Introduction
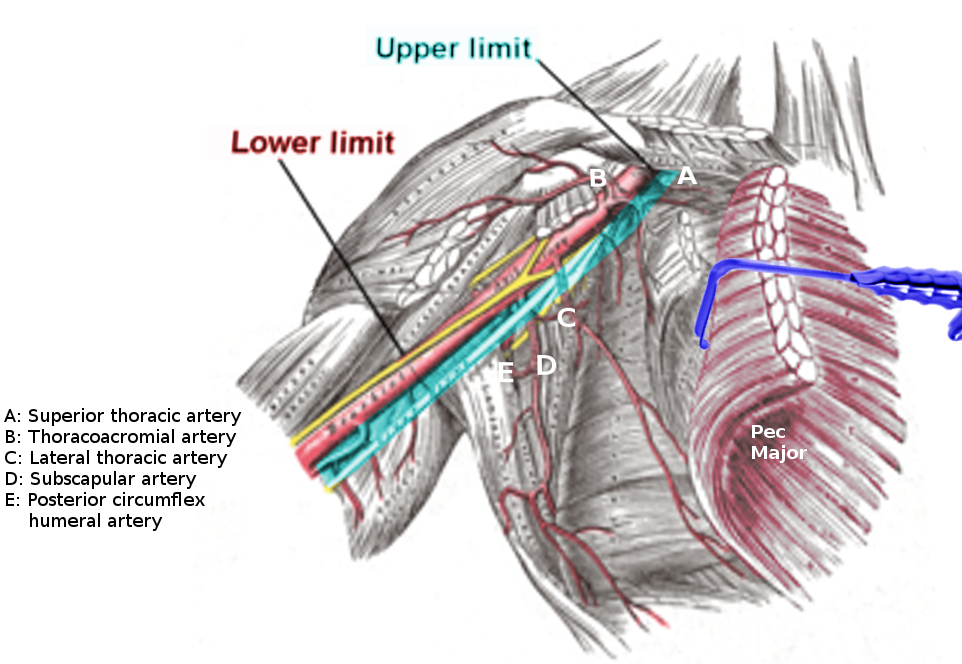
The axillary artery has three divisions, based on relative positioning to the pectoralis minor muscle. The superior thoracic artery, also referred to as the supreme thoracic artery, is the first branch of the axillary artery. This artery courses anteriorly and medially along the superior border of the pectoralis minor muscle. The superior thoracic artery then passes between the lateral aspect of the chest and the pectoralis minor muscle. Typically, this artery proceeds to anastomose with the intercostal and the internal thoracic artery. However, there are several physiological variants in both the origin and anastomoses of this artery. In most individuals, it is the only branch of the first division of the axillary artery. The superior thoracic is a small artery that can usually be palpated two finger widths below the clavicle on the midclavicular line.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Typically, the superior thoracic artery is the first and only branch off of the first division of the axillary artery. It runs medially along the superior border of the pectoralis minor muscle, inferior to the subclavius and distal to the lateral border of the first rib — branches of the superior thoracic artery supply the first and second intercostal spaces. Additionally, the superior portion of the serratus anterior gets its vascular supply by terminal branches of this artery. The intermediate and inferior portions of the serratus anterior muscle are supplied by the lateral thoracic and thoracodorsal arteries, respectively. The superior thoracic artery anastomosis with the several branches of the internal thoracic (mammary) artery.[1] These anastomoses are both direct and indirect through the superior two branches of the anterior intercostal artery.
Embryology
As with all branches of the axillary artery, the superior thoracic artery develops from the vascular plexus of the upper limb bud.[2] The upper limb bud forms as a result of interactions between the ectoderm and underlying lateral plate mesoderm. The axial trunk develops around the middle of the fourth week, or approximately day 32, of fetal development. By 41 days, the axillary artery and its branches, including the superior thoracic, are typically formed. The development of the lower limb bud, and its vascular plexus, usually follows around four days later. The positioning of the limb buds in all species is associated with the level of Hox gene expression along the anterior-posterior axis.[3] Therefore, any alterations in either the expression or functioning of these genes can influence the upper limb bud, vascular plexus, and the eventual development of the superior thoracic artery.
Blood Supply and Lymphatics
The superior thoracic is the first branch of the axillary artery, which itself is an extension of the subclavian artery. Venous blood is drained by branches of the axillary vein, which runs medial to the axillary artery along its entire course.
Muscles
The superior portion of the serratus anterior and the intercostal muscles of the first and second intercostal spaces are the only muscles typically perfused by the superior thoracic artery.
Physiologic Variants
There are numerous physiological variants associated with the superior thoracic artery. The most common variant is when the artery branches off the second part of the axillary via the thoracoacromial artery. One case report of a willed-body donor in India reported a particularly unusual course. In this individual, the superior thoracic originated from the lateral aspect of the first branch of the axillary. It then passed between the two divisions of the lateral cord of the brachial plexus.[4] There are also reports where the superior thoracic may not be the only branch of the first portion of the axillary artery. In some rare cases, the subscapular artery may also branch off the proximal axillary artery.[5] Typically, these physiological variants have little to no effect on the blood supply to the serratus anterior or the first and second intercostal muscles. As reported above, these variants are usually identified incidentally in willed-bodied donors. Although speculated that individuals of Black race origin might have a higher incidence of physiological variations, there is insubstantial data to support this claim.
Surgical Considerations
Any procedure involving the subclavian or axillary artery has the potential to affect the superior thoracic artery. These may include surgery for the correction of congenital anomalies such as an aberrant subclavian or during repair of an axillary artery dissection. Given the size and location of the artery, iatrogenic injuries are very rare.
Clinical Significance
Injuries to the superior thoracic artery are rare. When these injuries occur, they often present in cases of penetrating neck/chest trauma. The subclavian/axillary arteries and their branches are only involved in approximately 3% of penetrating neck and chest trauma injuries due to protection from overlying structures. However, damage to these arteries is associated with significant morbidity and mortality. Most patients will die before reaching the hospital, and those who survive will often have severely impaired the functioning of the affected limb due to brachial plexus injuries. 14% of these arterial injuries have a concomitant first rib or clavicular injuries.[6] Cases with rib and clavicular injuries are more likely to have superior thoracic artery involvement. Other potential causes of injury include anterior shoulder dislocations. These cases are more common in elderly populations with a higher propensity for fall-related injuries.
Rarely, the superior thoracic artery can suffer damage during percutaneous coronary interventions (PCI). Uchikado et al. reported a unique case of injury to the superior thoracic during sheath insertion for stent placement. The patient tolerated the procedure well; however, they reported nausea and hypotension with no abnormal physical findings one-hour post PCI. The authors initially suspected vasovagal reflex, and the diagnosis of superior thoracic injury did not occur until after performing angiography.[7] Female sex, short height, anticoagulation, and excessive wire manipulation have been identified as key risk factors for the development of peripheral arterial perforation.[8] In these patients, damage to small vessels such as the superior thoracic artery should merit consideration in the context of shock after PCI. However, these injuries are extremely rare as the reported incidence of angiographic-evident peripheral artery perforation is only 0.9%.[9] An additional consideration is during coronary artery bypass graft (CABG) open-heart procedures. During these procedures, the internal thoracic (mammary) artery is the most frequently used arterial graft for myocardial revascularization due to its intrinsic resistance to atherosclerotic disease.[10] It is often a preferred option over the saphenous vein due to higher long term graft patency. When harvesting this artery, all of the branches and anastomosis must get appropriately clipped. Failure to clip the superior thoracic can theoretically result in hemithorax during the postoperative period.
In conclusion, clinicians should suspect superior thoracic artery injury in patients presenting with penetrating injuries and pleuritic chest pain. A high degree of suspicion is crucial as patients may present with tachycardia, tachypnea, and hypotension without evidence of external bleeding or hematoma. These patients may present with other pressing concerns, including pneumothorax. Although a chest radiograph is usually the first imaging modality used, a neck computed tomographic angiography (CTA) is the gold standard for diagnosing these injuries. A CTA with contrast showing a hematoma posterior to the clavicle suggests the involvement of this artery.[6]
Media
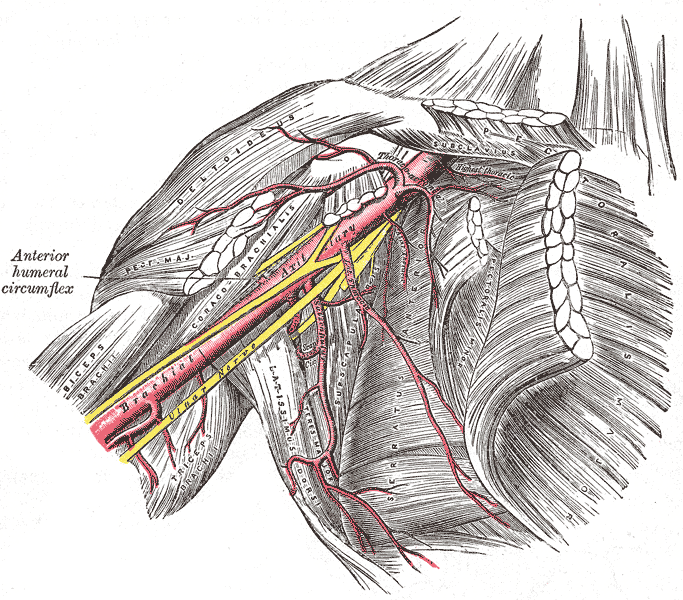
(Click Image to Enlarge)
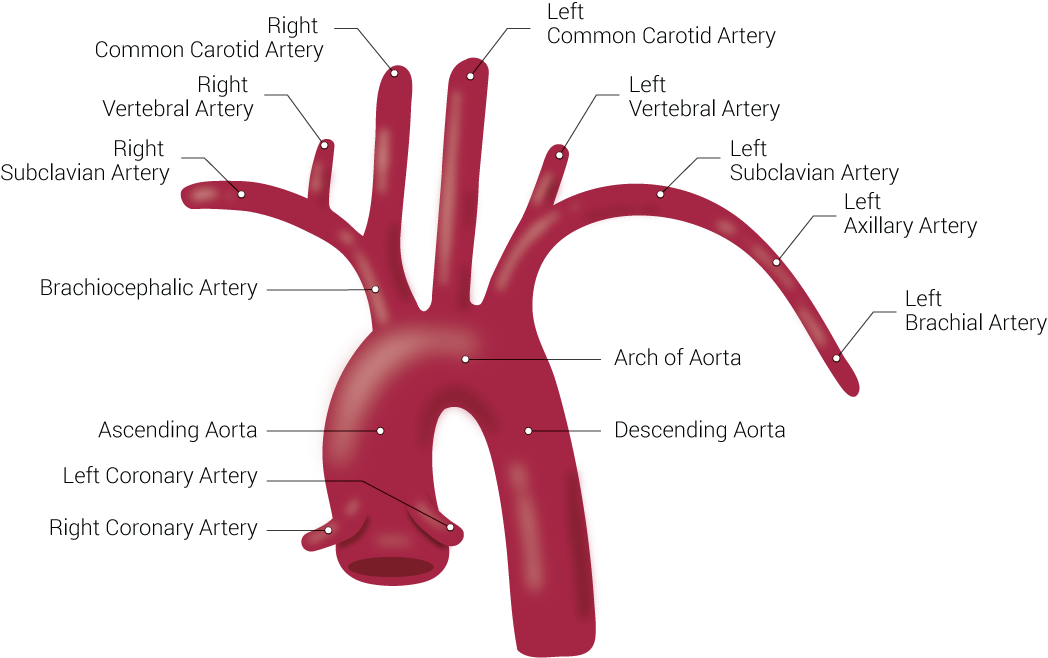
Branches of the Aorta. This illustration includes the right common carotid artery, right vertebral artery, right subclavian artery, brachiocephalic artery, ascending aorta, left coronary artery, right coronary artery, left common carotid artery, left vertebral artery, left subclavian artery, left axillary artery, left brachial artery, arch of aorta, and descending aorta.
Contributed by Beckie Palmer
(Click Image to Enlarge)
References
Shahoud JS, Kerndt CC, Burns B. Anatomy, Thorax, Internal Mammary (Internal Thoracic) Arteries. StatPearls. 2023 Jan:(): [PubMed PMID: 30726022]
Rodríguez-Niedenführ M, Burton GJ, Deu J, Sañudo JR. Development of the arterial pattern in the upper limb of staged human embryos: normal development and anatomic variations. Journal of anatomy. 2001 Oct:199(Pt 4):407-17 [PubMed PMID: 11693301]
Iimura T, Pourquié O. Hox genes in time and space during vertebrate body formation. Development, growth & differentiation. 2007 May:49(4):265-75 [PubMed PMID: 17501904]
Level 3 (low-level) evidenceAastha, Jain A, Kumar MS. An unusual variation of axillary artery: a case report. Journal of clinical and diagnostic research : JCDR. 2015 Jan:9(1):AD05-7. doi: 10.7860/JCDR/2015/11680.5477. Epub 2015 Jan 1 [PubMed PMID: 25737968]
Level 3 (low-level) evidenceBagoji IB, Hadimani GA, Bannur BM, Patil BG, Bharatha A. A unique branching pattern of the axillary artery: a case report. Journal of clinical and diagnostic research : JCDR. 2013 Dec:7(12):2939-40. doi: 10.7860/JCDR/2013/5883.3795. Epub 2013 Dec 15 [PubMed PMID: 24551680]
Level 3 (low-level) evidenceWong VW, Gordy SD, Schreiber M, Tieu BH. Penetrating neck injury to the superior thoracic artery managed by video-assisted thoracoscopic surgery. Case reports in surgery. 2013:2013():413462. doi: 10.1155/2013/413462. Epub 2013 Feb 7 [PubMed PMID: 23476874]
Level 3 (low-level) evidenceUchikado Y, Yoshino S, Ohmure K, Tabata H, Tateishi S, Ohishi M. Angle-tipped guidewire-induced vascular perforation at branch of superior thoracic artery during sheath insertion: Case report. Journal of cardiology cases. 2017 Nov:16(5):158-161. doi: 10.1016/j.jccase.2017.07.007. Epub 2017 Aug 23 [PubMed PMID: 30279824]
Level 3 (low-level) evidenceButurak A, Demirci Y, Dağdelen S. Management of an iatrogenic radial artery perforation: a case report. Turk Kardiyoloji Dernegi arsivi : Turk Kardiyoloji Derneginin yayin organidir. 2013 Jun:41(4):332-5. doi: 10.5543/tkda.2013.56957. Epub [PubMed PMID: 23760121]
Level 3 (low-level) evidenceKaufman J, Moglia R, Lacy C, Dinerstein C, Moreyra A. Peripheral vascular complications from percutaneous transluminal coronary angioplasty: a comparison with transfemoral cardiac catheterization. The American journal of the medical sciences. 1989 Jan:297(1):22-5 [PubMed PMID: 2521545]
Level 3 (low-level) evidenceDar MI, Dar AH, Bilal M, Ahmad M, Haseeb A. Association of Internal Mammary Artery Flow with Different Comorbidities and Post-Coronary Artery Bypass Graft Complications. Cureus. 2017 Aug 20:9(8):e1584. doi: 10.7759/cureus.1584. Epub 2017 Aug 20 [PubMed PMID: 29062616]