 Anatomy, Shoulder and Upper Limb, Coracoclavicular Joint (Coracoclavicular Ligament)
Anatomy, Shoulder and Upper Limb, Coracoclavicular Joint (Coracoclavicular Ligament)
Introduction
The coracoclavicular ligament (CCL) serves as the acromioclavicular ligament's primary support (see Image. Left Shoulder Anatomy). These 2 ligaments coordinate to stabilize the acromioclavicular joint (ACJ), a major shoulder joint. The ACJ is a synovial plane joint that helps stabilize the shoulder girdle.[1] This joint's primary support derives from the acromioclavicular ligament intrinsic to the joint and the CCL extrinsic to the articulation. The CCL does not directly cross the ACJ. However, the CCL helps maintain the proper anatomical relationship of the acromion to the clavicle.
CCL injuries are commonly associated with shoulder separations, particularly in high-impact sports or trauma. Surgical intervention may be necessary for severe CCL injuries. Understanding the anatomy and function of this ligament is essential for managing various conditions affecting the shoulder.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Structure
The CCL is a complex ligament comprised of 2 parts: the conoid and trapezoid ligaments. The trapezoid ligament inserts 3 cm from the distal end of the clavicle, while the conoid insertion is slightly posterior, 4.5 cm from the clavicle's distal end [2]. The CCL's component ligaments are continuous inferiorly at the coracoid process attachment but separate at an angle before attaching superiorly to the clavicle's inferior aspect.[3] A bursa or fat often separates the conoid and trapezoid ligaments.
The conoid ligament attaches to the clavicle at the conoid tubercle posteromedial to the trapezoid tubercle. The conoid ligament appears as an inferiorly pointing cone, with its superior clavicular attachment being wide and inferior attachment being narrow, wrapping around posteromedially to the coracoid process's root.
The trapezoid ligament typically lies anterolateral to the conoid ligament. The trapezoid ligament is quadrilateral in shape, as its name implies, and is thinner than the conoid ligament. This ligament attaches inferiorly to the coracoid process's posterosuperior aspect, coming in contact with the conoid ligament's anterior margin. The trapezoid ligament angles anterolaterally away from the conoid ligament, while the conoid ligament is nearly vertical. The trapezoid ligament attaches to the trapezoid line on the clavicle's inferior surface. A bursa separates the trapezoid and conoid ligaments.
Function
The CCL connects the clavicle and the scapula's coracoid process. The conoid and trapezoid ligaments allow proper acromioclavicular apposition while preventing vertical scapular displacement toward the clavicle. The angled space between the 2 component ligaments allows for slight scapular rotation about the clavicle. The CCL is not an intrinsic ACJ component but contributes to its stability.
Some authors describe a "medial coracoclavicular ligament" (Caldani bicorne ligament) and consider the CCL a lateral ligament. The medial coracoclavicular ligament was first described in 1802, lying between the coracoid process' posterosuperior portion, the first rib's medial border, and the inferior region of the clavicle's middle third. The medial coracoclavicular ligament appears as a pearlescent yellow fibrous structure with a length of about 59.5 mm. This medial ligament helps stabilize the ACJ and acts as a last brake during cranial and posterior tractions.
Embryology
The CCL's embryological origin and development are still under analysis. Given the ligament's integral association with musculoskeletal anatomy, the belief is that precursor cells within the ligament primordia initially develop independently but later integrate to form a single functioning joint.[4] Multiple markers for joint structure development have been studied in animal models, including BMP, Wnt14, Gdf5/Gdf6, and α5β1 integrin.[5][6] Other studies have also pointed to Scleraxis as a ligament development marker, though further analysis of its expression is required.[7] The embryological leaflet involved in CCL development is the mesoderm.
Blood Supply and Lymphatics
The CCL's primary structures receive their blood supply from 2 sources. The first is the suprascapular artery, which arises from the subclavian artery at the thyrocervical trunk. The second is the thoracoacromial branch, which derives from the axillary artery. The suprascapular vein, related to the CCL, drains toward the external jugular vein. In the area of the CCL are lymphatic nodes draining the axillary and cervical regions.
Nerves
Joints are innervated according to the Hilton Law, which states that joints receive innervation from the articular branches of nerves supplying the muscles acting on the joint. The CCL region is innervated by brachial plexus branches, specifically the suprascapular, axillary, and lateral pectoral nerves' articular branches.
Muscles
Various muscles move and stabilize the shoulder girdle. The CCL supports the coracoclavicular articulation during complex shoulder movements to prevent separating the scapula from the clavicle. Muscles primarily causing movement around these structures include the serratus anterior, trapezius, teres major, rhomboid major, rhomboid minor, and triceps brachii's long head. These muscles attach directly to the scapula, contributing to the CCL's mechanical stability and movement restriction. The pectoralis minor tendon crosses the fascial arch created by the medial coracoclavicular ligament at the level of the coracoid process.
Physiologic Variants
A 1975 study reported that CCL variation may involve the ligament's replacement with a coracoclavicular bone bridge.[8] Meanwhile, a 2004 radiographic study comparing the prevalence of coracoclavicular joints (CCJs) in the French population with skeletal remains from medieval times reported the prevalence of CCJs to be 0.82%.[9] A 2021 US osteological study found that 9% of 2,724 subjects had this anomaly and that it was more prevalent among African Americans and women. However, the reported figures about CCJ frequency in the population vary widely, depending on the study.[10]
Another cadaveric research analyzed 24 CCLs to determine variations. Researchers found 3 conoid ligament variants. Of 18 conoid ligaments, 9 attached to the root of the coracoid process, 6 were confluent with the superior transverse scapular ligament, and 3 had a distinct fascicle that originated at the conoid ligament's inferior attachment and inserted superiorly onto the trapezoid ligament's lateral attachment.[11]
Surgical Considerations
Acromioclavicular and coracoclavicular injuries are managed in various ways.[12][13][14] Treatment recommendations are based on the Rockwood Classification of Acromioclavicular Joint Separation.[15] Types I and II injuries generally receive nonoperative treatment, typically managed with sling immobilization, rest, ice, and physical therapy. Type III injuries are managed individually, as no consensus currently exists about optimal operative management for this group. Types IV, V, and VI injuries are managed surgically with one of the methods discussed below.
Managing types IV, V, and VI ACJ dislocations has recently shifted toward anatomical coracoclavicular reconstruction.[16][17] The procedure necessitates treating the conoid and trapezoid ligaments separately and restoring their attachment sites near the physiological origin. Anatomic reconstruction can increase the risk of low-impact fractures, as it entails bone tunnel formation for anchoring.[18][19] Other limitations include decreased range of motion, revision failure, rotational pain, and incision site pain or deformity.[20]
Methods of anatomic reconstruction include allographic reconstruction and fixation with a suture button. Prior methods to stabilize the acromioclavicular and coracoclavicular joints have included screws (Bosworth technique), pins (Phemister technique), and cerclage wires or lag screws from the clavicle to the coracoid. These methods demonstrate good outcomes, though reported issues include hardware failure, pin migration, and loss of reduction. Studies show that anatomic coracoclavicular reconstruction, with either a suture button or native reconstruction, provides good-to-excellent outcomes.[21][22]
Additionally, a 58-month follow-up of 23 patients who underwent suture-button coracoclavicular fixation showed that 96% were satisfied or very satisfied with the procedure's outcome.[23] However, Calvert et al's multicenter study of 119 cases reported an overall 27.1% complication rate, 11 of which were due to hardware failure.[24]
Clinical Significance
Symptomatic Coracoclavicular Joint
A symptomatic CCJ is a condition associated with the actual presence of a CCJ. While CCJ prevalence is low, the literature suggests this condition is typically asymptomatic.[25] Symptomatic CCJs are treated conservatively before surgical correction.[26]
Trauma
ACJ injuries commonly result from a direct fall onto the shoulder (see Image. Acromioclavicular Joint Dislocation). Direct and indirect trauma may lead to acromioclavicular dislocation or failure. The CCL helps oppose joint separation and maintain the approximation of the acromion and clavicle. Disruption of a CCL component converts the other component into a fulcrum, enabling the coracoid process to rotate beneath the clavicle. ACJ injuries create vulnerable regions that enhance the risk of succeeding ACJ dislocations. The Rockwood Classification categorizes injuries with CCL rupture under grades III to VI.[27]
The Rockwood Classification is as follows:
- Type I: Acromioclavicular ligament sprain with intact joint space and no coracoclavicular involvement
- Type II: Acromioclavicular ligament tear with widened joint space. An intact CCL maintains the coracoclavicular distance.
- Type III: Complete acromioclavicular ligament disruption. CCLs are disrupted up to 100%, though they remain intact and attached to the periosteal sleeve. This injury type has a high probability of muscle detachment, with the clavicle mildly displaced superiorly.
- Type IV: ACJ rupture with posterior joint dislocation into the trapezius. The acromioclavicular ligament is completely disrupted. The widened joint space is evident. Coracoclavicular disruption may be partial or complete.
- Type V: Demonstrates complete disruption of the acromioclavicular and coracoclavicular ligaments and muscle attachments. The clavicle dislocates superiorly.
- Type VI: Complete acromioclavicular ligament disruption. The CCL is completely torn, and the coracoclavicular interval does not exist. Muscle attachments are partially intact or absent. The clavicle is displaced inferiorly relative to the acromion process.
Septic Arthritis of the Acromioclavicular Joint
ACJ septic arthritis can lead to significant mortality and morbidity. The condition can easily be confused with septic glenohumeral joint arthritis. Pain and erythema overlying the ACJ are characteristic.[28] ACJ septic arthritis is rare but mostly affects immunocompromised patients and men in the 5th and 6th decades of life.
Septic arthritis usually arises from hematogenous bacterial spread to the affected joint. More vascularized joints have an increased risk of infection. Septic arthritis most commonly involves the knee, hip, shoulder, ankle, and foot. By comparison, ACJ sepsis is relatively rare due to the joint's decreased vascularity and size.[29] ACJ septic arthritis has been reported in a 69-year-old man with Klinefelter syndrome with shoulder pain and septic arthritis. Metabolic syndrome, manifesting as obesity, hypercholesterolemia, hypertension, and impaired glucose tolerance, also increases ACJ pathology risk. Microbial agents causing ACJ sepsis include Staphylococcus aureus, Cryptococcus neoformans, and Haemophilus influenzae.[30]
The treatment for this condition is antimicrobial therapy with or without surgery or aspiration.[31] Surgical compression may be performed arthroscopically or through an open approach in severe ACJ sepsis.[32] Drainage is an option in less severe cases.
Osteomyelitis may result from the surgical reconstruction of an injured ACJ. Poor hygiene and nonadherence to postsurgical wound care protocols are possible risk factors.[33] Management requires intravenous antibiotics and, often, surgical exploration.[34]
Other Issues
Behavioral and Structural Properties of the Coracoclavicular Ligament
The viscoelastic properties of the CCL components differ from those of other ligaments within the shoulder capsule. The conoid and trapezoid ligaments' structural properties are similar, and both are stiffer than the coracoacromial ligament's lateral band and the glenohumeral ligaments.[35][36] Further, the anatomical orientation of the ligamentous fibers comprising the CCL alters its loading dynamics and ability to respond to external loads, increasing rupture risk.[37] The structural properties of each CCL component are thus essential in supporting the ACJ when subjected to various internal and external loading forces.
Coracoclavicular Joint Osteoarthritis
The CCJ is a rare anatomical entity. CCL degeneration within this joint is even rarer. However, when present, the condition can lead to shoulder pain or discomfort. Diagnosis may be difficult due to a lack of awareness among clinicians, potentially resulting in delayed therapy. Imaging modalities such as standing radiographs and dynamic magnetic resonance imaging may help visualize a symptomatic CCJ.
Symptomatic CCJs may be differentiated from subcoracoid impingement through local anesthetic injections. Nonoperative interventions include anti-inflammatories, physiotherapy, and corticosteroid injections, with surgical excision reserved for cases refractory to conservative measures. Besides hampering normal movement and causing pain, CCJs have been reported to exacerbate thoracic outlet syndrome in some individuals.[38]
Media
(Click Image to Enlarge)
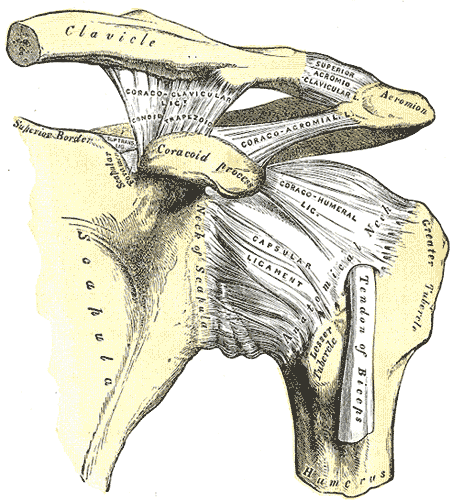
Left Shoulder Anatomy. This image shows the anatomic relationships between the clavicle, scapula, scapular neck, foramen, and superior border, coracoid process, acromion, greater and lesser humeral tubercles, humerus and anatomical neck, tendon of the biceps brachii long head, and the coracoclavicular (with the conoid and trapezoid), coracoacromial, superior acromioclavicular, coracohumeral, and capsular ligaments.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)

Acromioclavicular Joint Dislocation. The acromioclavicular joint is generally damaged following falls, producing direct shoulder trauma. The scapula is pushed inferiorly while the clavicle remains in position. The loss of contact between the two bony heads is called "dislocation." The left coracoclavicular ligament was severely damaged in this patient, resulting in acromioclavicular joint dislocation.
Contributed by Bruno Bordoni, PhD
References
Nakazawa M, Nimura A, Mochizuki T, Koizumi M, Sato T, Akita K. The Orientation and Variation of the Acromioclavicular Ligament: An Anatomic Study. The American journal of sports medicine. 2016 Oct:44(10):2690-2695 [PubMed PMID: 27315820]
Zhu NF, Rui BY, Zhang YL, Chen YF. Anatomic study of coracoclavicular ligaments for reconstruction of acromioclavicular joint dislocations. Journal of orthopaedic science : official journal of the Japanese Orthopaedic Association. 2016 Nov:21(6):749-752. doi: 10.1016/j.jos.2016.08.001. Epub 2016 Aug 27 [PubMed PMID: 27576109]
Hyland S, Charlick M, Varacallo M. Anatomy, Shoulder and Upper Limb, Clavicle. StatPearls. 2024 Jan:(): [PubMed PMID: 30252246]
Shukunami C, Yoshimoto Y, Takimoto A, Yamashita H, Hiraki Y. Molecular characterization and function of tenomodulin, a marker of tendons and ligaments that integrate musculoskeletal components. The Japanese dental science review. 2016 Nov:52(4):84-92. doi: 10.1016/j.jdsr.2016.04.003. Epub 2016 Apr 27 [PubMed PMID: 28408960]
Montero JA, Lorda-Diez CI, Sanchez-Fernandez C, Hurle JM. Cell death in the developing vertebrate limb: A locally regulated mechanism contributing to musculoskeletal tissue morphogenesis and differentiation. Developmental dynamics : an official publication of the American Association of Anatomists. 2021 Sep:250(9):1236-1247. doi: 10.1002/dvdy.237. Epub 2020 Sep 2 [PubMed PMID: 32798262]
Marín-Llera JC, Garciadiego-Cázares D, Chimal-Monroy J. Understanding the Cellular and Molecular Mechanisms That Control Early Cell Fate Decisions During Appendicular Skeletogenesis. Frontiers in genetics. 2019:10():977. doi: 10.3389/fgene.2019.00977. Epub 2019 Oct 11 [PubMed PMID: 31681419]
Level 3 (low-level) evidenceTozer S, Duprez D. Tendon and ligament: development, repair and disease. Birth defects research. Part C, Embryo today : reviews. 2005 Sep:75(3):226-36 [PubMed PMID: 16187327]
McClure JG, Raney RB. Anomalies of the scapula. Clinical orthopaedics and related research. 1975 Jul-Aug:(110):22-31 [PubMed PMID: 808367]
Nehme A, Tricoire JL, Giordano G, Rouge D, Chiron P, Puget J. Coracoclavicular joints. Reflections upon incidence, pathophysiology and etiology of the different forms. Surgical and radiologic anatomy : SRA. 2004 Feb:26(1):33-8 [PubMed PMID: 14574466]
Level 2 (mid-level) evidenceHarlow ER, Sasala LM, Talbot CE, Desai BJ, Ina J, Miskovsky S. Prevalence and Morphology of the Coracoclavicular Joint: An Osteological Study of 2,724 Subjects Using Univariable and Multivariable Logistic Regression Analyses. Frontiers in surgery. 2021:8():761441. doi: 10.3389/fsurg.2021.761441. Epub 2021 Oct 28 [PubMed PMID: 34778366]
Harris RI, Vu DH, Sonnabend DH, Goldberg JA, Walsh WR. Anatomic variance of the coracoclavicular ligaments. Journal of shoulder and elbow surgery. 2001 Nov-Dec:10(6):585-8 [PubMed PMID: 11743540]
Beitzel K, Cote MP, Apostolakos J, Solovyova O, Judson CH, Ziegler CG, Edgar CM, Imhoff AB, Arciero RA, Mazzocca AD. Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2013 Feb:29(2):387-97. doi: 10.1016/j.arthro.2012.11.023. Epub [PubMed PMID: 23369483]
Level 1 (high-level) evidenceCisneros LN, Reiriz JS. Management of chronic unstable acromioclavicular joint injuries. Journal of orthopaedics and traumatology : official journal of the Italian Society of Orthopaedics and Traumatology. 2017 Dec:18(4):305-318. doi: 10.1007/s10195-017-0452-0. Epub 2017 Mar 8 [PubMed PMID: 28275882]
Tamaoki MJ, Belloti JC, Lenza M, Matsumoto MH, Gomes Dos Santos JB, Faloppa F. Surgical versus conservative interventions for treating acromioclavicular dislocation of the shoulder in adults. The Cochrane database of systematic reviews. 2010 Aug 4:2010(8):CD007429. doi: 10.1002/14651858.CD007429.pub2. Epub 2010 Aug 4 [PubMed PMID: 20687087]
Level 1 (high-level) evidenceBorbas P, Churchill J, Ek ET. Surgical management of chronic high-grade acromioclavicular joint dislocations: a systematic review. Journal of shoulder and elbow surgery. 2019 Oct:28(10):2031-2038. doi: 10.1016/j.jse.2019.03.005. Epub 2019 Jul 23 [PubMed PMID: 31350107]
Level 1 (high-level) evidenceWarth RJ, Martetschläger F, Gaskill TR, Millett PJ. Acromioclavicular joint separations. Current reviews in musculoskeletal medicine. 2013 Mar:6(1):71-8. doi: 10.1007/s12178-012-9144-9. Epub [PubMed PMID: 23242975]
Phadke A, Bakti N, Bawale R, Singh B. Current concepts in management of ACJ injuries. Journal of clinical orthopaedics and trauma. 2019 May-Jun:10(3):480-485. doi: 10.1016/j.jcot.2019.03.020. Epub 2019 Apr 1 [PubMed PMID: 31061573]
Tauber M, Gordon K, Koller H, Fox M, Resch H. Semitendinosus tendon graft versus a modified Weaver-Dunn procedure for acromioclavicular joint reconstruction in chronic cases: a prospective comparative study. The American journal of sports medicine. 2009 Jan:37(1):181-90. doi: 10.1177/0363546508323255. Epub 2008 Sep 25 [PubMed PMID: 18818433]
Level 2 (mid-level) evidenceWylie JD, Johnson JD, DiVenere J, Mazzocca AD. Shoulder Acromioclavicular and Coracoclavicular Ligament Injuries: Common Problems and Solutions. Clinics in sports medicine. 2018 Apr:37(2):197-207. doi: 10.1016/j.csm.2017.12.002. Epub [PubMed PMID: 29525023]
Millett PJ, Horan MP, Warth RJ. Two-Year Outcomes After Primary Anatomic Coracoclavicular Ligament Reconstruction. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2015 Oct:31(10):1962-73. doi: 10.1016/j.arthro.2015.03.034. Epub 2015 May 19 [PubMed PMID: 25998014]
Lee S, Bedi A. Shoulder acromioclavicular joint reconstruction options and outcomes. Current reviews in musculoskeletal medicine. 2016 Dec:9(4):368-377 [PubMed PMID: 27645218]
Fauci F, Merolla G, Paladini P, Campi F, Porcellini G. Surgical treatment of chronic acromioclavicular dislocation with biologic graft vs synthetic ligament: a prospective randomized comparative study. Journal of orthopaedics and traumatology : official journal of the Italian Society of Orthopaedics and Traumatology. 2013 Dec:14(4):283-90. doi: 10.1007/s10195-013-0242-2. Epub 2013 May 7 [PubMed PMID: 23649818]
Level 1 (high-level) evidenceVenjakob AJ, Salzmann GM, Gabel F, Buchmann S, Walz L, Spang JT, Vogt S, Imhoff AB. Arthroscopically assisted 2-bundle anatomic reduction of acute acromioclavicular joint separations: 58-month findings. The American journal of sports medicine. 2013 Mar:41(3):615-21. doi: 10.1177/0363546512473438. Epub 2013 Jan 31 [PubMed PMID: 23371472]
Clavert P, Meyer A, Boyer P, Gastaud O, Barth J, Duparc F, SFA. Complication rates and types of failure after arthroscopic acute acromioclavicular dislocation fixation. Prospective multicenter study of 116 cases. Orthopaedics & traumatology, surgery & research : OTSR. 2015 Dec:101(8 Suppl):S313-6. doi: 10.1016/j.otsr.2015.09.012. Epub 2015 Nov 3 [PubMed PMID: 26545944]
Level 2 (mid-level) evidenceNikolaides AP, Dermon AR, Papavasiliou KA, Kirkos JM. Coracoclavicular joint degeneration, an unusual cause of painful shoulder: a case report. Acta orthopaedica Belgica. 2006 Jan:72(1):90-2 [PubMed PMID: 16570902]
Level 3 (low-level) evidenceSingh VK, Singh PK, Trehan R, Thompson S, Pandit R, Patel V. Symptomatic coracoclavicular joint: incidence, clinical significance and available management options. International orthopaedics. 2011 Dec:35(12):1821-6. doi: 10.1007/s00264-011-1309-4. Epub 2011 Jul 15 [PubMed PMID: 21761150]
Gorbaty JD, Hsu JE, Gee AO. Classifications in Brief: Rockwood Classification of Acromioclavicular Joint Separations. Clinical orthopaedics and related research. 2017 Jan:475(1):283-287. doi: 10.1007/s11999-016-5079-6. Epub 2016 Sep 16 [PubMed PMID: 27637619]
Williams M. Diagnostic challenges in acromioclavicular septic arthritis. BMJ case reports. 2016 Jun 2:2016():. doi: 10.1136/bcr-2016-216034. Epub 2016 Jun 2 [PubMed PMID: 27257000]
Level 3 (low-level) evidenceHong MJ, Kim YD, Ham HD. Acute septic arthritis of the acromioclavicular joint caused by Haemophilus parainfluenzae: a rare causative origin. Clinical rheumatology. 2015 Apr:34(4):811-4. doi: 10.1007/s10067-014-2554-x. Epub 2014 Mar 4 [PubMed PMID: 24584486]
Corey SA, Agger WA, Saterbak AT. Acromioclavicular septic arthritis and sternoclavicular septic arthritis with contiguous pyomyositis. Clinics in orthopedic surgery. 2015 Mar:7(1):131-4. doi: 10.4055/cios.2015.7.1.131. Epub 2015 Feb 10 [PubMed PMID: 25729529]
Level 3 (low-level) evidenceSteinmetz RG, Maupin JJ, Smith JN, White CB. Septic arthritis of the acromioclavicular joint: a case series and review of the literature. Shoulder & elbow. 2020 Aug:12(4):272-283. doi: 10.1177/1758573218815289. Epub 2018 Dec 4 [PubMed PMID: 32788932]
Level 2 (mid-level) evidenceThomas J, Daud M, Macmull S. Acute septic arthritis of the acromioclavicular joint caused by Staphylococcus aureus with marked soft tissue collection towards posterior medial aspect of the AC joint: A rare clinical presentation. IDCases. 2022:29():e01513. doi: 10.1016/j.idcr.2022.e01513. Epub 2022 May 24 [PubMed PMID: 35663610]
Level 3 (low-level) evidenceYeak RD, Daud H, Nizlan NM. Osteomyelitis post acromioclavicular joint reconstruction. Chinese journal of traumatology = Zhonghua chuang shang za zhi. 2019 Jun:22(3):182-185. doi: 10.1016/j.cjtee.2019.03.004. Epub 2019 Apr 20 [PubMed PMID: 31060897]
Oswald A, Alorda A, Tassone M, Walker A, Ganti L. Acromioclavicular Osteomyelitis: When Simple Cellulitis Is No Longer Simple. Orthopedic reviews. 2022:14(3):36909 [PubMed PMID: 35936799]
Soslowsky LJ, An CH, DeBano CM, Carpenter JE. Coracoacromial ligament: in situ load and viscoelastic properties in rotator cuff disease. Clinical orthopaedics and related research. 1996 Sep:(330):40-4 [PubMed PMID: 8804273]
Boardman ND, Debski RE, Warner JJ, Taskiran E, Maddox L, Imhoff AB, Fu FH, Woo SL. Tensile properties of the superior glenohumeral and coracohumeral ligaments. Journal of shoulder and elbow surgery. 1996 Jul-Aug:5(4):249-54 [PubMed PMID: 8872921]
Costic RS, Vangura A Jr, Fenwick JA, Rodosky MW, Debski RE. Viscoelastic behavior and structural properties of the coracoclavicular ligaments. Scandinavian journal of medicine & science in sports. 2003 Oct:13(5):305-10 [PubMed PMID: 14507296]
Schuh A, Seehaus F, Onyemaechi NO, Hönle W. Osteoarthritis in a symptomatic coracoclavicular joint. Global medicine and therapeutics. 2018 Dec:3(1):. doi: 10.15761/gmt.1000106. Epub 2018 Mar 30 [PubMed PMID: 35425879]
