohyoid nerve and the hypoglossal nerve. The vagus nerve is the primary innervation of the soft palate where the ascending palatine artery is known for being the main blood supply.
Muscles
The ascending palatine artery's location passes between the styloglossus and the stylopharyngeus muscles where it later makes its way into the levator veli palatine muscle. This artery provides blood to the musculus uvulae, palatoglossus, palatopharyngeus, and the levator veli palatine muscles.[1][2] However, the palatopharyngeus muscle receives the majority of its blood supply from the ascending pharyngeal artery.[6]
Physiologic Variants
The presence of anterior and posterior branches of the ascending palatine artery differs between individuals. The anterior branch alone is expected to arise in 25% of people, the posterior alone is found 35% of the time, as where both anterior and posterior branches together are found in 40% of people.[1] The ascending palatine artery branches from the facial artery in 67% of individuals, with rare cases of the artery arising from the external carotid artery.[7][8]
Surgical Considerations
Osteotomies of the Le Fort l Segment
Osteotomies of the Le Fort l segment are common surgeries that are known to have low complication rates. The main complication includes ischemia which leads to avascular bone necrosis of the Le Fort l segment, which is rare. When completing this surgery, it is important to note that the ascending palatine artery, along with the ascending pharyngeal artery, are the main, and most common, blood supplies to the area.[9] However, the absence of the ascending palatine artery occurs in 10% of patients, leading to an increased risk of hypoperfusion and avascular necrosis.[9]
Complications Due to Physiologic Variations
When the anterior and posterior branches of the ascending palatine artery are not present simultaneously, there can be differences in surgical risks. When the ascending branch is non-existent, and the posterior branch terminates close to the uvula, there is an increased risk of damaging the main blood supply to the soft palate.[1]
Cleft Palate Repair
Knowledge of the soft palates arterial supply is important for surgical procedures of velopharyngeal incompetence and cleft palate. Cleft palates result in the arteries of the soft palate being displaced anterior-laterally due to the bone and muscle deformities.[10] It is suggested to dissect around the hamulus to avoid damage to the ascending palatine artery, which provides the main blood supply to the soft palate, ascending pharyngeal artery, and the recurrent pharyngeal arteries.[2][10] By dissecting around the hamulus, there is the prevention of wound breakdown, muscular fibrosis, and flap failure.[10]
Clinical Significance
Treatment of Recurrent Hemorrhage after Tonsillectomy
After a tonsillectomy bleeding from the lodge is a rare complication, occurring in approximately 3% of all patients.[11] This bleeding occurs due to a pseudoaneurysm of the tonsillar branch of the ascending palatine artery. Usually, reoperation or pharmacologic treatment is effective in stopping the bleed; however, in severe cases, endovascular therapy is the primary treatment.[11] The selective embolization of the ascending palatine artery is the best method for stopping a severe bleed.[11]
Hard Palate Necrosis after Ascending Palatine Artery Embolization
This procedure is a standard treatment used for refractory epistaxis is embolization. The embolization of the ascending palatine artery can result in unilateral necrosis of the mucosa that is superficial to the hard palate.[12] Surgical debridement alongside antibiotics and analgesic can be used to treat the necrosis of the tissue of the hard palate.[12]
Other Issues
The ascending palatine artery is not well researched and therefore requires more attention to gain further understanding of its function, physiological variations, clinical significance, and surgical considerations.
Media
References
Cho JH, Kim JW, Park HW, Suh JD, Kim JK, Yoon JH. Arterial supply of the human soft palate. Surgical and radiologic anatomy : SRA. 2017 Jul:39(7):731-734. doi: 10.1007/s00276-016-1798-3. Epub 2017 Jan 30 [PubMed PMID: 28138793]
Huang MH, Lee ST, Rajendran K. Clinical implications of the velopharyngeal blood supply: a fresh cadaveric study. Plastic and reconstructive surgery. 1998 Sep:102(3):655-67 [PubMed PMID: 9727428]
Meegalla N, Sood G, Nessel TA, Downs BW. Anatomy, Head and Neck: Facial Arteries. StatPearls. 2023 Jan:(): [PubMed PMID: 30725617]
Katori Y, Kawase T, Cho KH, Abe H, Rodríguez-Vázquez JF, Murakami G, Abe S. Prestyloid compartment of the parapharyngeal space: a histological study using late-stage human fetuses. Surgical and radiologic anatomy : SRA. 2012 Dec:34(10):909-20. doi: 10.1007/s00276-012-0975-2. Epub 2012 May 11 [PubMed PMID: 22576264]
Suzuki T, Sakashita T, Homma A, Hatakeyama H, Kano S, Mizumachi T, Yoshida D, Fujima N, Onimaru R, Tsuchiya K, Yasuda K, Shirato H, Suzuki F, Fukuda S. Effectiveness of superselective intra-arterial chemoradiotherapy targeting retropharyngeal lymph node metastasis. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2016 Oct:273(10):3331-6. doi: 10.1007/s00405-016-3933-5. Epub 2016 Feb 13 [PubMed PMID: 26874732]
Cheng NX, Zhang KQ. [The applied anatomic study of palatopharyngeus muscle]. Zhonghua zheng xing wai ke za zhi = Zhonghua zhengxing waike zazhi = Chinese journal of plastic surgery. 2004 Sep:20(5):384-7 [PubMed PMID: 15623114]
Wang C, Kundaria S, Fernandez-Miranda J, Duvvuri U. A description of arterial variants in the transoral approach to the parapharyngeal space. Clinical anatomy (New York, N.Y.). 2014 Oct:27(7):1016-22. doi: 10.1002/ca.22273. Epub 2014 Feb 7 [PubMed PMID: 24510490]
Touré G, Moreau A, Ndiaye M, Ory A. Vascularization of the maxilla by a branch of the submandibular artery. Journal of stomatology, oral and maxillofacial surgery. 2019 Sep:120(4):366-368. doi: 10.1016/j.jormas.2019.01.015. Epub 2019 Feb 11 [PubMed PMID: 30763777]
Bruneder S, Wallner J, Weiglein A, Kmečová Ĺ, Egger J, Pilsl U, Zemann W. Anatomy of the Le Fort I segment: Are arterial variations a potential risk factor for avascular bone necrosis in Le Fort I osteotomies? Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2018 Aug:46(8):1285-1295. doi: 10.1016/j.jcms.2018.04.023. Epub 2018 May 2 [PubMed PMID: 29805066]
Cheng N, Zhang K, Song R. [Applied anatomy of arterial supply for the soft palate]. Zhonghua zheng xing wai ke za zhi = Zhonghua zhengxing waike zazhi = Chinese journal of plastic surgery. 2000 Jul:16(4):208-11 [PubMed PMID: 11593673]
Guziński M, Garcarek J, Kurcz J, Masalski M, Krecicki T. [Endovascular treatment of recurrent hemorrhage after tonsillectomy]. Przeglad lekarski. 2012:69(7):314-6 [PubMed PMID: 23276023]
Level 3 (low-level) evidenceAlalawi WA, Almajed E. Unilateral Hard Palate Necrosis After Ascending Palatine Artery Embolization. The Journal of craniofacial surgery. 2018 Jul:29(5):e437-e438. doi: 10.1097/SCS.0000000000004456. Epub [PubMed PMID: 29521756]