Introduction
Colorectal cancer (CRC) is the world's fourth leading cause of death. It has links with inappropriate food habits such as low consumption of fruits, vegetables, fiber, fish, vitamin C, dairy products, and vitamin D, and high consumption of foods containing heme-iron (red and processed meat). Moreover, other factors that increase its incidence include poor lifestyles such as high alcohol consumption, obesity, and lack of exercise. The inherited CRC syndromes are a series of diseases that have specific mutations that predispose to CRC. These are more aggressive and have a worse prognosis since they correlate with other tumors, and some do not respond to chemotherapy.
Early diagnosis is challenging for physicians due to the absence of pathognomonic clinical findings. The evidence shows that 50% of the patients are asymptomatic and usually present with symptoms (such as rectal bleeding, weight loss, and intestinal obstruction) when the disease is already advanced. Familial adenomatous polyposis (FAP) and syndromes not associated with polyposis, such as Lynch syndrome, are the most common cause of the onset of hereditary syndromes. When considered together, they represent 6% to 10% of all cases of CRC.[1]
Estimates are that tumors found in young adults are related to hereditary CRC syndromes. This article will review the most common genetic syndromes in the development of CRC and the medical-surgical treatment approach according to current evidence.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Hereditary colorectal cancer (HCRC) is not a single disease; it is a group of diseases or syndromes with a mutational genetic component; these generate a clinically differentiated phenotype. It subdivides into two large HNPCC groups and the HPCC:
Hereditary non-polyposis colorectal cancer (HNPCC) is an autosomal dominant cancer syndrome; the incidence of this syndrome is 1.7 to 4.2% among all CRCs patients (represents 3 to 8 cases per million inhabitants in the world, according to Globocan 2018).[2][3][4][3]
- Lynch syndrome (LS) is the commonest of hereditary cancers and correlates with an increased risk of colorectal, endometrium, ovary, stomach, and small bowel cancer. LS has associations with mutations of DNA mismatch repair (MMR)as MLH1(76%), MSH2(40%), MSH6, PMS2, and EPCAM.[5] LS is incidence represents 3 to 5 cases per million inhabitants, according to Globocan 2018).[6]
- Sporadic colorectal carcinomas, MLH1-/PMS2-deficient.[7]
- Muir-Torre syndrome:( The genes most commonly mutated MLH1, MSH2, MSH6, and PMS2). Its incidence represents 2 cases per ten million inhabitants, according to Globocan 2018).[8]
- Turcot syndrome type I: The frequency is approximately 20% to 25% among all TS. It is related to mutations of the MMR gene.[9]
Hereditary polyposis colorectal cancer (HPCC) accounts for approximately 3 to 5 % of all CRC cases.[10][11] (represents 5 to 9 cases per million inhabitants globally, according to Globocan 2018).
- Familial adenomatous polyposis (FAP) is related to the germline mutations of the APC gene. FAP incidence represents 2 to 3 cases per million inhabitants, according to data from the Danish Polyposis Registry 2017.[12]
- Adenomatous polyposis syndromes (APC and MUTYH).[13]
- Juvenile polyposis coli: (BMPR1A and SMAD4).[14] It is estimated the incidence of 1 per one million inhabitants.[15][16]
- Peutz-Jeghers syndrome: (STK11/LKB1), is incidence represents 1.2 per one million inhabitants.[17][18]
- PTEN hamartoma tumor syndrome: (PHTS; PTEN).[19]
- Cowden syndrome:(affecting the PTEN-gene).[20] It is incidence represents 6 cases per ten million inhabitants.[21][22][23]
- Turcot syndrome type II: The frequency is approximately 75% to 80% among all TSs. It is related to the APC gene mutation.[24]
- Gardner syndrome: (involved APC gene).[25] It is incidence represents 1 per one million people within the United States.[25]
Epidemiology
Colorectal cancer (CRC) is the third most common cancer and the fourth most common cause of cancer-related mortality globally. The estimated age-standardized incidence and mortality rates in 2018 worldwide for both sexes of all ages is 19.7 per 100000 inhabitants, and the mortality rate is 8.9 per 100000 patients, according to Globocan. The incidence increases significantly by six times when it is related to obesity.[26] The hereditary CRC occurs in those individuals with a family history of colorectal cancer with familial adenomatous polyposis or hereditary nonpolyposis colorectal cancer, the most common being Lynch syndrome.[5]
These are detected in 6% to 10% of all CRC diagnosed before age 50; that is, its incidence would be 2 per 100000 inhabitants in the world population.[1][27][1] The risk of advanced neoplasia after a small tubular adenoma in the initial colonoscopy is four times higher in patients with a positive fecal immunochemical test.[28] Additionally, the relative risk of colorectal cancer is higher when patients have a history of colon cancer than rectal cancer.[29]
Pathophysiology
The mutational mechanisms associated with CRC are:
Genomic Instability
- Instability Chromosome: is the most common type found in 85% of the CRCs.[30] This mutation causes the loss of heterozygosity in tumor suppressor genes and mutations in proto-oncogenes.[31] Mutations affect the following genes: APC, TP53, and K-ras, allelic loss of 18q, and aneuploidy. For example, FAP develops cancer from this route (CRC risk 90% without colectomy and risk of extracolonic cancers 10 to 99 adenomas).[32] There are many mutations in the APC gene (a large “housekeeping” gene), including micro-deletions and frameshift mutations. More than 60% of the mutations are present at the 5′ ends of the exon on the 5q21 chromosome.[33]
- Microsatellite instability: It is present in 15% of CRC.[30] It is caused by errors in the repair system due to DNA damage (MMR), mainly due to failure in base complementarity, which generates the expansion of short sequences in tandem and increases the number of mutations. The MMR system is made up of seven genes: hMLH1, hMLH3, hMSH2, hMSH3, hMSH6, hPMS1, and hPMS2; Currently, more than 500 different mutations have been described.[34] For example, LS progresses to cancer from the aforementioned (Lifetime risk of CRC 70%).[32] Cumulative incidence at 75 years for colorectal cancer were 46%, 43%, and 15% in path MLH1, MSH2, and MSH6 carriers, respectively.[35]
Epigenetic (DNA methylation) Methylation of CpG islands occurs in sporadic CRC 15%, and also it affects the expression of DNA repair genes or Mismatch genes.[36][37]
History and Physical
We will focus on the two most frequent pathologies of hereditary colorectal cancer according to the polyposis classification:
HNPCC - Lynch syndrome (LS): Characteristically presents with flat polyps located in the right colon, which generate CRC and other cancers (endometrium, stomach, ovary, pancreas, ureter and renal pelvis, cerebral glioblastoma, biliary tract, cancer of the small intestine, sebaceous carcinomas and keratoacanthomas). Endometrial cancer occurs in relatively young women.[38] The diagnosis is challenging for the doctor due to the absence of pathognomonic clinical signs. A genetic study is required to establish the definitive diagnosis, so it is recommended to make a previous selection of these patients with the criteria of Bethesda and Amsterdam.[39]
HPCC) - Familial adenomatous polyposis (FAP): It is characterized by hundreds or thousands of precancerous adenomatous polyps, which generate CRC and other cancers, Also may occur extracolonic manifestations (desmoid tumor, osteomas, epidermoid cysts, papillary thyroid carcinoma, pancreatic carcinoma, gastric cancer, duodenal cancer, hepatobiliary and CNS tumors), this is due to mutations in the gene (APC), which controls cell proliferation and the regulation of a new long non-coding RNA (lncRNA).[40] It is classified clinically in two ways:
- Classic FAP: Consists of the involvement of the entire colon with the appearance of 100 to 1000 adenomatous polyps, the age of onset of polyps comprises between 10 and 20 years of age; estimates are that the diagnosis of CRC corresponds to 30 to 40 years of age, It correlates with the majority of cancers described above, which increases comorbidity.[41][42]
- Attenuated FAP: Frequently affects the right colon, with an appearance of 10 to 100 adenomatous polyps, the age of onset of polyps between 20 to 30 years of age; estimates are the diagnosis of CRC corresponds to 40 to 50 years of age. It commonly carries associations with gastric, duodenal, and thyroid cancer.[43][44]
Evaluation
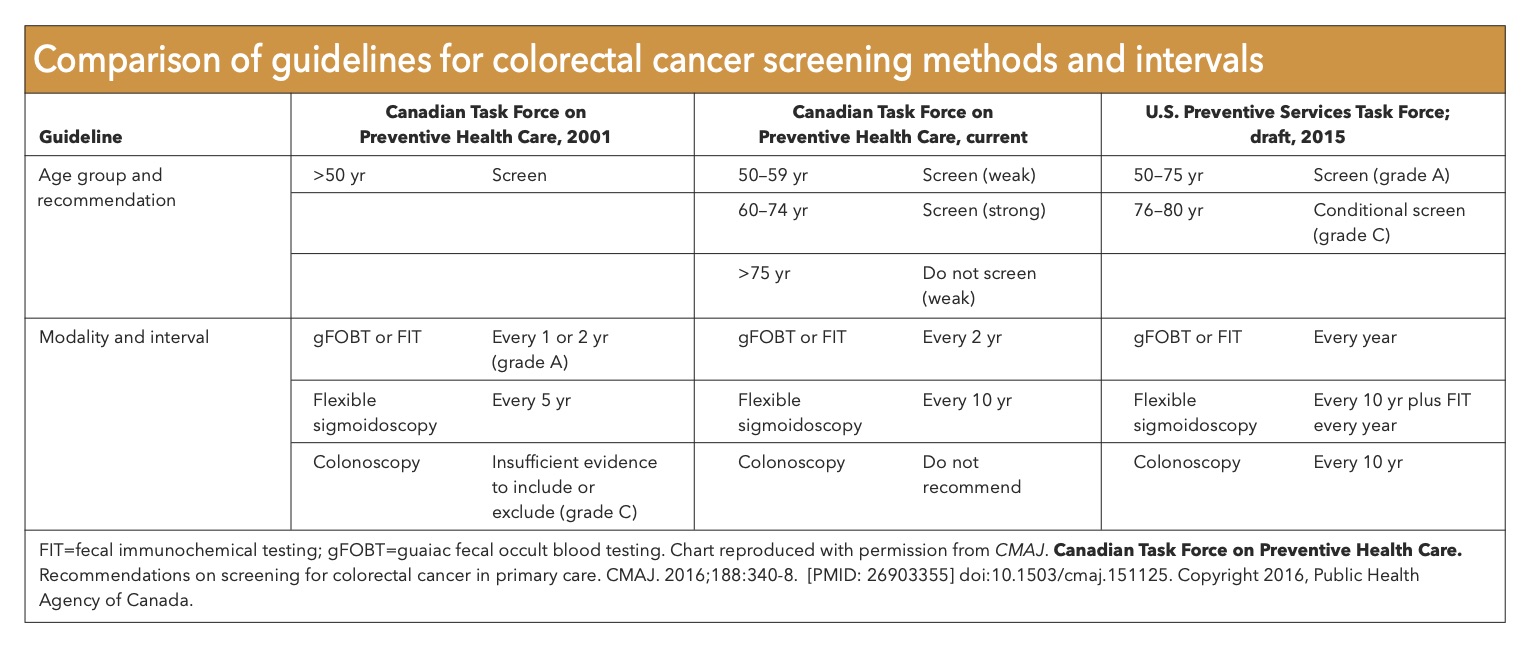
The diagnostic basis of hereditary CRC is from clinical findings, family history, genetic tests, and diagnostic images (see Table. Colorectal Carcinoma Screening Guidelines).
Physical examination: Should include evaluation of adenopathies, mainly supraclavicular, cervical and axillary, digital rectal examination, abdominal palpation in search of masses or ascites, hepatomegaly suggesting a hepatic metastatic compromise.
Total colonoscopy: It is a gold standard technique since it allows the resection and biopsy of the lesions observed during the procedure.[45] Moreover, endoscopy with a colonic capsule is a promising technique for noninvasive colon screening; however, it is a risk to detect polyps and not be able to biopsy them.[46]
Family history: more than one criterion raises suspicion of LS.
- Modified Bethesda criteria, which are:
- Patients with CRC belong to families that meet the criteria of Amsterdam
- Patients with two neoplasms associated with HNPCC, including synchronous or metachronous CRC and extracolonic cancer (endometrium, ovary, gastric, hepatobiliary, small intestine, ureter, or renal pelvis)
- Patients with CRC and a first-degree relative with CRC, extracolonic neoplasm associated with HNPCC or colorectal adenoma; one of the cancers diagnosed before 50 and the adenoma before 40 years of age
- Patients with CRC or endometrial cancer are diagnosed before 50 years of age
- Patients with CRC in the right colon and histologically undifferentiated are diagnosed before 50
- Patients with CCR-type cells in the signet ring (composed of more than 50% of signet ring cells) were diagnosed before 50
- Patients with colorectal adenoma are diagnosed before 40 years of age[47]
- Amsterdam criteria II, which are:
- Three or more relatives affected by a neoplasm associated with HNPCC (CRC, cancer of the endometrium, small intestine, ureter, or renal pelvis), one of them being a first-degree relative of the other two, and;
- Two or more successive generations were affected, and;
- One or more relatives affected by CRC were diagnosed before 50 years of age, and;
- Exclusion of FAP in cases of CCR.[48]
Molecular and genetic testing: LS Diagnosis is made by tumor testing with MMR immunohistochemistry and PCR for MSI (microsatellite instability), a genetic phenotype that characterizes these tumors. Therefore, having a positive genetic test (MSI), a positive Bethesda or Amsterdam item, and the tumor located on the right side of the colon are highly suspicious findings of Lynch syndrome.[49] When colonic polyposis presents in a single person with a negative family history, consideration should be to test for a de novo APC mutation; if negative, follow with MUTYH genetic testing when colonic polyposis is present only in siblings, consider recessive inheritance, and test for MUTYH first.[40]
Diagnostic Imaging: It is suggested to perform computed tomography with the contrast of the chest, abdomen, and pelvis to estimate the stage of the disease in all patients with colorectal cancer. Additionally, It is suggested to perform computed tomography or magnetic resonance imaging of the pelvis to assess the status of the mesorectal margin in selected cases.
Specific aspects of individuals' family history of CRC would influence the age at which, planning to begin screening and the frequency of screening. Following details with the family history of the number of first-degree relatives should be considered before planning for a screening schedule;
- Established diagnosis of CRC
- Advanced polyp that harbors any of the following characteristics:
- Adenoma size of equal to or greater than 1 cm
- Presence of high-grade dysplasia
- Adenoma with a villous component
- Advanced sessile serrated lesion with any of the following characteristics:
- Sessile polyp with a size equal to or greater than 1 cm
- Serrated adenoma with equal or greater than 1 cm size
- Presence of dysplasia in a sessile serrated polyp
According to the response to the above questions, the following screening schedules are recommended. If equal to or more than one first-degree relative is affected, the screening is to be initiated either at the age of 40 or at the age equal to 10 years younger than the affected FDR, whichever comes earlier. Moreover, a continuous schedule plan with either colonoscopy every five years or annual fecal immunochemical testing (FIT) are recommended.
Consequently, if the first-degree relative has a polyp without a well-established tissue diagnosis of either an advanced adenoma or a serrated polyp, the individual would be categorized as average risk.
High-Risk Syndrome Screenings
Specific screening schedules should be planned for individuals with Lynch-associated cancers. The schedule should be organized based on the following characteristics; 1. personal and family history of cancer, 2. the gene affected, and 3. the mode of ascertainment of the familial mutation. According to some expert opinions, and due to the significantly lower lifetime cancer risk for carriers of germline PMS2 mutations, screening recommendations must be tailored to the MMR gene alone. Moreover, a later mean age of colorectal cancer (CRC) onset in germline MSH6 carriers should dictate a modified screening schedule.
Collectively, screening is recommended for the following individuals considering the Lynch-associated cancers:
- Individuals with either a pathogenic germline mutation in the DNA mismatch repair (MMR) genes or epithelial cellular adhesion molecule (EPCAM) deletions that can inactivate Mutation S Homolog 2 (MSH2)
- Individuals at risk for Lynch syndrome, including individuals in families meeting Amsterdam I or II criteria and individuals meeting revised Bethesda guidelines
- High-risk individuals with an equal or greater than 2.5 to 5 % risk for MMR mutation according to the prediction models[50]
Treatment / Management
Management of patients with HCCR is multidisciplinary and mainly stems from patients' specific findings.
Chemotherapy: Depending on their genetic mutation, hereditary CRCs may respond differently to traditional chemotherapy regimens. The microsatellite instability in many cases reflects a difference in the biological characteristics of the tumor, possibly with a unique susceptibility to immunotherapy.[51][52] High-risk rectal cancers require neoadjuvant chemotherapy along with radiotherapy.[53] (B3)
- Current ASCO, NCCN, and ESMO guidelines strongly recommend adjuvant therapy for selected stage II with high-risk/pMMR/MSI-S disease and all stage III (node-positive). The guidelines advocate administering adjuvant chemotherapy (FOLFOX or CAPOX) within 6 to 8 weeks after surgical resection, pending recovery of the patient's health.
- FOLFOX (5-fluorouracil plus + leucovorin plus +oxaliplatin) is the first-line modern chemotherapy for metastatic disease more effective than the obsolete single-agent chemotherapy (5-fluorouracil) (HR for SLP: 0.59, 95% CI 0.49 to 0.73, 2 RCT), (HR for OS: 0.69, 95% CI 0.51 to 0.94, 1 RCT).[54]
- FOLFIRI (5-fluorouracil plus + leucovorin plus + irinotecan) is the second most effective chemotherapy in metastatic CRC and is either first or second line. (HR for OS: 0.58, 95% CI 0.43 to 0.80, 1 RCT).
- Combinations based on irinotecan were more effective than irinotecan alone (HR for PFS: 0.68, 95% CI 0.60 to 0.76, 6 RCT) [Level II]. Targeted agents increased the efficacy of conventional chemotherapy when considered together (HR for OS: 0.84, 95% CI 0.77 to 0.91, 6 RCT) and when bevacizumab alone (HR for PFS: 0.67, 95% CI 0.60 to 0.75, 4 RCT).[54]
- In metastatic colorectal cancer, monoclonal antibodies are used (bevacizumab, cetuximab, and panitumumab) in combination with chemotherapy. There is a distinct benefit in the addition of bevacizumab to chemotherapy for tumors on the right side of cetuximab to chemotherapy for tumors on the left side (for RAS wild-type tumors) to oxaliplatin- and irinotecan-based regimens which can be a consideration for first-line therapy.[55]
- A meta-analysis including the TAILOR and the PRIME study suggests that primary tumor location predicted a survival benefit when adding the anti-epidermal growth factor receptor antibody to FOLFOX regimen in RAS & NRAS-wild metastatic CRC patients (OS, HR for left-sided: 0.71; 95% CI: 0.59-0.85; P=.0002 and HR for right-sided: 0.90; 95% CI: 0.65-1.25; P=.53). The efficacy was similar in patients with wild molecular characteristics RAS / BRAF.[56] (A1)
Radiotherapy: Preoperative radiotherapy (hypofractionated) with chemotherapy is recommended in patients with stage II and III rectal cancer or unresectable residual tumor (positive margins), according to the report of anatomopathological findings of the surgical specimen.[57] The use of radiotherapy is limited to palliative therapy for selected cases of metastasis (bone, brain).[58] (B2)
Surgery: The appropriate surgical option for patients with colon cancer and LS (total abdominal colectomy or segmental colectomy with ileorectal anastomosis) will depend on the risk factors. The surgical preferences of the patient, with special emphasis on the age of the patient and the capacity of the patient to follow intensive surveillance,[59] but currently, segmental resection is the most performed surgical method in these cases.[60] Also, patients should be offered the option of prophylactically extended surgery (hysterectomy and oophorectomy) if possible in postmenopausal women.[61][62] (A1)
In FAP, prophylactic colectomy is an important option to prevent CRC.[63] The preventive surgical approach is limited for patients with attenuated FAP, delayed colectomy time, and increased standardization of laparoscopic surgery.[64] However, surveillance and surgical management planning should follow a thorough assessment of familial cancer risk.[65]
Differential Diagnosis
Gardner syndrome: is a variant of FAP and is an autosomal dominant inherited disease characterized by multiple intestinal polyps together with extra-intestinal manifestations including multiple osteomas, connective tissue tumors, thyroid carcinomas, hypertrophied pigmented epithelium of the retina, and also frequent retained supernumerary teeth and odontomas.[25] This condition carries a high risk of developing colon cancer.[66]
Muir-Torre syndrome: MTS is a rare subtype of LS characterized by sebaceous neoplasms of the skin and visceral malignancies, with colonic carcinoma being the most common.[67]
Turcot syndrome: TS is the association of primary brain tumors. It divides into two subtypes: TS type I (Intestinal polyps are large, fewer in number than 100, and are apt to undergo a malignant change. Associated brain tumor is usually a glioblastoma or an astrocytoma.) and TS type II (Familial adenomatous polyposis-associated type. There is a predisposition to the development of medulloblastoma.)[68] Tumors can also arise from the spinal cord, manifesting with symptoms of spinal cord compression.[69]
Juvenile polyposis coli: JPC is a rare disease characterized by juvenile hamartomatous polyps in the gastrointestinal tract. The lifetime risk of CRC is 20%.[70] JPC is diagnosed with more than five juvenile polyps in the colon and/or rectum; the presence of juvenile polyps along the digestive tract, including the stomach; the presence of any number of juvenile polyps in association with a family history of JIP.[71] Clinical signs include isolated rectal bleeding, anemia, abdominal pain, intestinal invaginations, diarrhea, rectal prolapse, and spontaneous anal elimination of polyps in juvenile polyposis coli and generalized juvenile polyposis. Other associated signs may include growth retardation and edema.[72]
Peutz-Jeghers Syndrome: PJS is characterized by the pigmentation of mucocutaneous melanin and multiple gastrointestinal polyposes. The clinical manifestations mainly included black spots, abdominal pain, and anemia.[73] These polyps have a higher risk of developing GI cancers of the colorectal, pancreatic, and gastric organs, in addition to a wide variety of non-GI epithelial malignancies, such as cancers of the breast, uterus, cervix, and ovary, testicular, and lung (see Image. Breast Cancer Metastasis Sites). The lifetime risk of CRC is 39%.[74] Patients with PJS present a high risk of intussusception and should receive regular follow-up due to the high risk of cancer and the possibility of relapse.[75]
Hamartoma tumor syndrome: This is called PTEN (PHTS).[76] PTEN correlates with multiple benign diseases (macrocephaly, Hashimoto's thyroiditis, mucocutaneous hamartomas, colon polyps, and vascular malformations) and malignant tumors (breast, thyroid, renal, endometrial, and colon cancer),[76] as well as neurodevelopmental disorders such as autism.[77] PHTS patients may also demonstrate an increased risk of immunological dysregulation, including autoimmunity and immune deficiencies.[19]
Cowden syndrome: CS classically is characterized by multiple hamartomas that can occur in any organ, macrocephaly, mucocutaneous lesions, an increased risk of breast and thyroid cancers, and ovarian and colon cancer. The lifetime risk of CRC is 13%.[22][78]
Bannayan-Riley-Ruvalcaba syndrome: BRRS is a congenital disorder frequently characterized by hamartomatous intestinal polyps, lipomas, macrocephaly, and genital lentiginosis. BRRS patients with a PTEN mutation share the same risk of developing cancer as patients with CS.[79]
Proteus syndromes: PS is a disorder characterized by progressive excessive growth at the level of the skeleton, skin, fat, and central nervous system, with few hamartomatous polyps. Complications include hemimegaloencephaly, bullous lung disease, pulmonary embolism, and deep vein thrombosis. The tumors are usually benign, although there are reports of rare cases of malignant tumors.[80]
Solamen syndrome: The term 'SOLAMEN syndrome' "Segmental Overgrowth, Lipomatosis, Arteriovenous Malformation, and Epidermal Nevus." These patients are carriers of germline mutations in the phosphatase and PTEN homologs.[81]
Surgical Oncology
Surgical management should be planned considering the specific hereditary colorectal cancer. Accordingly, the treatment of choice for patients with attenuated and familial adenomatous polyposis, with a significantly large number of rectal adenomas, is proctocolectomy with ileostomy or ileal-pouch anal anastomosis (IPAA). However, the timing of treatment should be individualized. On the other hand, if all of the rectal adenomas greater than 5 mm in size can be removed endoscopically, rectal sparing alternatives with total colectomy with ileorectal anastomosis (TAC-IRA) is the preferred management. Moreover, in patients with greater than 20-lifetime adenomas, MUTYH-associated polyposis (MAP) should be considered. Accordingly, patients with biallelic MYH mutations are recommended for annual colonoscopy and polypectomy for polyps that can be removed endoscopically.[82]
Prognosis
In their study, Lee and his colleagues indicated that those with sporadic colorectal cancer (CRC) and a family history of CRC had better overall survival but a cancer recurrence similar to those who did not have a CRC family history.[83]
CRC survivors (5 to 10 years post-diagnosis) reported overall good health-related quality of life but significantly poorer social functioning and more problems with dyspnea, constipation, diarrhea, and finances than controls, mainly among younger subjects.[84]
Complications
Severe complications during colonoscopy represent the most important adverse effect of colorectal cancer screening programs. The immediate complication occurred in 3.3%, as perforation and hemorrhagic events. However, the following factors increase the risk of early and late complications, including a history of colon disease, a history of anticoagulation, a history of pelvic surgery or abdominal radiotherapy, and a history of perforation.[85]
After a total colectomy, systemic complications can occur in 22%, mainly in those older than 65 years, due to significant comorbidities, while the incidence of surgical complications was 8%, such as anastomotic leakage, major infections in the wound, and postoperative hemorrhage.[86]
Deterrence and Patient Education
There is a need for educational efforts to raise awareness about CRC, particularly among the young. There is also a need to improve adherence to screening in young patients eligible for screening and to emphasize early evaluation of symptoms. These are essential steps to decreasing the burden of CRC in younger patients.[87]
Good lifestyle and dietary habits are recommended to reduce the most critical factor in colorectal carcinogenesis starting in the early stages of life.[88]
Enhancing Healthcare Team Outcomes
An interprofessional approach includes a gastroenterologist, oncologist, colorectal surgeon, primary care provider, nurse practitioner (physician and mid-level practitioners), geneticist, nurse genetics counselor, other nursing staff, and pharmacist. Consider offering genetic testing to people with suspected hereditary colorectal cancer and their family members after genetic counseling.[89] Suggestions are that in individuals with a family history in the first degree of classical FAP, the screening strategy is annual colonoscopy from 12 to 15 years, up to 30 to 35 years of age, and then it is suggested to continue screening every five years.[90][91]
- In the population with suspicion or family history of HNPCC, suggestions are that the screening strategy is a colonoscopy every two years, from 20 to 25 years, or five to ten years before the age of the youngest case diagnosed in the family.[92][93]
- Studies consistently report that registration and screening reduce CRC incidence and mortality in patients with FAP and LS.[94] [Level 2]
- The MSI test is an effective screening test for Lynch syndrome. However, it must correlate with the panel of markers used or the thresholds used to denote a positive test.[95] [Level 2]
- The studies indicate that in adenomatous polyposis coli patients with APC promoter, hypermethylation is an early event in carcinogenesis of CRC and could be a valuable diagnostic marker for early-stage CRC.[96][97] [Level 2]
- Currently, the evidence of chemoprevention is for NSAIDs, sulindac, and aspirin in low doses that reduce the progression of polyps and the long-term incidence of colorectal cancers in patients with FAP and HNPCC, respectively.[98] [Level 2]
- Strict vigilance is necessary for the syndromes associated with CCR and extracolonic manifestations, especially LS with endometrial cancer, as well as those mentioned in the differential diagnosis section.[99]
- The risk factors that increase mortality are advanced age, male sex, African-American race, elevated CEA, and not undergoing curative surgery. Likewise, patients with CRC have an association with an increased risk of cardiovascular death, especially during the first year after diagnosis.[100] [Level 2]
- Overall, FOLFOX was the most effective first-line treatment [Level I], and FOLFIRI plus cetuximab (KRAS/NRAS wild) was the most effective treatment in terms of long-term survival, Wang and colleagues, in their analysis of 75 RCTs published after 1997. This treatment is preferable for patients with CRC in clinical practice.[101] [Level 1]
- The use of bevacizumab represents hope for increased survival and a chance of metastasectomy for patients with metastatic CRC. However, serious adverse events are associated with its use, especially severe hypertension and gastrointestinal perforation, that merit consideration.[102] [Level 1]
- The treating physician should recommend a diet rich in dietary fiber because it decreases CRC risk and post-operative relapses.[103][104][105] Currently, there is inadequate data to support the benefits of exercise in the field of colorectal surgery.[106][107] [Level 3]
Irrespective of the path of treatment (chemotherapy, surgery, etc.), all members of the interprofessional team must follow the patient, off counsel, and alert other team members as necessary when they note a change in the patient's status, including adverse drug events or therapeutic failure or relapse, recording their observations in the patient's medical record. This way, the appropriate measures can be taken to change the treatment regimen to optimize patient outcomes. The interprofessional approach to patient care will benefit the patient and ensure proper therapeutic care. [Level 5]
Media
(Click Image to Enlarge)
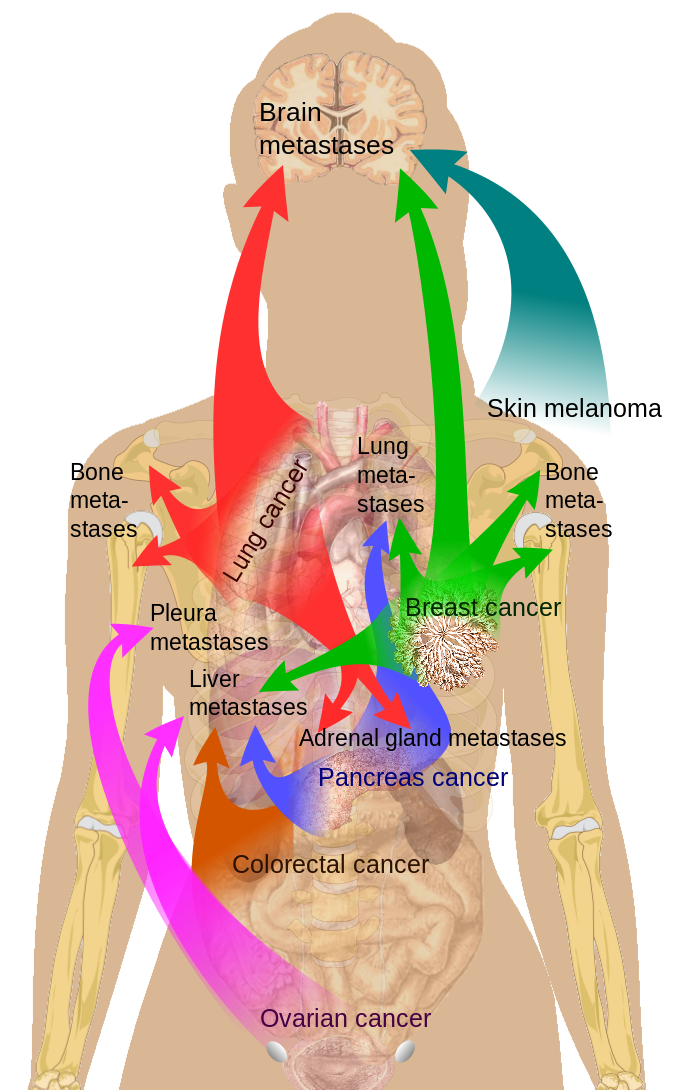
Breast Cancer Metastasis Sites
Medical Gallery of Mikael Häggström, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Valle L, Vilar E, Tavtigian SV, Stoffel EM. Genetic predisposition to colorectal cancer: syndromes, genes, classification of genetic variants and implications for precision medicine. The Journal of pathology. 2019 Apr:247(5):574-588. doi: 10.1002/path.5229. Epub 2019 Feb 20 [PubMed PMID: 30584801]
Katballe N, Christensen M, Wikman FP, Ørntoft TF, Laurberg S. Frequency of hereditary non-polyposis colorectal cancer in Danish colorectal cancer patients. Gut. 2002 Jan:50(1):43-51 [PubMed PMID: 11772966]
Lee J, Xiao YY, Sun YY, Balderacchi J, Clark B, Desani J, Kumar V, Saverimuthu A, Win KT, Huang Y, Xu Y. Prevalence and characteristics of hereditary non-polyposis colorectal cancer (HNPCC) syndrome in immigrant Asian colorectal cancer patients. BMC cancer. 2017 Dec 13:17(1):843. doi: 10.1186/s12885-017-3799-y. Epub 2017 Dec 13 [PubMed PMID: 29237405]
Kanth P, Grimmett J, Champine M, Burt R, Samadder NJ. Hereditary Colorectal Polyposis and Cancer Syndromes: A Primer on Diagnosis and Management. The American journal of gastroenterology. 2017 Oct:112(10):1509-1525. doi: 10.1038/ajg.2017.212. Epub 2017 Aug 8 [PubMed PMID: 28786406]
Porkka N, Lahtinen L, Ahtiainen M, Böhm JP, Kuopio T, Eldfors S, Mecklin JP, Seppälä TT, Peltomäki P. Epidemiological, clinical and molecular characterization of Lynch-like syndrome: A population-based study. International journal of cancer. 2019 Jul 1:145(1):87-98. doi: 10.1002/ijc.32085. Epub 2019 Jan 7 [PubMed PMID: 30575961]
Level 2 (mid-level) evidenceSui QQ, Jiang W, Wu XD, Ling YH, Pan ZZ, Ding PR. A frameshift mutation in exon 19 of MLH1 in a Chinese Lynch syndrome family: a pedigree study. Journal of Zhejiang University. Science. B. 2019 Jan.:20(1):105-108. doi: 10.1631/jzus.B1800105. Epub [PubMed PMID: 30614234]
Tarancón-Diez M, Büttner R, Friedrichs N. Enhanced Tumoral MLH1-Expression in MLH1-/PMS2-Deficient Colon Cancer Is Indicative of Sporadic Colon Cancer and Not HNPCC. Pathology oncology research : POR. 2020 Jul:26(3):1435-1439. doi: 10.1007/s12253-018-00571-3. Epub 2019 Jan 6 [PubMed PMID: 30613919]
Schierbeck J, Vestergaard T, Bygum A. Skin Cancer Associated Genodermatoses: A Literature Review. Acta dermato-venereologica. 2019 Apr 1:99(4):360-369. doi: 10.2340/00015555-3123. Epub [PubMed PMID: 30653245]
Hu XR, Xu C, Kang Y, Wang T, Zhang Y, Yang XH. [Correlation between mismatch-repair protein expression and clinicopathologic features in 658 colorectal cancers]. Zhonghua bing li xue za zhi = Chinese journal of pathology. 2018 Nov 8:47(11):827-833. doi: 10.3760/cma.j.issn.0529-5807.2018.11.003. Epub [PubMed PMID: 30423605]
Hampel H. Population Screening for Hereditary Colorectal Cancer. Surgical oncology clinics of North America. 2018 Apr:27(2):319-325. doi: 10.1016/j.soc.2017.11.006. Epub [PubMed PMID: 29496092]
Cruz-Correa M, Pérez-Mayoral J, Dutil J, Echenique M, Mosquera R, Rivera-Román K, Umpierre S, Rodriguez-Quilichini S, Gonzalez-Pons M, Olivera MI, Pardo S, Puerto Rico Clinical Cancer Genetics Consortia. Hereditary cancer syndromes in Latino populations: genetic characterization and surveillance guidelines. Hereditary cancer in clinical practice. 2017:15():3. doi: 10.1186/s13053-017-0063-z. Epub 2017 Jan 21 [PubMed PMID: 28127413]
Karstensen JG, Burisch J, Pommergaard HC, Aalling L, Højen H, Jespersen N, Schmidt PN, Bülow S. Colorectal Cancer in Individuals With Familial Adenomatous Polyposis, Based on Analysis of the Danish Polyposis Registry. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2019 Oct:17(11):2294-2300.e1. doi: 10.1016/j.cgh.2019.02.008. Epub 2019 Feb 8 [PubMed PMID: 30743005]
Sutcliffe EG, Bartenbaker Thompson A, Stettner AR, Marshall ML, Roberts ME, Susswein LR, Wang Y, Klein RT, Hruska KS, Solomon BD. Multi-gene panel testing confirms phenotypic variability in MUTYH-Associated Polyposis. Familial cancer. 2019 Apr:18(2):203-209. doi: 10.1007/s10689-018-00116-2. Epub [PubMed PMID: 30604180]
Rosty C. The Role of the Surgical Pathologist in the Diagnosis of Gastrointestinal Polyposis Syndromes. Advances in anatomic pathology. 2018 Jan:25(1):1-13. doi: 10.1097/PAP.0000000000000173. Epub [PubMed PMID: 28901964]
Level 3 (low-level) evidenceBrosens LA, Langeveld D, van Hattem WA, Giardiello FM, Offerhaus GJ. Juvenile polyposis syndrome. World journal of gastroenterology. 2011 Nov 28:17(44):4839-44. doi: 10.3748/wjg.v17.i44.4839. Epub [PubMed PMID: 22171123]
Raab M, Sanhaji M, Matthess Y, Hörlin A, Lorenz I, Dötsch C, Habbe N, Waidmann O, Kurunci-Csacsko E, Firestein R, Becker S, Strebhardt K. PLK1 has tumor-suppressive potential in APC-truncated colon cancer cells. Nature communications. 2018 Mar 16:9(1):1106. doi: 10.1038/s41467-018-03494-4. Epub 2018 Mar 16 [PubMed PMID: 29549256]
Spoto CPE, Gullo I, Carneiro F, Montgomery EA, Brosens LAA. Hereditary gastrointestinal carcinomas and their precursors: An algorithm for genetic testing. Seminars in diagnostic pathology. 2018 May:35(3):170-183. doi: 10.1053/j.semdp.2018.01.004. Epub 2018 Jan 31 [PubMed PMID: 29397239]
Sengupta S, Bose S. Peutz-Jeghers Syndrome. The New England journal of medicine. 2019 Jan 31:380(5):472. doi: 10.1056/NEJMicm1806623. Epub [PubMed PMID: 30699321]
Eissing M, Ripken L, Schreibelt G, Westdorp H, Ligtenberg M, Netea-Maier R, Netea MG, de Vries IJM, Hoogerbrugge N. PTEN Hamartoma Tumor Syndrome and Immune Dysregulation. Translational oncology. 2019 Feb:12(2):361-367. doi: 10.1016/j.tranon.2018.11.003. Epub 2018 Nov 30 [PubMed PMID: 30504085]
Yauy K, Imbert-Bouteille M, Bubien V, Lindet-Bourgeois C, Rathat G, Perrochia H, MacGrogan G, Longy M, Bessis D, Tinat J, Baert-Desurmont S, Blanluet M, Perre PV, Baudry K, Pujol P, Corsini C. Ovarian Clear Cell Carcinoma in Cowden Syndrome. Journal of the National Comprehensive Cancer Network : JNCCN. 2019 Jan:17(1):7-11. doi: 10.6004/jnccn.2018.7065. Epub [PubMed PMID: 30659124]
Pilarski R. Cowden syndrome: a critical review of the clinical literature. Journal of genetic counseling. 2009 Feb:18(1):13-27. doi: 10.1007/s10897-008-9187-7. Epub 2008 Oct 30 [PubMed PMID: 18972196]
Garofola C, Jamal Z, Gross GP. Cowden Disease. StatPearls. 2024 Jan:(): [PubMed PMID: 30252240]
Sohrabi M, Zamani F, Ajdarkosh H, Rakhshani N, Ameli M, Mohamadnejad M, Kabir A, Hemmasi G, Khonsari M, Motamed N. Prevalence of colorectal polyps in a group of subjects at average-risk of colorectal cancer undergoing colonoscopic screening in Tehran, Iran between 2008 and 2013. Asian Pacific journal of cancer prevention : APJCP. 2014:15(22):9773-9 [PubMed PMID: 25520103]
Level 2 (mid-level) evidenceBuecher B. Colorectal adenomatous polyposis syndromes: Genetic determinism, clinical presentation and recommendations for care. Bulletin du cancer. 2016 Feb:103(2):199-209. doi: 10.1016/j.bulcan.2015.10.019. Epub 2016 Jan 19 [PubMed PMID: 26805944]
Charifa A, Jamil RT, Zhang X. Gardner Syndrome. StatPearls. 2024 Jan:(): [PubMed PMID: 29493967]
Sung H, Siegel RL, Rosenberg PS, Jemal A. Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. The Lancet. Public health. 2019 Mar:4(3):e137-e147. doi: 10.1016/S2468-2667(18)30267-6. Epub 2019 Feb 4 [PubMed PMID: 30733056]
Venugopal A, Stoffel EM. Colorectal Cancer in Young Adults. Current treatment options in gastroenterology. 2019 Mar:17(1):89-98. doi: 10.1007/s11938-019-00219-4. Epub [PubMed PMID: 30712157]
Symonds EL, Cole SR, Lau SY, Steele S, Meng R, Woodman RJ, Young GP, Cock C, Fraser R, Bampton P. The significance of the small adenoma: a longitudinal study of surveillance colonoscopy in an Australian population. European journal of gastroenterology & hepatology. 2019 May:31(5):563-569. doi: 10.1097/MEG.0000000000001358. Epub [PubMed PMID: 30672827]
Yu H, Hemminki A, Sundquist K, Hemminki K. Familial Associations of Colon and Rectal Cancers With Other Cancers. Diseases of the colon and rectum. 2019 Feb:62(2):189-195. doi: 10.1097/DCR.0000000000001262. Epub [PubMed PMID: 30640834]
Gupta R, Sinha S, Paul RN. The impact of microsatellite stability status in colorectal cancer. Current problems in cancer. 2018 Nov:42(6):548-559. doi: 10.1016/j.currproblcancer.2018.06.010. Epub 2018 Jul 18 [PubMed PMID: 30119911]
Vacante M, Borzì AM, Basile F, Biondi A. Biomarkers in colorectal cancer: Current clinical utility and future perspectives. World journal of clinical cases. 2018 Dec 6:6(15):869-881. doi: 10.12998/wjcc.v6.i15.869. Epub [PubMed PMID: 30568941]
Level 3 (low-level) evidenceBallester V, Rashtak S, Boardman L. Clinical and molecular features of young-onset colorectal cancer. World journal of gastroenterology. 2016 Feb 7:22(5):1736-44. doi: 10.3748/wjg.v22.i5.1736. Epub [PubMed PMID: 26855533]
Li H, Zhang L, Jiang Q, Shi Z, Tong H. Identification a nonsense mutation of APC gene in Chinese patients with familial adenomatous polyposis. Experimental and therapeutic medicine. 2017 Apr:13(4):1495-1499. doi: 10.3892/etm.2017.4122. Epub 2017 Feb 14 [PubMed PMID: 28413499]
De' Angelis GL, Bottarelli L, Azzoni C, De' Angelis N, Leandro G, Di Mario F, Gaiani F, Negri F. Microsatellite instability in colorectal cancer. Acta bio-medica : Atenei Parmensis. 2018 Dec 17:89(9-S):97-101. doi: 10.23750/abm.v89i9-S.7960. Epub 2018 Dec 17 [PubMed PMID: 30561401]
Møller P, Seppälä TT, Bernstein I, Holinski-Feder E, Sala P, Gareth Evans D, Lindblom A, Macrae F, Blanco I, Sijmons RH, Jeffries J, Vasen HFA, Burn J, Nakken S, Hovig E, Rødland EA, Tharmaratnam K, de Vos Tot Nederveen Cappel WH, Hill J, Wijnen JT, Jenkins MA, Green K, Lalloo F, Sunde L, Mints M, Bertario L, Pineda M, Navarro M, Morak M, Renkonen-Sinisalo L, Valentin MD, Frayling IM, Plazzer JP, Pylvanainen K, Genuardi M, Mecklin JP, Moeslein G, Sampson JR, Capella G, Mallorca Group. Cancer risk and survival in path_MMR carriers by gene and gender up to 75 years of age: a report from the Prospective Lynch Syndrome Database. Gut. 2018 Jul:67(7):1306-1316. doi: 10.1136/gutjnl-2017-314057. Epub 2017 Jul 28 [PubMed PMID: 28754778]
Abbaszadegan MR, Moghbeli M. Genetic and molecular origins of colorectal Cancer among the Iranians: an update. Diagnostic pathology. 2018 Dec 22:13(1):97. doi: 10.1186/s13000-018-0774-0. Epub 2018 Dec 22 [PubMed PMID: 30579343]
Markowitz SD, Bertagnolli MM. Molecular origins of cancer: Molecular basis of colorectal cancer. The New England journal of medicine. 2009 Dec 17:361(25):2449-60. doi: 10.1056/NEJMra0804588. Epub [PubMed PMID: 20018966]
Pellat A, Netter J, Perkins G, Cohen R, Coulet F, Parc Y, Svrcek M, Duval A, André T. [Lynch syndrome: What is new?]. Bulletin du cancer. 2019 Jul-Aug:106(7-8):647-655. doi: 10.1016/j.bulcan.2018.10.009. Epub 2018 Dec 4 [PubMed PMID: 30527816]
Adar T, Rodgers LH, Shannon KM, Yoshida M, Ma T, Mattia A, Lauwers GY, Iafrate AJ, Hartford NM, Oliva E, Chung DC. Universal screening of both endometrial and colon cancers increases the detection of Lynch syndrome. Cancer. 2018 Aug 1:124(15):3145-3153. doi: 10.1002/cncr.31534. Epub 2018 May 11 [PubMed PMID: 29750335]
Morin PJ. Colorectal cancer: the APC-lncRNA link. The Journal of clinical investigation. 2019 Feb 1:129(2):503-505. doi: 10.1172/JCI125985. Epub 2019 Jan 14 [PubMed PMID: 30640173]
Zhang J, Li Z, Huang X, Ye J. [Clinical and molecular characteristics of a child with familial adenomatous polyposis]. Zhonghua er ke za zhi = Chinese journal of pediatrics. 2016 Mar:54(3):205-8. doi: 10.3760/cma.j.issn.0578-1310.2016.03.010. Epub [PubMed PMID: 26957067]
Giang H, Nguyen VT, Nguyen SD, Nguyen HP, Vo BT, Nguyen TM, Nguyen NH, Truong KD, Do TT, Phan MD, Nguyen HN. Detection of a heterozygous germline APC mutation in a three-generation family with familial adenomatous polyposis using targeted massive parallel sequencing in Vietnam. BMC medical genetics. 2018 Oct 19:19(1):188. doi: 10.1186/s12881-018-0701-y. Epub 2018 Oct 19 [PubMed PMID: 30340471]
Sample DC, Samadder NJ, Pappas LM, Boucher KM, Samowitz WS, Berry T, Westover M, Nathan D, Kanth P, Byrne KR, Burt RW, Neklason DW. Variables affecting penetrance of gastric and duodenal phenotype in familial adenomatous polyposis patients. BMC gastroenterology. 2018 Jul 16:18(1):115. doi: 10.1186/s12876-018-0841-8. Epub 2018 Jul 16 [PubMed PMID: 30012100]
Kallenberg FGJ, Bastiaansen BAJ, Nio CY, Soeters MR, Boermeester MA, Aalfs CM, Bossuyt PMM, Dekker E. Adrenal Lesions in Patients With (Attenuated) Familial Adenomatous Polyposis and MUTYH-Associated Polyposis. Diseases of the colon and rectum. 2017 Oct:60(10):1057-1064. doi: 10.1097/DCR.0000000000000809. Epub [PubMed PMID: 28891849]
Hatfield E, Green JS, Woods MO, Warden G, Parfrey PS. Impact of colonoscopic screening in Familial Colorectal Cancer Type X. Molecular genetics & genomic medicine. 2018 Nov:6(6):1021-1030. doi: 10.1002/mgg3.478. Epub 2018 Oct 9 [PubMed PMID: 30300963]
Kroijer R, Kobaek-Larsen M, Qvist N, Knudsen T, Baatrup G. Colon capsule endoscopy for colonic surveillance. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland. 2019 May:21(5):532-537. doi: 10.1111/codi.14557. Epub 2019 Feb 5 [PubMed PMID: 30637886]
González ML, Causada-Calo N, Santino JP, Dominguez-Valentin M, Ferro FA, Sammartino I, Kalfayan PG, Verzura MA, Piñero TA, Cajal AR, Pavicic W, Vaccaro C. Universal determination of microsatellite instability using BAT26 as a single marker in an Argentine colorectal cancer cohort. Familial cancer. 2018 Jul:17(3):395-402. doi: 10.1007/s10689-017-0052-4. Epub [PubMed PMID: 29128931]
Moufid FZ, Bouguenouch L, El Bouchikhi I, Chbani L, Iraqui Houssaini M, Sekal M, Belhassan K, Bennani B, Ouldim K. The First Molecular Screening of MLH1 and MSH2 Genes in Moroccan Colorectal Cancer Patients Shows a Relatively High Mutational Prevalence. Genetic testing and molecular biomarkers. 2018 Aug:22(8):492-497. doi: 10.1089/gtmb.2018.0067. Epub 2018 Jul 25 [PubMed PMID: 30044143]
Arakawa K, Hata K, Kawai K, Tanaka T, Nishikawa T, Sasaki K, Shuno Y, Kaneko M, Hiyoshi M, Emoto S, Murono K, Nozawa H. Predictors for High Microsatellite Instability in Patients with Colorectal Cancer Fulfilling the Revised Bethesda Guidelines. Anticancer research. 2018 Aug:38(8):4871-4876. doi: 10.21873/anticanres.12800. Epub [PubMed PMID: 30061262]
Klančar G, Blatnik A, Šetrajčič Dragoš V, Vogrič V, Stegel V, Blatnik O, Drev P, Gazič B, Krajc M, Novaković S. A Novel Germline MLH1 In-Frame Deletion in a Slovenian Lynch Syndrome Family Associated with Uncommon Isolated PMS2 Loss in Tumor Tissue. Genes. 2020 Mar 18:11(3):. doi: 10.3390/genes11030325. Epub 2020 Mar 18 [PubMed PMID: 32197529]
Cox VL, Saeed Bamashmos AA, Foo WC, Gupta S, Yedururi S, Garg N, Kang HC. Lynch Syndrome: Genomics Update and Imaging Review. Radiographics : a review publication of the Radiological Society of North America, Inc. 2018 Mar-Apr:38(2):483-499. doi: 10.1148/rg.2018170075. Epub [PubMed PMID: 29528821]
Walkowska J, Kallemose T, Jönsson G, Jönsson M, Andersen O, Andersen MH, Svane IM, Langkilde A, Nilbert M, Therkildsen C. Immunoprofiles of colorectal cancer from Lynch syndrome. Oncoimmunology. 2019:8(1):e1515612. doi: 10.1080/2162402X.2018.1515612. Epub 2018 Sep 26 [PubMed PMID: 30546958]
McGee SF, AlGhareeb W, Ahmad CH, Armstrong D, Babak S, Berry S, Biagi J, Booth C, Bossé D, Champion P, Colwell B, Finn N, Goel R, Gray S, Green J, Harb M, Hyde A, Jeyakumar A, Jonker D, Kanagaratnam S, Kavan P, MacMillan A, Muinuddin A, Patil N, Porter G, Powell E, Ramjeesingh R, Raza M, Rorke S, Seal M, Servidio-Italiano F, Siddiqui J, Simms J, Smithson L, Snow S, St-Hilaire E, Stuckless T, Tate A, Tehfe M, Thirlwell M, Tsvetkova E, Valdes M, Vickers M, Virik K, Welch S, Marginean C, Asmis T. Eastern Canadian Colorectal Cancer Consensus Conference 2017. Current oncology (Toronto, Ont.). 2018 Aug:25(4):262-274. doi: 10.3747/co.25.4083. Epub 2018 Aug 14 [PubMed PMID: 30111967]
Level 3 (low-level) evidenceMocellin S, Baretta Z, Roqué I Figuls M, Solà I, Martin-Richard M, Hallum S, Bonfill Cosp X. Second-line systemic therapy for metastatic colorectal cancer. The Cochrane database of systematic reviews. 2017 Jan 27:1(1):CD006875. doi: 10.1002/14651858.CD006875.pub3. Epub 2017 Jan 27 [PubMed PMID: 28128439]
Level 1 (high-level) evidenceSnyder M, Bottiglieri S, Almhanna K. Impact of Primary Tumor Location on First-line Bevacizumab or Cetuximab in Metastatic Colorectal Cancer. Reviews on recent clinical trials. 2018:13(2):139-149. doi: 10.2174/1574887113666180328104109. Epub [PubMed PMID: 29595113]
Chen D, Li L, Zhang X, Gao G, Shen L, Hu J, Yang M, Liu B, Qian X. FOLFOX plus anti-epidermal growth factor receptor (EGFR) monoclonal antibody (mAb) is an effective first-line treatment for patients with RAS-wild left-sided metastatic colorectal cancer: A meta-analysis. Medicine. 2018 Mar:97(10):e0097. doi: 10.1097/MD.0000000000010097. Epub [PubMed PMID: 29517682]
Level 2 (mid-level) evidenceWang X, Yu Y, Meng W, Jiang D, Deng X, Wu B, Zhuang H, Wang C, Shen Y, Yang L, Zhu H, Cheng K, Zhao Y, Li Z, Qiu M, Gou H, Bi F, Xu F, Zhong R, Bai S, Wang Z, Zhou Z. Total neoadjuvant treatment (CAPOX plus radiotherapy) for patients with locally advanced rectal cancer with high risk factors: A phase 2 trial. Radiotherapy and oncology : journal of the European Society for Therapeutic Radiology and Oncology. 2018 Nov:129(2):300-305. doi: 10.1016/j.radonc.2018.08.027. Epub 2018 Oct 28 [PubMed PMID: 30381141]
Level 2 (mid-level) evidenceYu J, Li N, Tang Y, Wang X, Tang Y, Wang SL, Song YW, Liu YP, Li YX, Jin J. Outcomes after hypofractionated stereotactic radiotherapy for colorectal cancer oligometastases. Journal of surgical oncology. 2019 Mar:119(4):532-538. doi: 10.1002/jso.25361. Epub 2019 Jan 4 [PubMed PMID: 30609038]
Maeda T, Cannom RR, Beart RW Jr, Etzioni DA. Decision model of segmental compared with total abdominal colectomy for colon cancer in hereditary nonpolyposis colorectal cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2010 Mar 1:28(7):1175-80. doi: 10.1200/JCO.2009.25.9812. Epub 2010 Feb 1 [PubMed PMID: 20124166]
Sun J, Dong M, Xiao X. Efficacy, functional outcome and post-operative complications of total abdominal colectomy with ileorectal anastomosis vs. segmental colectomy in hereditary non-polyposis colorectal cancer. Experimental and therapeutic medicine. 2018 Sep:16(3):1603-1612. doi: 10.3892/etm.2018.6380. Epub 2018 Jun 29 [PubMed PMID: 30186378]
Schneider R, Schneider C, Büttner R, Reinacher-Schick A, Tannapfel A, Fürst A, Rüschoff J, Jakobeit C, Royer-Pokora B, Möslein G. [Colorectal Carcinoma with Suspected Lynch Syndrome: A Multidisciplinary Algorithm]. Zentralblatt fur Chirurgie. 2015 Dec:140(6):591-9. doi: 10.1055/s-0034-1368480. Epub 2014 Nov 5 [PubMed PMID: 25372301]
Herzig DO, Buie WD, Weiser MR, You YN, Rafferty JF, Feingold D, Steele SR. Clinical Practice Guidelines for the Surgical Treatment of Patients With Lynch Syndrome. Diseases of the colon and rectum. 2017 Feb:60(2):137-143. doi: 10.1097/DCR.0000000000000785. Epub [PubMed PMID: 28059909]
Level 1 (high-level) evidenceKalady MF, Church JM. Prophylactic colectomy: Rationale, indications, and approach. Journal of surgical oncology. 2015 Jan:111(1):112-7. doi: 10.1002/jso.23820. Epub 2014 Nov 21 [PubMed PMID: 25418116]
Yamadera M, Ueno H, Kobayashi H, Konishi T, Ishida F, Yamaguchi T, Hinoi T, Inoue Y, Kanemitsu Y, Tomita N, Ishida H, Sugihara K. Current status of prophylactic surgical treatment for familial adenomatous polyposis in Japan. Surgery today. 2017 Jun:47(6):690-696. doi: 10.1007/s00595-016-1431-4. Epub 2016 Oct 21 [PubMed PMID: 27770209]
Kennelly RP, Gryfe R, Winter DC. Familial colorectal cancer: Patient assessment, surveillance and surgical management. European journal of surgical oncology : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2017 Feb:43(2):294-302. doi: 10.1016/j.ejso.2016.07.008. Epub 2016 Jul 27 [PubMed PMID: 27546013]
Goral D, Highland J, Lovell MA, Chan KH. Head and neck presentation of Gardner Syndrome: A pediatric case series. International journal of pediatric otorhinolaryngology. 2018 Jul:110():31-33. doi: 10.1016/j.ijporl.2018.04.018. Epub 2018 Apr 25 [PubMed PMID: 29859582]
Level 2 (mid-level) evidenceGay JT, Troxell T, Gross GP. Muir-Torre Syndrome. StatPearls. 2024 Jan:(): [PubMed PMID: 30020643]
Velter C, Caussade P, Fricker JP, Cribier B. [Muir-Torre syndrome and Turcot syndrome]. Annales de dermatologie et de venereologie. 2017 Aug-Sep:144(8-9):525-529. doi: 10.1016/j.annder.2017.01.017. Epub 2017 Feb 27 [PubMed PMID: 28256262]
Khattab A, Monga DK. Turcot Syndrome. StatPearls. 2024 Jan:(): [PubMed PMID: 30521203]
Adam MP, Feldman J, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A, Larsen Haidle J, MacFarland SP, Howe JR. Juvenile Polyposis Syndrome. GeneReviews(®). 1993:(): [PubMed PMID: 20301642]
Gonzalez RS, Adsay V, Graham RP, Shroff SG, Feely MM, Drage MG, Lewin DN, Swanson EA, Yantiss RK, Bağci P, Krasinskas AM. Massive gastric juvenile-type polyposis: a clinicopathological analysis of 22 cases. Histopathology. 2017 May:70(6):918-928. doi: 10.1111/his.13149. Epub 2017 Feb 16 [PubMed PMID: 27991685]
Level 3 (low-level) evidenceAhmed A, Alsaleem B. Nonfamilial Juvenile Polyposis Syndrome with Exon 5 Novel Mutation in SMAD 4 Gene. Case reports in pediatrics. 2017:2017():5321860. doi: 10.1155/2017/5321860. Epub 2017 Mar 27 [PubMed PMID: 28428902]
Level 3 (low-level) evidenceJia Y, Fu H, Li N, Kang Q, Sheng J. [Diagnosis and treatment for 46 cases of Peutz-Jeghers syndrome]. Zhong nan da xue xue bao. Yi xue ban = Journal of Central South University. Medical sciences. 2018 Dec 28:43(12):1323-1327. doi: 10.11817/j.issn.1672-7347.2018.12.007. Epub [PubMed PMID: 30643048]
Level 3 (low-level) evidenceWu M, Krishnamurthy K. Peutz-Jeghers Syndrome. StatPearls. 2024 Jan:(): [PubMed PMID: 30570978]
Khanna K, Khanna V, Bhatnagar V. Peutz-Jeghers syndrome: need for early screening. BMJ case reports. 2018 Dec 13:11(1):. doi: 10.1136/bcr-2018-225076. Epub 2018 Dec 13 [PubMed PMID: 30567229]
Level 3 (low-level) evidenceSloot YJE, Rabold K, Netea MG, Smit JWA, Hoogerbrugge N, Netea-Maier RT. Effect of PTEN inactivating germline mutations on innate immune cell function and thyroid cancer-induced macrophages in patients with PTEN hamartoma tumor syndrome. Oncogene. 2019 May:38(19):3743-3755. doi: 10.1038/s41388-019-0685-x. Epub 2019 Jan 22 [PubMed PMID: 30670777]
Yehia L, Ngeow J, Eng C. PTEN-opathies: from biological insights to evidence-based precision medicine. The Journal of clinical investigation. 2019 Feb 1:129(2):452-464. doi: 10.1172/JCI121277. Epub 2019 Jan 7 [PubMed PMID: 30614812]
Harada A, Umeno J, Esaki M. Gastrointestinal: Multiple venous malformations and polyps of the small intestine in Cowden syndrome. Journal of gastroenterology and hepatology. 2018 Nov:33(11):1819. doi: 10.1111/jgh.14304. Epub 2018 Jun 27 [PubMed PMID: 29952025]
Won HS, Chang ED, Na SJ, Whang IY, Lee DS, You SH, Kim YS, Kim JS. PTEN Mutation Identified in Patient Diagnosed with Simultaneous Multiple Cancers. Cancer research and treatment. 2019 Jan:51(1):402-407. doi: 10.4143/crt.2017.579. Epub 2018 Feb 27 [PubMed PMID: 29510612]
Pal R, Bhattacharjee R, Bhansali A. Protean manifestations of Proteus syndrome. Postgraduate medical journal. 2018 Jul:94(1113):416. doi: 10.1136/postgradmedj-2018-135731. Epub 2018 Apr 6 [PubMed PMID: 29626058]
Caux F, Plauchu H, Chibon F, Faivre L, Fain O, Vabres P, Bonnet F, Selma ZB, Laroche L, Gérard M, Longy M. Segmental overgrowth, lipomatosis, arteriovenous malformation and epidermal nevus (SOLAMEN) syndrome is related to mosaic PTEN nullizygosity. European journal of human genetics : EJHG. 2007 Jul:15(7):767-73 [PubMed PMID: 17392703]
Level 3 (low-level) evidenceTian X, Wang Q, Cai W. A Novel Mutation in MYH Gene Associated with Aggressive Colorectal Cancer in a Child: A Case Report and Review of Literature. OncoTargets and therapy. 2020:13():8557-8565. doi: 10.2147/OTT.S259587. Epub 2020 Aug 25 [PubMed PMID: 32904697]
Level 3 (low-level) evidenceLee SY, Kim DW, Kang SI, Ihn MH, Oh HK, Kang SB, Kim CH, Kim HR, Kim YJ, Ju JK. Impact of Family History on Prognosis of Patients with Sporadic Colorectal Cancer. Annals of surgical oncology. 2019 Apr:26(4):1118-1126. doi: 10.1245/s10434-019-07179-0. Epub 2019 Jan 25 [PubMed PMID: 30684157]
Thong MSY, Koch-Gallenkamp L, Jansen L, Bertram H, Eberle A, Holleczek B, Waldeyer-Sauerland M, Waldmann A, Zeissig SR, Brenner H, Arndt V. Age-specific health-related quality of life in long-term and very long-term colorectal cancer survivors versus population controls - a population-based study(). Acta oncologica (Stockholm, Sweden). 2019 May:58(5):801-810. doi: 10.1080/0284186X.2018.1557340. Epub 2019 Feb 8 [PubMed PMID: 30736716]
Level 2 (mid-level) evidenceVanaclocha-Espi M, Ibáñez J, Molina-Barceló A, Valverde-Roig MJ, Pérez E, Nolasco A, de la Vega M, de la Lastra-Bosch ID, Oceja ME, Espinàs JA, Font R, Pérez-Riquelme F, Arana-Arri E, Portillo I, Salas D, CRIBEA Group. Risk factors for severe complications of colonoscopy in screening programs. Preventive medicine. 2019 Jan:118():304-308. doi: 10.1016/j.ypmed.2018.11.010. Epub 2018 Nov 8 [PubMed PMID: 30414944]
Carlomagno N, Santangelo ML, Amato B, Calogero A, Saracco M, Cremone C, Miranda A, Dodaro C, Renda A. Total colectomy for cancer: analysis of factors linked to patients' age. International journal of surgery (London, England). 2014:12 Suppl 2():S135-S139. doi: 10.1016/j.ijsu.2014.08.363. Epub 2014 Aug 30 [PubMed PMID: 25181631]
Level 2 (mid-level) evidencePatel SG, Ahnen DJ. Colorectal Cancer in the Young. Current gastroenterology reports. 2018 Mar 28:20(4):15. doi: 10.1007/s11894-018-0618-9. Epub 2018 Mar 28 [PubMed PMID: 29616330]
Nimptsch K, Wu K. Is Timing Important? The Role of Diet and Lifestyle during Early Life on Colorectal Neoplasia. Current colorectal cancer reports. 2018 Feb:14(1):1-11. doi: 10.1007/s11888-018-0396-7. Epub 2018 Jan 18 [PubMed PMID: 30140177]
LaDuca H, McFarland R, Gutierrez S, Yussuf A, Ho N, Pepper J, Reineke P, Cain T, Blanco K, Horton C, Dolinsky JS. Quality of Clinician-Reported Cancer History When Ordering Genetic Testing. JCO clinical cancer informatics. 2018 Dec:2():1-11. doi: 10.1200/CCI.18.00014. Epub [PubMed PMID: 30652589]
Level 2 (mid-level) evidenceMauri G, Sartore-Bianchi A, Russo AG, Marsoni S, Bardelli A, Siena S. Early-onset colorectal cancer in young individuals. Molecular oncology. 2019 Feb:13(2):109-131. doi: 10.1002/1878-0261.12417. Epub 2018 Dec 22 [PubMed PMID: 30520562]
Weinberg BA, Marshall JL. Colon Cancer in Young Adults: Trends and Their Implications. Current oncology reports. 2019 Jan 18:21(1):3. doi: 10.1007/s11912-019-0756-8. Epub 2019 Jan 18 [PubMed PMID: 30659375]
Yurgelun MB, Hampel H. Recent Advances in Lynch Syndrome: Diagnosis, Treatment, and Cancer Prevention. American Society of Clinical Oncology educational book. American Society of Clinical Oncology. Annual Meeting. 2018 May 23:38():101-109. doi: 10.1200/EDBK_208341. Epub [PubMed PMID: 30231390]
Level 3 (low-level) evidenceBiller LH, Syngal S, Yurgelun MB. Recent advances in Lynch syndrome. Familial cancer. 2019 Apr:18(2):211-219. doi: 10.1007/s10689-018-00117-1. Epub [PubMed PMID: 30627969]
Level 3 (low-level) evidenceBarrow P, Khan M, Lalloo F, Evans DG, Hill J. Systematic review of the impact of registration and screening on colorectal cancer incidence and mortality in familial adenomatous polyposis and Lynch syndrome. The British journal of surgery. 2013 Dec:100(13):1719-31. doi: 10.1002/bjs.9316. Epub [PubMed PMID: 24227356]
Level 1 (high-level) evidenceCoelho H, Jones-Hughes T, Snowsill T, Briscoe S, Huxley N, Frayling IM, Hyde C. A systematic review of test accuracy studies evaluating molecular micro-satellite instability testing for the detection of individuals with lynch syndrome. BMC cancer. 2017 Dec 8:17(1):836. doi: 10.1186/s12885-017-3820-5. Epub 2017 Dec 8 [PubMed PMID: 29221446]
Level 1 (high-level) evidenceLiang J, Lin C, Hu F, Wang F, Zhu L, Yao X, Wang Y, Zhao Y. APC polymorphisms and the risk of colorectal neoplasia: a HuGE review and meta-analysis. American journal of epidemiology. 2013 Jun 1:177(11):1169-79. doi: 10.1093/aje/kws382. Epub 2013 Apr 10 [PubMed PMID: 23576677]
Level 1 (high-level) evidenceLiang TJ, Wang HX, Zheng YY, Cao YQ, Wu X, Zhou X, Dong SX. APC hypermethylation for early diagnosis of colorectal cancer: a meta-analysis and literature review. Oncotarget. 2017 Jul 11:8(28):46468-46479. doi: 10.18632/oncotarget.17576. Epub [PubMed PMID: 28515349]
Level 1 (high-level) evidenceWakeman C, Keenan J, Eteuati J, Hollington P, Eglinton T, Frizelle F. Chemoprevention of colorectal neoplasia. ANZ journal of surgery. 2017 Dec:87(12):E228-E232. doi: 10.1111/ans.13392. Epub 2015 Dec 21 [PubMed PMID: 26686322]
Dicks E, Pullman D, Kao K, MacMillan A, Simmonds C, Etchegary H. Universal tumor screening for Lynch syndrome: perspectives of Canadian pathologists and genetic counselors. Journal of community genetics. 2019 Jul:10(3):335-344. doi: 10.1007/s12687-018-0398-9. Epub 2018 Nov 21 [PubMed PMID: 30465127]
Level 3 (low-level) evidenceGaitanidis A, Spathakis M, Tsalikidis C, Alevizakos M, Tsaroucha A, Pitiakoudis M. Risk factors for cardiovascular mortality in patients with colorectal cancer: a population-based study. International journal of clinical oncology. 2019 May:24(5):501-507. doi: 10.1007/s10147-018-01382-x. Epub 2019 Jan 2 [PubMed PMID: 30604158]
Wang J, Luo L, Wang D, Guo B, Li J, Yang Z, Tang D. Combination adjuvant chemotherapy with targeted drugs for treatment of colorectal cancer: A network meta-analysis. Journal of cellular biochemistry. 2018 Feb:119(2):1521-1537. doi: 10.1002/jcb.26312. Epub 2017 Nov 24 [PubMed PMID: 28771807]
Level 1 (high-level) evidenceda Silva WC, de Araujo VE, Lima EMEA, Dos Santos JBR, Silva MRRD, Almeida PHRF, de Assis Acurcio F, Godman B, Kurdi A, Cherchiglia ML, Andrade EIG. Comparative Effectiveness and Safety of Monoclonal Antibodies (Bevacizumab, Cetuximab, and Panitumumab) in Combination with Chemotherapy for Metastatic Colorectal Cancer: A Systematic Review and Meta-Analysis. BioDrugs : clinical immunotherapeutics, biopharmaceuticals and gene therapy. 2018 Dec:32(6):585-606. doi: 10.1007/s40259-018-0322-1. Epub [PubMed PMID: 30499082]
Level 2 (mid-level) evidenceJayedi A, Emadi A, Shab-Bidar S. Dietary Inflammatory Index and Site-Specific Cancer Risk: A Systematic Review and Dose-Response Meta-Analysis. Advances in nutrition (Bethesda, Md.). 2018 Jul 1:9(4):388-403. doi: 10.1093/advances/nmy015. Epub [PubMed PMID: 30032224]
Level 3 (low-level) evidenceMa Y, Hu M, Zhou L, Ling S, Li Y, Kong B, Huang P. Dietary fiber intake and risks of proximal and distal colon cancers: A meta-analysis. Medicine. 2018 Sep:97(36):e11678. doi: 10.1097/MD.0000000000011678. Epub [PubMed PMID: 30200062]
Level 1 (high-level) evidenceGianfredi V, Salvatori T, Villarini M, Moretti M, Nucci D, Realdon S. Is dietary fibre truly protective against colon cancer? A systematic review and meta-analysis. International journal of food sciences and nutrition. 2018 Dec:69(8):904-915. doi: 10.1080/09637486.2018.1446917. Epub 2018 Mar 8 [PubMed PMID: 29516760]
Level 1 (high-level) evidenceLee CHA, Kong JC, Ismail H, Riedel B, Heriot A. Systematic Review and Meta-analysis of Objective Assessment of Physical Fitness in Patients Undergoing Colorectal Cancer Surgery. Diseases of the colon and rectum. 2018 Mar:61(3):400-409. doi: 10.1097/DCR.0000000000001017. Epub [PubMed PMID: 29377872]
Level 1 (high-level) evidencePiraux E, Caty G, Reychler G. Effects of preoperative combined aerobic and resistance exercise training in cancer patients undergoing tumour resection surgery: A systematic review of randomised trials. Surgical oncology. 2018 Sep:27(3):584-594. doi: 10.1016/j.suronc.2018.07.007. Epub 2018 Jul 17 [PubMed PMID: 30217322]
Level 1 (high-level) evidence