 Anatomy, Head and Neck: Eye Superior Oblique Muscle
Anatomy, Head and Neck: Eye Superior Oblique Muscle
Introduction
The superior oblique is one of the two noteworthy oblique extraocular muscles. These muscles are unique in that they do not originate from the common tendinous ring, have an angular attachment to the eyeball, and they attach to the posterior aspect of the eyeball. The superior oblique functions explicitly to move the eye in the down-and-out position and intort the eye.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The superior oblique muscle attaches to the trochlea—a fibrous, cartilaginous pulley attached to the trochlear fovea of the frontal bone. Originating from the periosteal covering of the sphenoid, the superior oblique reaches the trochlea by passing along the medial border of the roof of the orbit. Upon reaching the trochlea, the superior oblique tendon turns posterolaterally to cross the eyeball and continues to reach its insertion point on the outer posterior quadrant of the eyeball.[1] [2]
This unique path of the superior oblique muscle allows the eye to distinctively move down and out (i.e., inferolaterally) when contracted. However, under normal circumstances, this muscle does not act in isolation, and instead, its movements combine with other extraocular muscles. One such combined movement is the depression of the eye when the medial rectus has adducted the eye. Depression of the eye is normally the function of the inferior rectus muscle; however, adduction of the eye neutralizes the mechanical positioning of the inferior rectus.[3][4]
Embryology
The development of the superior oblique muscle is not unique when compared to the other extraocular muscles. Nevertheless, these extraocular muscles are unique when compared to periocular tissues in that these muscles arise from paraxial mesoderm in the prechordal plate, and not neural crest cells like their connective tissue tendons.[5] The superior oblique muscle appears at week 6 of development along with the medial rectus, while most other extraocular muscles appear at week 5.
The unique pulley action of the superior oblique along the trochlea is due to the specialized development of the muscle. Embryologic studies show that at the early stage of development, the muscle itself, the insertion tendon, and the cartilaginous pulley travel together in a straight line. At around 12 weeks, the tendon then begins to turn around the trochlear cartilage, creating the pulley action.[6]
Blood Supply and Lymphatics
The ophthalmic artery, which branches off the internal carotid artery, supplies the majority of the bloody supply to the orbit and extraocular muscles. The superior oblique muscle gets its vascular supply from the lateral muscular branch of the ophthalmic artery, which also gives blood to the lateral and superior rectus muscles as well as the levator palpebrae superioris muscle. The ophthalmic artery also branches into the medial muscular branch, which supplies blood to the remaining extraocular muscles.[7]
Venous drainage of the superior oblique muscle is similar to the remaining extraocular muscles. Deoxygenated blood from the muscles first reaches the four vortex veins arising from the posterior aspect of the eye then empties into the superior and inferior orbital veins. The orbital veins, also known as the ophthalmic veins, then drain into the cavernous sinus.
Nerves
Innervation of the superior oblique muscle is distinct from the remaining extraocular muscles in that its nerve supply is from the trochlear nerve (CN IV). Most of the remaining extraocular muscles are innervated by the oculomotor nerve (CN III), except for the lateral rectus, which receives innervation via the abducens nerve (CN VI).[4][8] The trochlear nerve originates at the level of the inferior colliculus from the dorsal surface of the medial midbrain. It enters the orbit outside of the annulus and travels superior to the oculomotor nerve in the lateral cavernous sinus and inserts on the lateral border of the superior oblique muscle.[8] The tumultuous course of the trochlear nerve increases its susceptibility to damage due to vascular disease or tumors, resulting in a superior oblique muscle palsy.
Muscles
The superior oblique muscle originates above the annulus of Zinn, which is the origin site for most of the other extraocular muscles. The muscle itself travels along the superomedial orbital wall; however, its cord-like tendon is what passes through the trochlea and turns at an approximately 53-degree angle in the posterolateral direction sagittally. It then fans out and inserts on the sclera in the superotemporal quadrant.
The tendon of the superior oblique is thin and extends posteriorly for approximately 11 mm. The insertion point of the tendon is about 6 to 7 mm from the optic nerve (CN I). One unique aspect of this tendon is its relation to the superior temporal vortex vein, which exits temporally to the insertion of the superior oblique but can also split the fibers of the insertion and pass through them.
The superior oblique muscle is made up of similar muscle types to the remaining extraocular muscles, a particular type of skeletal muscle which contains a combination of type I, slow fibers, and type II, rapid fibers. Also, extraocular muscles, including the superior oblique, possess a higher ratio of nerve fibers to skeletal muscle fibers when compared to other skeletal muscles.[9]
Physiologic Variants
Physiologic variations between individuals exist when discussing specific measurements of the superior oblique muscle. Certain measurements, such as the size of the muscle, the length of the tendon, the insertion point, and the angle the muscle takes upon approaching the trochlea may differ from individual to individual. Furthermore, as discussed above, the superior temporal vortex vein differs in its path relative to the superior oblique muscle when comparing individuals, passing either through or around the muscle.
Surgical Considerations
The complex anatomy and function of the superior oblique muscle and tendon make surgery on these structures quite challenging. One surgical consideration is the requirement of an incision through the conjunctiva and through Tenon’s fascia, a connective tissue capsule that attaches to the optic nerve posteriorly and is pierced by most extraocular muscles, including the superior oblique, to access the episcleral space. Excessive damage to this fascia may cause adhesions, which may limit eye movement.
Factors to consider when starting surgery are noting the most common sites of infection, which are the patient’s skin, lid margins, and conjunctiva. Infection of these sites can cause serious postoperative complications, therefore cleansing these structures with an antimicrobial solution in advance of surgery is vital.[10]
Clinical Significance
Assessment of all the extraocular muscles is usually done clinically by having the patient follow the clinician’s finger in the shape of an “H” in the air. Isolated testing of the superior oblique muscle is by having the patient look down and in. Although the specific function of the superior oblique is the movement of the eye in the down and out direction, it is challenging to isolate the function of the superior oblique by having the patient look in this direction due to the contributions of the lateral rectus and inferior rectus. Instead, as mentioned above, the superior oblique is tested by having the patient look down and in. By canceling the action of the inferior rectus muscle via contraction of the medial rectus, one can isolate the action of the superior oblique.
Strabismus is a condition that can present in childhood as acquired paralytic strabismus and is usually due to malfunction of one or more of CN III, IV, and VI, resulting in ocular misalignment. Specific malfunction of CN IV results in paralysis of the superior oblique muscle, which leads to hypertropia, an upward deviation of the eye due to unopposed action of the superior rectus muscle, usually during contralateral gaze.[11] For example, a patient with right CN IV palsy may have right hypertrophia when looking to the left. Strabismus surgery may be performed to correct the misalignment of the eyes. Surgical options include loosening, tightening, or repositioning of the muscle.[7]
Superior oblique palsy is another condition that may be caused by damage to CN IV. Damage to CN IV may occur due to vasculopathy, tumor, or trauma. This palsy commonly presents as difficulty looking downwards. Therefore, a presenting patient may complain of problems when descending stairs or reading a book.[3] Patients may complain of verticle diplopia when looking downwards or contralaterally. Tilting head to the opposite side may help decrease double vision. Tilting head to the affected side worsens double vision.
Media
(Click Image to Enlarge)
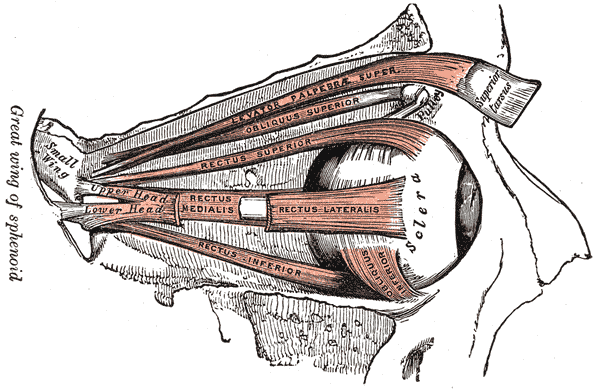
Orbital Muscles. This image shows the anatomical relationships between the levator palpebrae superioris, superior and inferior obliques, and superior, lateral, inferior, and medial recti. The sphenoid's greater wing, the sclera, and the superior tarsus are also referenced.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Shin A, Yoo L, Chaudhuri Z, Demer JL. Independent passive mechanical behavior of bovine extraocular muscle compartments. Investigative ophthalmology & visual science. 2012 Dec 19:53(13):8414-23. doi: 10.1167/iovs.12-10318. Epub 2012 Dec 19 [PubMed PMID: 23188730]
Level 3 (low-level) evidenceKels BD, Grzybowski A, Grant-Kels JM. Human ocular anatomy. Clinics in dermatology. 2015 Mar-Apr:33(2):140-6. doi: 10.1016/j.clindermatol.2014.10.006. Epub [PubMed PMID: 25704934]
Lawden M. The superior oblique muscle and its disorders. Practical neurology. 2018 Oct:18(5):348-349. doi: 10.1136/practneurol-2018-001994. Epub [PubMed PMID: 30217956]
Demer JL. Compartmentalization of extraocular muscle function. Eye (London, England). 2015 Feb:29(2):157-62. doi: 10.1038/eye.2014.246. Epub 2014 Oct 24 [PubMed PMID: 25341434]
Level 3 (low-level) evidenceZiermann JM, Diogo R, Noden DM. Neural crest and the patterning of vertebrate craniofacial muscles. Genesis (New York, N.Y. : 2000). 2018 Jun:56(6-7):e23097. doi: 10.1002/dvg.23097. Epub 2018 Apr 16 [PubMed PMID: 29659153]
Katori Y, Rodríguez-Vázquez JF, Kawase T, Murakami G, Cho BH, Abe S. Early fetal development of hard tissue pulleys for the human superior oblique and tensor veli palatini muscles. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2011 Mar:193(2):127-33. doi: 10.1016/j.aanat.2011.01.004. Epub 2011 Jan 26 [PubMed PMID: 21334866]
Ludwig PE, Aslam S, Czyz CN. Anatomy, Head and Neck: Eye Muscles. StatPearls. 2023 Jan:(): [PubMed PMID: 29262013]
René C. Update on orbital anatomy. Eye (London, England). 2006 Oct:20(10):1119-29 [PubMed PMID: 17019410]
Janbaz AH, Lindström M, Liu JX, Pedrosa Domellöf F. Intermediate filaments in the human extraocular muscles. Investigative ophthalmology & visual science. 2014 Jul 15:55(8):5151-9. doi: 10.1167/iovs.14-14316. Epub 2014 Jul 15 [PubMed PMID: 25028355]
Patel CC, Goldenberg DT, Trese MT, Walsh MK, OʼMalley ER. Subretinal abscess after strabismus surgery: case report and literature review. Retinal cases & brief reports. 2011 Winter:5(1):6-9. doi: 10.1097/ICB.0b013e3181babedb. Epub [PubMed PMID: 25389671]
Level 3 (low-level) evidenceBagheri A, Fallahi MR, Abrishami M, Salour H, Aletaha M. Clinical features and outcomes of treatment for fourth nerve palsy. Journal of ophthalmic & vision research. 2010 Jan:5(1):27-31 [PubMed PMID: 22737323]
