Introduction
Giant cell tumor (GCT) is one of the most common benign bone tumors, predominantly occurring in young adults aged 20 to 40 with a high recurrence rate and the potential for aggressive behavior.[1] Typically found at the metaphyseal or epiphyseal regions of the tibia or femur, GCT, despite its predominantly benign nature, exhibits a highly unpredictable spectrum of disease behavior. Local aggressiveness varies from focal symptoms arising from bony or cortical destruction and surrounding soft tissue expansion to the rare occurrence of metastasis. Instances of GCT within the axial skeleton pose a heightened risk of severe local complications and are often deemed unresectable.[2]
Under the microscope, the biopsied tissue reveals multinucleated giant cells comprising 3 distinct cell types:
- Giant cell tumor stromal cells originating from osteoblasts
- Mononuclear histiocytic cells
- Multinucleated giant cells belonging to an osteoclast-monocyte lineage [3]
The giant cells carry out the primary task of tumor bone resorption within the tumor. The spindle-like stromal cells are pivotal in recruiting monocytes and facilitating their fusion into giant cells. The stromal cells also improve the resorptive capabilities of the giant cells, contributing to the overall bone resorption mechanism.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The precise etiology of GCT is not fully understood, and there is ongoing debate about whether it represents a true neoplasm or a reactive condition. Notably, a 20q11 amplification is seen in 54% of GCTs, and 20% of cases exhibit over-expression of p53. Centrosome amplification and boosted telomerase activity, coupled with the prevention of telomere shortening, provide evidence supporting a neoplastic origin.[4][5][6]
Epidemiology
GCTs represent 4% to 10% of all primary bone tumors and 15% to 20% of benign bone tumors [7], with a preference for affecting young adults. Approximately half of these tumors occur in individuals during their third and fourth decades of life, with rarity observed in those older than 50. There is a female-to-male ratio between 1.3 and 1.5 to 1, and the incidence is higher among Asian populations than in Western populations. Among the reported cases, 44% are situated around the knee joint, 10% in the distal radius, 6% in the proximal humerus, and 13% in the hands and feet.[7] The spine and skull are rarely affected. In the axial skeleton, the ala of the sacrum is the most common location, and when the spine is involved, the vertebral body is the most commonly affected. The mandible and maxilla are preferred in the head, while in the hand, GCTs frequently occur in the phalanges.
Although benign, GCTs exhibit locally aggressive behavior and have the potential to metastasize. Around 1% to 5% of cases show metastasis, with a notable positive correlation between the occurrence of metastases and local aggressiveness and recurrence.[8] The lungs are the most common site for metastases.[9] Varying degrees of local aggressiveness, ranging from simple cortical breakthrough to extension into surrounding soft tissues and articular structures, can cause severe and debilitating local complications. The risk of recurrence is approximately 35%.[10]
The tumor typically occurs sporadically before the age of 20, with less than 5% of cases presenting in skeletally immature patients.[11] A higher incidence of vertebral GCT and multicentricity is noted in patients with skeletal immaturity. Although less common, multifocal lesions exhibit more aggressiveness than solitary lesions.[12] In individuals with Paget disease, there is an elevated occurrence of GCT, with a preference for flat bones like the skull and pelvis.[13]
Pathophysiology
The pathogenesis of GCT appears to be significantly influenced by the receptor activator of the nuclear factor kappa B [NF-kB] ligand (RANKL). Under normal physiologic conditions, osteoclast formation requires interaction with cells of the osteoblastic lineage, which may depend upon cell-cell contact and the interaction of RANKL with its receptor RANK.[14] Monocytes express high levels of this receptor, while various cell types, including stromal cells and lymphocytes, express RANKL. Different coregulatory molecules also participate in osteoclast formation, including monocyte-colony-stimulating factor, vitamin D, parathyroid and parathyroid hormone-related protein, and prostaglandins.[15]
Several studies identified a high expression of RANKL by stromal cells within GCTs.[15][16] These stromal cells also secrete factors that can regulate or prevent osteoclastogenesis, including osteoprotegerin, serving as a natural negative regulator of RANKLE that obstructs osteoclast and osteoblast interactions and functions as a natural negative regulator of RANKL.[17] The expression of RANKL by the osteoblast-like mononuclear stromal cells stimulates the recruitment of the osteoclastic cells from a normal monocytic pre-osteoclast cell. The osteoclastic giant cells then actively absorb host bone via a cathepsin K and matrix metalloproteinase 13-mediated process, which would account for the osteolysis associated with these tumors.[18]
Mutations in the H3F3A gene, found in over 90% of GCT, are implicated in driving tumorigenesis. These mutations are restricted to the stromal cell population and are absent in osteoclasts or their precursors.[19] Neoplastic stromal cells likely possess an immature osteoblast phenotype, expressing markers such as RANKL and other indicators of the early osteoblast lineage within their transcriptional repertoire.[20] The activation of stromal cells has been hypothesized to occur not from inherent genetic changes but rather from the local release of red cells and plasma proteins into the matrix induced by hemorrhage. Maintaining the stromal cells' immature state may involve unknown reciprocal signals from giant cells. RANKL has been identified as a primary molecular target for therapeutic interventions.[14]
Furthermore, investigations into PD-L1 levels among patients with GCT have revealed higher local recurrence rates in individuals expressing PD-L1.[21] There is speculation that PD-L1 immune checkpoint inhibitors may benefit patients experiencing recurrent GCT following denosumab therapy.[22][23]
Histopathology
Upon gross inspection, these lesions exhibit characteristic features such as chocolate brown, soft and spongy texture, and fragility.[24] Yellow-to-orange discoloration from the hemosiderin can also be present. Commonly, cystic blood-filled cavities within the tumor may be observed.[1] Examination typically reveals a variable degree of cortical expansion and disruption while the periosteum remains intact.[25]
Histologically, these lesions appear cellular, featuring a distinctive composition of multinucleated giant cells and a background network of mononuclear stromal cells.[20] The mononuclear cells can exhibit a variety of shapes, including plump, oval, or spindle-shaped, and may display prominent mitotic activity, although cellular atypia is uncommon. The multinucleate giant cells have numerous centrally located nuclei, unlike the peripherally located nuclei of Langerhans-type giant cells observed in atypical infections. The nuclei of these giant cells are compact and oval, containing prominent nucleoli. Giant cells are distributed throughout the lesion, and the concentration of multinucleated giant cells can vary from tumor to tumor. While some tumors feature numerous multinucleated giant cells, others have limited giant cells settled in whirls of spindle-shaped stromal cells. In approximately 5% of cases, giant cells invade small perforating vessels.
In benign bone GCTs, 3 distinct cell types are identified:[26]
- Type I cells: Resembling interstitial fibroblasts; these cells produce collagen and exhibit proliferative capabilities. This cell likely constitutes the tumor component of GCT and shares features with mesenchymal stem cells. Their characteristics suggest a potential early differentiation into osteoblasts.[27]
- Type II cells: Also interstitial, these cells resemble the monocyte/macrophage family and could potentially be recruited from the peripheral bloodstream.[1] Type II cells serve as precursors to the multinucleated giant cells within the tumor.
- Type III cells: Represented by multinucleated giant cells, these cells share many characteristics with osteoclasts and display similar morphologies.[15] Type III cells possess enzymes for bone resorption, including tartrate-resistant acid phosphatase and type II carbonic anhydrase.[28][29]
Type II and type III cells exhibit significant activity for insulin-like growth factors 1 and 2, while this activity is notably absent in type I cells. This observation implies that insulin-like growth factors 1 and 2 play a crucial role in the development and regulation of GCTs.[1]
Genetically, 80% of individuals with GCTs of the bone exhibit the cytogenetic abnormality of telomeric associations (tas), with half of the cells in the tumor showing the tas abnormality.[30] The RANK pathway is often implicated in the pathogenesis of GCT, representing a crucial signaling pathway in bone remodeling. This pathway plays a critical role in the differentiation of precursors into multinucleated osteoclasts and the activation of osteoclasts, leading to bone resorption.[31] H3F3A gene mutations are reported in around 69% to 100% of GCTs. Recently, a case of GCT of the bone was found to have an H3F3B gene mutation.[32] Yakoub et al reported 2 cases of giant cell-poor GCT of the bone, diagnosed by the presence of H3.3 G34W monoclonal antibody in the mononuclear cells through immunohistochemistry.[33]
History and Physical
The presentation of GCTs can vary, and common findings include the following:
- Pain: The most prevalent symptom, often due to mechanical insufficiency resulting from bone destruction.
- Swelling and deformity: Associated with more extensive lesions.
- A soft tissue mass or bump: Occasional and results from cortical destruction and tumor progression outside the bone, typically found close to the joint. A limited range of motion at the joint area is expected.
- Joint effusion and synovitis: Possible manifestations
- Pathological fractures: Approximately 12% of patients present with fractures at diagnosis.[34][35] The pathologic fracture incidence at presentation is 11% to 37%, indicating a potentially more aggressive disease with a higher risk of local recurrence and metastatic spread.[29][36]
- Epiphyseal location: Found in 90% of tumors, often extending to the articular subchondral bone or abutting the cartilage. It rarely invades the joint or its capsule. In skeletally immature patients, lesions are likely found in the metaphysis.[37][38] Only 1.2% of GCT involved metaphysis or diaphysis without epiphyseal involvement.
- Common locations: Descending order of occurrence includes the distal femur, proximal tibia, distal radius, and sacrum.[39] Half of all GCTs arise around the knee region. Other sites include the proximal femur, fibular head, and proximal humerus. Pelvic bone involvement is relatively rare.[40]
- Multicentricity: The simultaneous occurrence of GCT in different sites occurs but is exceedingly rare.[41][42] Most commonly, GCT is a solitary lesion. Multicentric involvement (<1%) is clinically aggressive and tends to affect the small bones of the hands and feet, showing differences from solitary lesions. Patients with multicentric lesions are generally younger than those with lesions elsewhere.
Evaluation
The evaluation for GCT involves a combination of laboratory and imaging studies, followed by a biopsy for a definitive diagnosis. Below is a detailed discussion.
Blood Investigations
Routine blood investigations are conducted as part of the preoperative workup. Specifically, serum acid phosphatase should be assessed, as it is known to be increased in patients with GCT and can correlate with treatment response. This is especially useful in cases of local recurrence. In a retrospective study, Hayashida et al reported that tartrate-resistant acid phosphatase 5b levels were found to be raised in younger patients and those with fewer pathological secondary changes. Interestingly, these levels do not necessarily correlate with tumor volume.[43]
Imaging Modalities
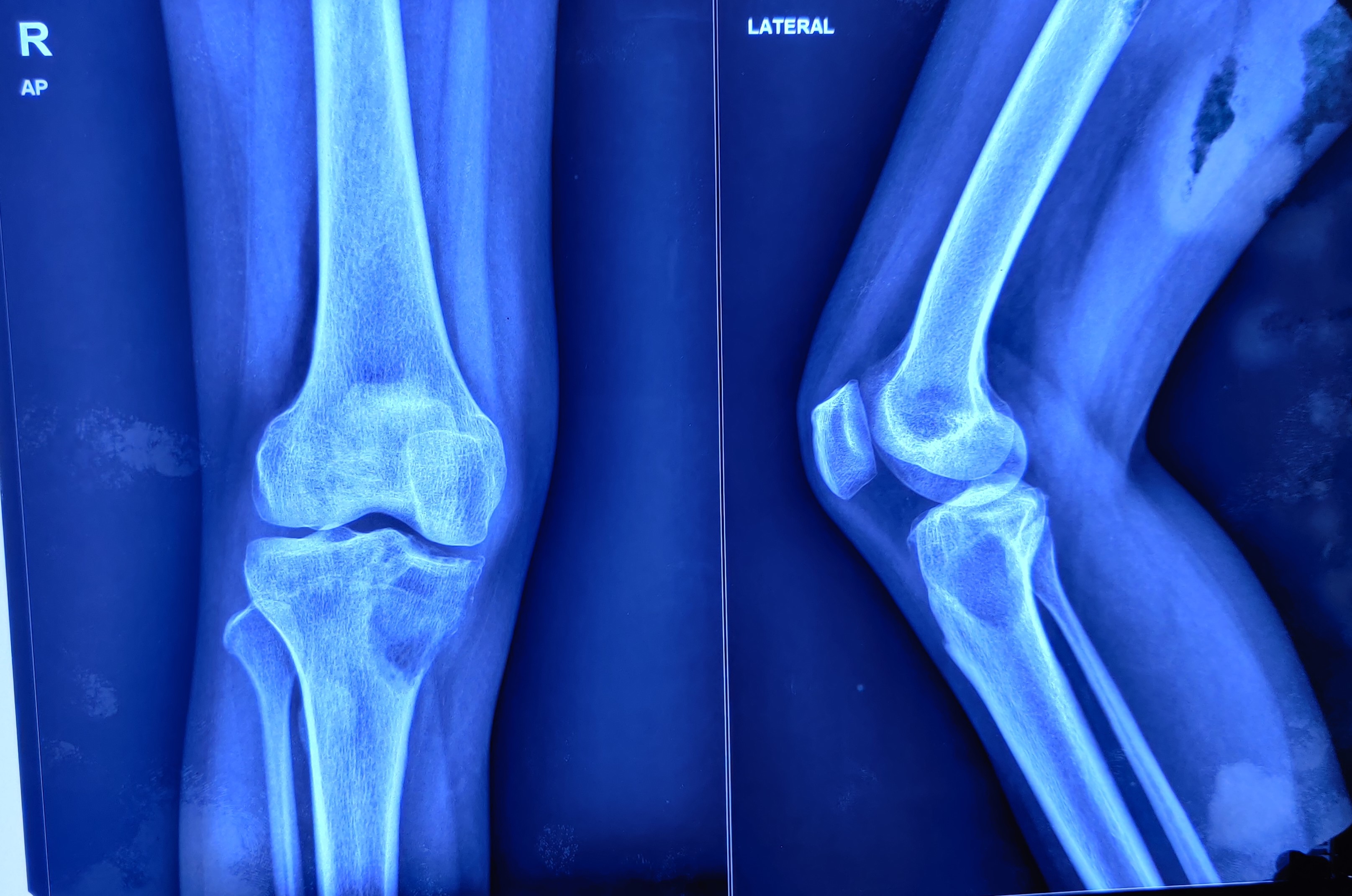
Radiograph examination typically reveals a characteristic radiolucent geographic appearance with a narrow transition zone at the lesion margin (see Image. Lytic Lesion). Unlike many benign lesions, GCT lacks a prominent sclerotic rim at the lesion margin. Calcification of the matrix, periosteal reaction, and new bone formation are typically absent.[20] The lesion is eccentrically located in the epiphyseal portion and tends to extend up to a centimeter into the subchondral bone.
Imaging modalities such as computed tomography (CT) scan and magnetic resonance imaging (MRI) can confirm the typical subchondral location of GCTs within the bone and assess the extent of a soft tissue mass, either beyond the bone cortex or through the adjacent joint.[44][45] Functional positron emission tomography (PET) and bone scans are other modern imaging modalities that can determine the extent of disease involvement.
CT scans provide a more accurate assessment of cortical thinning, penetration, and bone mineralization than plain radiographs. The neocortex formation and tumor density can be visualized, helping distinguish primary osteosarcoma. A chest CT scan is recommended in patients with locally recurrent disease to assess for metastatic spread.
MRI is a crucial tool for assessing the integrity of the surrounding soft tissues, neurovascular structures, and the extent of subchondral extension into adjacent joints. GCT lesions typically present with homogeneous signal intensity, appearing as well-circumscribed lesions on MRI. On T1-weighted images, these lesions exhibit low signal intensity, while on T2-weighted images, intermediate signal intensity is observed. The typical features include an expansile hypervascular mass with cystic changes, displaying heterogeneous low to intermediate signal intensity on T1-weighted images and intermediate to high intensity on T2-weighted images.[24][25] Notably, areas of low signal intensity on both T1 and T2-weighted images are attributed to the accumulation of significant amounts of hemosiderin.[20] MRI helps assess the soft tissue mass and cystic components within the tumor. For the evaluation of residual or recurrent GCT, fat-suppression fluid-sensitive sequences in MRI are useful.[23]
Bone scans aid in staging multicentric disease, although findings, typically revealing a decrease in the radiotracer uptake in the tumor's center, lack specificity for GCTs. Aneurysmal bone cysts exhibit a similar appearance. Limited data exist regarding fluorine-18 fluorodeoxyglucose (FDG)-PET for newly diagnosed GCT. GCT shows the accumulation of the FDG tracer, distinguishing it from many benign bone tumors, presumably due to the active metabolism of osteoclast-like giant cells.[26][27] However, the advantages of FDG PET evaluation compared to conventional imaging with CT, MRI, or a bone scan remain unclear. Changes in FDG uptake over time correlate with the tumor's metabolism and angiogenic activity.[28] Additionally, the response to denosumab therapy can be assessed using 18F-fluorodeoxyglucose-positron avidity.[23]
Biopsy and Immunohistochemistry
Biopsy samples undergo immunohistochemistry, and identifying the H3.3-G34W mutation is sensitive and specific for diagnosing GCT, helping differentiate it from other giant cell-rich tumors.[46][47] Furthermore, detecting this mutation provides valuable insights into the molecular characteristics of GCT, informing potential therapeutic approaches and prognostic considerations for patients.
Treatment / Management
The management of GCT involves a multidisciplinary approach, combining surgical, medical, and sometimes radiation therapies. The specific approach depends on factors such as the tumor's location, size, aggressiveness, and whether it is primary or recurrent.
Surgical Resection
The standard care for treating GCT often involves a tailored approach considering the benign nature of most GCTs, their proximity to joints in young adults, and the goal of preserving bone anatomy. Many authors advocate for an intralesional approach rather than resection to maintain bone integrity.[48][49][50](B3)
While wide resection has been associated with a decreased risk of local recurrence, potentially raising the recurrence-free survival rate from 84% to 100%,[29][51][52] this approach comes with higher rates of surgical complications. It may lead to functional impairment, necessitating reconstruction.[53][54][55] The decision between intralesional curettage and wide resection is often made based on the tumor's location, size, aggressiveness, and the patient's overall health and preferences.(B2)
Resection may be the preferred option in benign tumors, particularly when bone salvageability through intralesional methods would cause a severe compromise in mechanical characteristics. This applies particularly to the "expendable bones," such as the lower ulnar and upper fibular end, where excision may be the treatment of choice.
In primary and recurrent cases, especially when the tumor involves the end of a long bone and causes significant dysfunction of the joint surface, reconstruction becomes necessary. Several options are available for these cases, including mega prosthetic joint replacement, biologic reconstruction with an autograft, arthrodesis with internal/external fixation, microvascular fibula reconstruction, Ilizarov method of bone regeneration, and osteoarticular allograft.[1][56](B3)
In the past, GCTs were often treated with amputations, wide resections, or reconstructions. However, considering that GCTs are benign yet locally aggressive tumors, a local intralesional surgical approach is deemed appropriate in most cases. Treatment options include curettage, curettage and bone grafting, curettage with polymethylmethacrylate (PMMA) insertion, and primary resection. Radiation therapy and embolization of the feeding vessels are used for pelvic and sacral tumors that are not amenable to surgery.[57]
Radiotherapy is recommended for spinal, sacral, or aggressive tumors when complete excision or curettage is impractical for any functional or medical reasons. Intralesional curettage and bone grafting are considered the limb-sparing treatment of choice, associated with acceptable functional and oncologic outcomes. However, a simple curettage with or without a bone graft presents a 27% and 55% recurrence rate. Many surgeons replace bone graft packing with PMMA packing due to its high recurrence rate.
Wide en-bloc resection is another option that offers the lowest recurrence rate and can be used in expendable bones. For instance, wide resection without reconstruction is often performed in the proximal fibula. In cases of GCT in the distal radius, resection and reconstruction with an allograft or an autograft are commonly undertaken.
Adjuvant Treatments
Adjuvant treatments, such as liquid nitrogen, phenol, or HO with argon beam coagulation, demonstrate excellent recurrence-free survival, especially when paired with intralesional curettage. The effectiveness of treating GCTs hinges more on the aggressiveness of the intralesional curettage than on the specific adjuvant used. The tumor location, associated fractures, extensions to the soft tissue, and an understanding of the resection's functional consequences influence tumor removal's adequacy.
Novel adjuvant therapies for GCTs include topical or systemic bisphosphonates like zoledronate or pamidronate. Bisphosphonates induce apoptosis and limit the tumor progression by targeting the osteoclast-like giant cells.[58][59] A clinical trial comparing zoledronic acid and denosumab reported no significant difference in the clinical and radiological outcomes. However, there was a higher risk of local recurrence with denosumab, though not statistically significant.[23] Recently, bisphosphonate mixed bone cement has been reported as an adjuvant for GCT, as it directly targets neoplastic mononuclear stromal cells after curettage.[60][61](B3)
Denosumab, a monoclonal antibody, is widely used to treat unresectable GCTs of bone in adults and skeletally-matured adolescents. It acts by specifically binding to RANKL. In addition to its primary use, denosumab has been utilized preoperatively to reduce the tumor size, diminish the tumor's blood supply, and facilitate joint preservation procedures in periarticular locations. However, consensus is lacking regarding the optimal dose and duration of denosumab for adjuvant treatment or in cases of inoperable tumors. Reports suggest increased chances of local recurrence and severe complications with long-term denosumab use, as it targets multinuclear giant cells without affecting neoplastic mononuclear stromal cells.[62]
The Food and Drug Administration (FDA) has approved denosumab for use in unresectable and metastatic GCT and in cases where surgical management would harm the patient.[23] Initially, neoadjuvant denosumab use was described for 12 months. However, due to the risk of increased local recurrence attributed to denosumab's promotion of new bone formation, which limits the identification of tumor margins, a short course of neoadjuvant denosumab has been studied. Comparative analyses indicate no significant difference in clinical or radiological outcome and the histopathological response between patients receiving a short course or long-term denosumab as a neoadjuvant therapy.[63](B3)
Sunitinib, a vascular endothelial growth factor receptor β-antagonist, has recently been reported for use with denosumab. This combination therapy aims to decrease stromal cell viability. Notably, its application was associated with completely eradicating giant and stromal cells in an adolescent patient with GCT.[64]
Cyclolinopeptide, a novel molecule extracted from linseed, has emerged as a potential new drug for GCTs. This compound possesses cytoprotective and immunosuppressive properties and demonstrates inhibitory effects on RANKL-signaling and osteoclastic differentiation.[65] Exploring cyclolinopeptide introduces a promising avenue for novel therapeutic interventions in GCT, offering an alternative approach to managing the disease. While further research and clinical studies are needed to assess the safety and efficacy of these newer novel agents, no recognized effective chemotherapeutic agent is currently available to manage GCTS.
Differential Diagnosis
Based on the radiographic findings, the differential diagnoses for GCTs include:
- Lytic metastatic lesion (particularly a vascular metastasis from thyroid or renal cell carcinoma)
- Primary bone tumor
- Brown tumor of hyperparathyroidism
- Nonossifying fibroma
- Aneurysmal bone cyst
- Fibrous metaphyseal defects
- Osteoblastoma
- Chondroblastoma
- Malignant fibrous histiocytoma
- Telangiectatic osteosarcoma.[45][66]
Notably, mutations within the H3F3A gene can distinguish GCT from other entities, as they are identified in up to 96% of cases.[67][68] However, a mutation in H3F3A does not entirely exclude malignancy in other osteoclast-rich tumors, like chondroblastoma, aneurysmal bone cyst, or nonossifying fibroma.[53][55] Specifically, chondroblastomas have a high frequency of mutations in histone 3.3 genes.[69]
Staging
Various classifications of GCTs have been proposed based on histology and clinical and radiographic appearance, although their clinical utility can be limited. The Campanacci grading system, however, provides a helpful framework:
- Grade I: Intraosseous lesions with well-marginated borders and an intact cortex.
- Grade II: More extensive intraosseous lesions associated with a thin cortex without loss of cortical continuity.
- IIA: Without pathological fracture.
- IIB: With pathological fracture.
- Grade III: Extraosseous lesions that extend into soft tissue.
Prognosis
Recurrence occurring after 3 years has been considered exceptional in the literature,[51] with the local recurrence rate for GCTs ranging from 20% to 50%, averaging 33%.[41][70] Modern curettage techniques have contributed to an improvement in the GCT local control rate. Total serum acid phosphatase is suggested as a tumor marker to monitor the response to GCT treatment. While an increase in tumor grade from I to III may not necessarily reflect the biological aggressiveness of the tumor, there is an observed increase in the recurrence rate in grade III lesions. A true spontaneous transformation to malignancy has been reported in very few cases.[71]
Pulmonary metastases account for about 16% to 25% of relapsed GCT cases, although they are seen in only 1% to 6% of primary cases. Treatment for pulmonary metastases involves wide resection, often combined with interferon alfa, chemotherapy, and radiation. In cases where complete surgical excision is not possible, adjuvant treatments, like radiation or chemotherapy, are generally recommended. For unresectable metastases, a combination of chemotherapy and radiation therapy is implemented. Lung metastases can have poor outcomes.[72][73][74]
Metastases of bone GCT are relatively rare, occurring in approximately 3% of cases, but the behavior of pulmonary metastasis is unpredictable.[75][76][77] Younger patients with local recurrence, Enneking stage-III disease, or axial involvement are at an increased risk.[68] Histologically, metastatic lesions resemble primary lesions. The mean interval between the onset of the tumor and the detection of pulmonary metastasis is approximately 18 to 24 months.[68] Complete excision of the metastases has shown success with good long-term survival, although those with comorbidities may eventually succumb to the metastases.[1]
In cases where a primary bone sarcoma is suspected within prominent areas of giant cell reaction and hemorrhage in a newly discovered GCT that was initially missed, it is essential to consider the possibility of malignancy rather than assuming a malignant transformation.[78] Malignant transformations in GCT can result in osteosarcoma, malignant histiocytoma, or fibrosarcoma. The occurrence of malignant transformation may be identified several years after the initial surgery, with a range of 4 to 40 years from the initial surgery.[79]
Overall, GCTs have a favorable prognosis. Pulmonary metastases can contribute to death in 16% to 25%. When a true malignant transformation occurs within a GCT, the prognosis is comparatively worse than that for a benign GCT. Nonetheless, it tends to be somewhat better than the prognosis for other high-grade sarcomas.
Complications
Giant cell tumors of the bone can be complicated by the following:
- Tumor recurrence
- Osteoarthritis of the knee joint
- Stress fracture
- Limited movement
- Pulmonary metastasis
- Local and deep infections
- Osteomyelitis
- Joint degeneration
- Hardware failure
Deterrence and Patient Education
As the exact cause of GCTs, like most other tumors, remains unclear, preventive measures for their occurrence are unknown. However, educating patients about the potential presentations of local invasion or metastasis is crucial, enabling them to seek medical advice early in the process. Early detection often leads to better outcomes. Additionally, educating patients about surgical treatment options is of utmost importance, empowering them to make informed decisions that can significantly impact the overall outcomes. Patient awareness and involvement are vital in managing GCT and optimizing the treatment journey.
Pearls and Other Issues
A few key facts to remember about GCT include the following:
- Bone GCT is a benign but locally aggressive primary bone tumor.
- Mutation in the H3F3A gene is a specific marker for diagnosing GCT.[80]
- Local control involves tumor removal with curettage therapies chosen for acceptable long-term outcomes and functional consequences.
- Post-treatment monitoring includes serial chest and site radiographs and serial physical examinations.
- Relapses may manifest as new swelling or pain.
- Tumor recurrence can occur many years after initial involvement and treatment.
- Recommended practice includes at least a 5-year close follow-up.
- Intensified surveillance, preferably with CT, is advised for pulmonary metastasis detection in patients with a local recurrence of bone GCT, particularly in the first 3 years after diagnosis.
Enhancing Healthcare Team Outcomes
Patients diagnosed with GCT benefit significantly from a collaborative and inter-professional healthcare team. In the initial stages, primary care providers or emergency physicians are often patients' first point of contact. Chiropractors may also be crucial in identifying GCT through radiographs and should promptly refer patients to the appropriate specialist. After identifying bone tumors on plain x-rays, orthopedic surgeons become pivotal in further evaluation and management. Radiologists provide interpretations of imaging studies to aid in the diagnostic process. The specialized care of orthopedic oncologists becomes essential for appropriate surgical interventions. Nursing professionals are integral throughout the care continuum, assisting in preoperative, surgical, and postoperative care. Additionally, rehabilitation specialists, such as occupational or physical therapists, contribute significantly to the patient's recovery, facilitating a prompt return to their daily activities. This collaborative approach ensures optimal care and aims to achieve the best possible outcomes for patients dealing with GCT.
Media
(Click Image to Enlarge)
References
Sobti A, Agrawal P, Agarwala S, Agarwal M. Giant Cell Tumor of Bone - An Overview. The archives of bone and joint surgery. 2016 Jan:4(1):2-9 [PubMed PMID: 26894211]
Level 3 (low-level) evidenceGhostine B, Sebaaly A, Ghanem I. Multifocal metachronous giant cell tumor: case report and review of the literature. Case reports in medicine. 2014:2014():678035. doi: 10.1155/2014/678035. Epub 2014 Jan 5 [PubMed PMID: 24511316]
Level 3 (low-level) evidenceWerner M. Giant cell tumour of bone: morphological, biological and histogenetical aspects. International orthopaedics. 2006 Dec:30(6):484-9 [PubMed PMID: 17013643]
McCarthy BJ, Shibui S, Kayama T, Miyaoka E, Narita Y, Murakami M, Matsuda A, Matsuda T, Sobue T, Palis BE, Dolecek TA, Kruchko C, Engelhard HH, Villano JL. Primary CNS germ cell tumors in Japan and the United States: an analysis of 4 tumor registries. Neuro-oncology. 2012 Sep:14(9):1194-200. doi: 10.1093/neuonc/nos155. Epub 2012 Aug 6 [PubMed PMID: 22869621]
Chan JY. A clinical overview of centrosome amplification in human cancers. International journal of biological sciences. 2011:7(8):1122-44 [PubMed PMID: 22043171]
Level 3 (low-level) evidenceSchwartz HS, Juliao SF, Sciadini MF, Miller LK, Butler MG. Telomerase activity and oncogenesis in giant cell tumor of bone. Cancer. 1995 Mar 1:75(5):1094-9 [PubMed PMID: 7850706]
Mavrogenis AF, Igoumenou VG, Megaloikonomos PD, Panagopoulos GN, Papagelopoulos PJ, Soucacos PN. Giant cell tumor of bone revisited. SICOT-J. 2017:3():54. doi: 10.1051/sicotj/2017041. Epub 2017 Sep 14 [PubMed PMID: 28905737]
Donthineni R, Boriani L, Ofluoglu O, Bandiera S. Metastatic behaviour of giant cell tumour of the spine. International orthopaedics. 2009 Apr:33(2):497-501. doi: 10.1007/s00264-008-0560-9. Epub 2008 May 7 [PubMed PMID: 18461324]
Level 2 (mid-level) evidenceViswanathan S, Jambhekar NA. Metastatic giant cell tumor of bone: are there associated factors and best treatment modalities? Clinical orthopaedics and related research. 2010 Mar:468(3):827-33. doi: 10.1007/s11999-009-0966-8. Epub 2009 Jul 14 [PubMed PMID: 19597900]
Level 2 (mid-level) evidenceHasan O, Ali M, Mustafa M, Ali A, Umer M. Treatment and recurrence of giant cell tumors of bone - A retrospective cohort from a developing country. Annals of medicine and surgery (2012). 2019 Dec:48():29-34. doi: 10.1016/j.amsu.2019.10.010. Epub 2019 Oct 15 [PubMed PMID: 31687136]
Level 2 (mid-level) evidencePatel MT, Nayak MR. Unusual Presentation of Giant Cell Tumor in Skeletally Immature Patient in Diaphysis of Ulna. Journal of orthopaedic case reports. 2015 Apr-Jun:5(2):28-31. doi: 10.13107/jocr.2250-0685.266. Epub [PubMed PMID: 27299037]
Level 3 (low-level) evidenceShekhar A, Murgod G, Korlhalli S. Synchronous Multicentric Giant Cell Tumour (GCT)-A Rare Case Report. Journal of clinical and diagnostic research : JCDR. 2014 Feb:8(2):185-6. doi: 10.7860/JCDR/2014/8153.4055. Epub 2014 Feb 3 [PubMed PMID: 24701530]
Level 3 (low-level) evidenceVerma V, Puri A, Shah S, Rekhi B, Gulia A. Giant Cell Tumor Developing in Paget's Disease of Bone: A Case Report with Review of Literature. Journal of orthopaedic case reports. 2016 Sep-Oct:6(4):103-107. doi: 10.13107/jocr.2250-0685.594. Epub [PubMed PMID: 28164066]
Level 3 (low-level) evidenceDufresne A, Derbel O, Cassier P, Vaz G, Decouvelaere AV, Blay JY. Giant-cell tumor of bone, anti-RANKL therapy. BoneKEy reports. 2012 Sep 5:1():149. doi: 10.1038/bonekey.2012.149. Epub 2012 Sep 5 [PubMed PMID: 24363925]
Morgan T, Atkins GJ, Trivett MK, Johnson SA, Kansara M, Schlicht SL, Slavin JL, Simmons P, Dickinson I, Powell G, Choong PF, Holloway AJ, Thomas DM. Molecular profiling of giant cell tumor of bone and the osteoclastic localization of ligand for receptor activator of nuclear factor kappaB. The American journal of pathology. 2005 Jul:167(1):117-28 [PubMed PMID: 15972958]
Mukaihara K, Suehara Y, Kohsaka S, Akaike K, Tanabe Y, Kubota D, Ishii M, Fujimura T, Kazuno S, Okubo T, Takagi T, Yao T, Kaneko K, Saito T. Protein Expression Profiling of Giant Cell Tumors of Bone Treated with Denosumab. PloS one. 2016:11(2):e0148401. doi: 10.1371/journal.pone.0148401. Epub 2016 Feb 10 [PubMed PMID: 26863138]
Boyce BF, Xing L. Functions of RANKL/RANK/OPG in bone modeling and remodeling. Archives of biochemistry and biophysics. 2008 May 15:473(2):139-46. doi: 10.1016/j.abb.2008.03.018. Epub 2008 Mar 25 [PubMed PMID: 18395508]
Level 3 (low-level) evidenceLindeman JH, Hanemaaijer R, Mulder A, Dijkstra PD, Szuhai K, Bromme D, Verheijen JH, Hogendoorn PC. Cathepsin K is the principal protease in giant cell tumor of bone. The American journal of pathology. 2004 Aug:165(2):593-600 [PubMed PMID: 15277232]
Behjati S, Tarpey PS, Presneau N, Scheipl S, Pillay N, Van Loo P, Wedge DC, Cooke SL, Gundem G, Davies H, Nik-Zainal S, Martin S, McLaren S, Goodie V, Robinson B, Butler A, Teague JW, Halai D, Khatri B, Myklebost O, Baumhoer D, Jundt G, Hamoudi R, Tirabosco R, Amary MF, Futreal PA, Stratton MR, Campbell PJ, Flanagan AM. Distinct H3F3A and H3F3B driver mutations define chondroblastoma and giant cell tumor of bone. Nature genetics. 2013 Dec:45(12):1479-82. doi: 10.1038/ng.2814. Epub 2013 Oct 27 [PubMed PMID: 24162739]
Level 2 (mid-level) evidenceSteensma MR, Tyler WK, Shaber AG, Goldring SR, Ross FP, Williams BO, Healey JH, Purdue PE. Targeting the giant cell tumor stromal cell: functional characterization and a novel therapeutic strategy. PloS one. 2013:8(7):e69101. doi: 10.1371/journal.pone.0069101. Epub 2013 Jul 26 [PubMed PMID: 23922683]
Kushlinskii NE, Alferov AA, Timofeev YS, Gershtein ES, Bulycheva IV, Bondarev AV, Shchupak MY, Sokolov NY, Polikarpova SB, Efimova MM, Dzampaev AA, Sushentsov EA, Aliev MD, Musaev ER. Key Immune Checkpoint PD-1/PD-L1 Signaling Pathway Components in the Blood Serum from Patients with Bone Tumors. Bulletin of experimental biology and medicine. 2020 Nov:170(1):64-68. doi: 10.1007/s10517-020-05005-2. Epub 2020 Nov 24 [PubMed PMID: 33231796]
Metovic J, Annaratone L, Linari A, Osella-Abate S, Musuraca C, Veneziano F, Vignale C, Bertero L, Cassoni P, Ratto N, Comandone A, Grignani G, Piana R, Papotti M. Prognostic role of PD-L1 and immune-related gene expression profiles in giant cell tumors of bone. Cancer immunology, immunotherapy : CII. 2020 Sep:69(9):1905-1916. doi: 10.1007/s00262-020-02594-9. Epub 2020 May 6 [PubMed PMID: 32377818]
van der Heijden L, Lipplaa A, van Langevelde K, Bovée JVMG, van de Sande MAJ, Gelderblom H. Updated concepts in treatment of giant cell tumor of bone. Current opinion in oncology. 2022 Jul 1:34(4):371-378. doi: 10.1097/CCO.0000000000000852. Epub [PubMed PMID: 35837707]
Level 3 (low-level) evidenceKundu ZS, Sen R, Dhiman A, Sharma P, Siwach R, Rana P. Effect of Intravenous Zoledronic Acid on Histopathology and Recurrence after Extended Curettage in Giant Cell Tumors of Bone: A Comparative Prospective Study. Indian journal of orthopaedics. 2018 Jan-Feb:52(1):45-50. doi: 10.4103/ortho.IJOrtho_216_17. Epub [PubMed PMID: 29416169]
Level 2 (mid-level) evidencePurohit S, Pardiwala DN. Imaging of giant cell tumor of bone. Indian journal of orthopaedics. 2007 Apr:41(2):91-6. doi: 10.4103/0019-5413.32037. Epub [PubMed PMID: 21139758]
Zhou Z, Li Y, Wang X, Hu J, Kuang M, Wang Z, Li S, Xu W, Xiao J. ALCAM(+) stromal cells: role in giant cell tumor of bone progression. Cell death & disease. 2018 Feb 20:9(3):299. doi: 10.1038/s41419-018-0361-z. Epub 2018 Feb 20 [PubMed PMID: 29463803]
Salerno M, Avnet S, Alberghini M, Giunti A, Baldini N. Histogenetic characterization of giant cell tumor of bone. Clinical orthopaedics and related research. 2008 Sep:466(9):2081-91. doi: 10.1007/s11999-008-0327-z. Epub 2008 Jun 10 [PubMed PMID: 18543051]
Yoshida H, Akeho M, Yumoto T. Giant cell tumor bone. Enzyme histochemical, biochemical and tissue culture studies. Virchows Archiv. A, Pathological anatomy and histology. 1982:395(3):319-30 [PubMed PMID: 6287714]
Level 3 (low-level) evidenceTurcotte RE. Giant cell tumor of bone. The Orthopedic clinics of North America. 2006 Jan:37(1):35-51 [PubMed PMID: 16311110]
Schwartz HS, Dahir GA, Butler MG. Telomere reduction in giant cell tumor of bone and with aging. Cancer genetics and cytogenetics. 1993 Dec:71(2):132-8 [PubMed PMID: 8281516]
Wu PF, Tang JY, Li KH. RANK pathway in giant cell tumor of bone: pathogenesis and therapeutic aspects. Tumour biology : the journal of the International Society for Oncodevelopmental Biology and Medicine. 2015 Feb:36(2):495-501. doi: 10.1007/s13277-015-3094-y. Epub 2015 Jan 25 [PubMed PMID: 25618600]
Wu R, Wu X, Weng X, Xiu Y, Xu G, Liu X, Liu X. Giant cell tumor of bone with H3F3B mutation: A case report. Medicine. 2023 Feb 17:102(7):e32995. doi: 10.1097/MD.0000000000032995. Epub [PubMed PMID: 36800629]
Level 3 (low-level) evidenceYakoub MA, Torrence D, Hwang S, Bartelstein M, Healey JH, Hameed M. Giant-cell-poor giant cell tumor of bone: report of two cases and literature review. Skeletal radiology. 2023 Sep:52(9):1791-1798. doi: 10.1007/s00256-023-04292-w. Epub 2023 Feb 14 [PubMed PMID: 36781420]
Level 3 (low-level) evidenceLarsson SE, Lorentzon R, Boquist L. Giant-cell tumor of bone. A demographic, clinical, and histopathological study of all cases recorded in the Swedish Cancer Registry for the years 1958 through 1968. The Journal of bone and joint surgery. American volume. 1975 Mar:57(2):167-73 [PubMed PMID: 1112843]
Level 3 (low-level) evidenceJeys LM, Suneja R, Chami G, Grimer RJ, Carter SR, Tillman RM. Impending fractures in giant cell tumours of the distal femur: incidence and outcome. International orthopaedics. 2006 Apr:30(2):135-8 [PubMed PMID: 16474936]
Lewis VO, Wei A, Mendoza T, Primus F, Peabody T, Simon MA. Argon beam coagulation as an adjuvant for local control of giant cell tumor. Clinical orthopaedics and related research. 2007 Jan:454():192-7 [PubMed PMID: 16957652]
Level 2 (mid-level) evidenceHoeffel JC, Galloy MA, Grignon Y, Chastagner P, Floquet J, Mainard L, Kadiri R. Giant cell tumor of bone in children and adolescents. Revue du rhumatisme (English ed.). 1996 Oct:63(9):618-23 [PubMed PMID: 8938873]
Shih HN, Hsu RW, Sim FH. Excision curettage and allografting of giant cell tumor. World journal of surgery. 1998 May:22(5):432-7 [PubMed PMID: 9564283]
Bridge JA, Neff JR, Mouron BJ. Giant cell tumor of bone. Chromosomal analysis of 48 specimens and review of the literature. Cancer genetics and cytogenetics. 1992 Jan:58(1):2-13 [PubMed PMID: 1728946]
Osaka S, Toriyama S. Surgical treatment of giant cell tumors of the pelvis. Clinical orthopaedics and related research. 1987 Sep:(222):123-31 [PubMed PMID: 3621712]
Level 3 (low-level) evidenceEckardt JJ, Grogan TJ. Giant cell tumor of bone. Clinical orthopaedics and related research. 1986 Mar:(204):45-58 [PubMed PMID: 3514036]
Tornberg DN, Dick HM, Johnston AD. Multicentric giant-cell tumors in the long bones. A case report. The Journal of bone and joint surgery. American volume. 1975 Apr:57(3):420-2 [PubMed PMID: 1123400]
Level 3 (low-level) evidenceHayashida K, Kawabata Y, Yoshida T, Saito K, Fujita S, Choe H, Kato I, Takeyama M, Inaba Y. Characteristics of Patients with Giant Cell Tumor of Bone and High Serum Tartrate-Resistant Acid Phosphatase 5b Levels: Comparison of Tumor Volume and Clinical Factors. Journal of Nippon Medical School = Nippon Ika Daigaku zasshi. 2022:89(6):572-579. doi: 10.1272/jnms.JNMS.2022_89-611. Epub [PubMed PMID: 36725001]
Pereira HM, Marchiori E, Severo A. Magnetic resonance imaging aspects of giant-cell tumours of bone. Journal of medical imaging and radiation oncology. 2014 Dec:58(6):674-8. doi: 10.1111/1754-9485.12249. Epub 2014 Sep 25 [PubMed PMID: 25256094]
Cavanna L, Biasini C, Monfredo M, Maniscalco P, Mori M. Giant cell tumor of bone. The oncologist. 2014 Nov:19(11):1207. doi: 10.1634/theoncologist.2014-0267. Epub [PubMed PMID: 25378541]
Level 3 (low-level) evidenceCleven AH, Höcker S, Briaire-de Bruijn I, Szuhai K, Cleton-Jansen AM, Bovée JV. Mutation Analysis of H3F3A and H3F3B as a Diagnostic Tool for Giant Cell Tumor of Bone and Chondroblastoma. The American journal of surgical pathology. 2015 Nov:39(11):1576-83. doi: 10.1097/PAS.0000000000000512. Epub [PubMed PMID: 26457357]
Fellenberg J, Sähr H, Mancarella D, Plass C, Lindroth AM, Westhauser F, Lehner B, Ewerbeck V. Knock-down of oncohistone H3F3A-G34W counteracts the neoplastic phenotype of giant cell tumor of bone derived stromal cells. Cancer letters. 2019 Apr 28:448():61-69. doi: 10.1016/j.canlet.2019.02.001. Epub 2019 Feb 8 [PubMed PMID: 30742944]
Level 3 (low-level) evidenceDreinhöfer KE, Rydholm A, Bauer HC, Kreicbergs A. Giant-cell tumours with fracture at diagnosis. Curettage and acrylic cementing in ten cases. The Journal of bone and joint surgery. British volume. 1995 Mar:77(2):189-93 [PubMed PMID: 7706330]
Level 3 (low-level) evidenceRock M. Curettage of giant cell tumor of bone. Factors influencing local recurrences and metastasis. La Chirurgia degli organi di movimento. 1990:75(1 Suppl):204-5 [PubMed PMID: 2249533]
Miller G, Bettelli G, Fabbri N, Capanna R. Curettage of giant cell tumor of bone. Introduction--material and methods. La Chirurgia degli organi di movimento. 1990:75(1 Suppl):203 [PubMed PMID: 2249532]
Lausten GS, Jensen PK, Schiødt T, Lund B. Local recurrences in giant cell tumour of bone. Long-term follow up of 31 cases. International orthopaedics. 1996:20(3):172-6 [PubMed PMID: 8832321]
Level 3 (low-level) evidenceCampanacci M, Baldini N, Boriani S, Sudanese A. Giant-cell tumor of bone. The Journal of bone and joint surgery. American volume. 1987 Jan:69(1):106-14 [PubMed PMID: 3805057]
Sung HW, Kuo DP, Shu WP, Chai YB, Liu CC, Li SM. Giant-cell tumor of bone: analysis of two hundred and eight cases in Chinese patients. The Journal of bone and joint surgery. American volume. 1982 Jun:64(5):755-61 [PubMed PMID: 7045129]
Level 3 (low-level) evidenceMcDonald DJ, Sim FH, McLeod RA, Dahlin DC. Giant-cell tumor of bone. The Journal of bone and joint surgery. American volume. 1986 Feb:68(2):235-42 [PubMed PMID: 3511063]
Oda Y, Miura H, Tsuneyoshi M, Iwamoto Y. Giant cell tumor of bone: oncological and functional results of long-term follow-up. Japanese journal of clinical oncology. 1998 May:28(5):323-8 [PubMed PMID: 9703860]
Level 2 (mid-level) evidencevan der Heijden L, Dijkstra PD, van de Sande MA, Kroep JR, Nout RA, van Rijswijk CS, Bovée JV, Hogendoorn PC, Gelderblom H. The clinical approach toward giant cell tumor of bone. The oncologist. 2014 May:19(5):550-61. doi: 10.1634/theoncologist.2013-0432. Epub 2014 Apr 9 [PubMed PMID: 24718514]
Puri A, Agarwal M. Treatment of giant cell tumor of bone: Current concepts. Indian journal of orthopaedics. 2007 Apr:41(2):101-8. doi: 10.4103/0019-5413.32039. Epub [PubMed PMID: 21139760]
Fujimoto N, Nakagawa K, Seichi A, Terahara A, Tago M, Aoki Y, Hosoi Y, Ohtomo K. A new bisphosphonate treatment option for giant cell tumors. Oncology reports. 2001 May-Jun:8(3):643-7 [PubMed PMID: 11295095]
Level 3 (low-level) evidenceChang SS, Suratwala SJ, Jung KM, Doppelt JD, Zhang HZ, Blaine TA, Kim TW, Winchester RJ, Lee FY. Bisphosphonates may reduce recurrence in giant cell tumor by inducing apoptosis. Clinical orthopaedics and related research. 2004 Sep:(426):103-9 [PubMed PMID: 15346059]
Zwolak P, Manivel JC, Jasinski P, Kirstein MN, Dudek AZ, Fisher J, Cheng EY. Cytotoxic effect of zoledronic acid-loaded bone cement on giant cell tumor, multiple myeloma, and renal cell carcinoma cell lines. The Journal of bone and joint surgery. American volume. 2010 Jan:92(1):162-8. doi: 10.2106/JBJS.H.01679. Epub [PubMed PMID: 20048108]
Greenberg DD, Lee FY. Bisphosphonate-loaded Bone Cement as a Local Adjuvant Therapy for Giant Cell Tumor of Bone: A 1 to 12-Year Follow-up Study. American journal of clinical oncology. 2019 Mar:42(3):231-237. doi: 10.1097/COC.0000000000000504. Epub [PubMed PMID: 30811352]
Xiang F, Liu H, Deng J, Ma W, Chen Y. Progress on Denosumab Use in Giant Cell Tumor of Bone: Dose and Duration of Therapy. Cancers. 2022 Nov 23:14(23):. doi: 10.3390/cancers14235758. Epub 2022 Nov 23 [PubMed PMID: 36497239]
Hindiskere S, Errani C, Doddarangappa S, Ramaswamy V, Rai M, Chinder PS. Is a Short-course of Preoperative Denosumab as Effective as Prolonged Therapy for Giant Cell Tumor of Bone? Clinical orthopaedics and related research. 2020 Nov:478(11):2522-2533. doi: 10.1097/CORR.0000000000001285. Epub [PubMed PMID: 32401001]
Mahdal M, Neradil J, Mudry P, Paukovcekova S, Staniczkova Zambo I, Urban J, Macsek P, Pazourek L, Tomas T, Veselska R. New Target for Precision Medicine Treatment of Giant-Cell Tumor of Bone: Sunitinib Is Effective in the Treatment of Neoplastic Stromal Cells with Activated PDGFRβ Signaling. Cancers. 2021 Jul 15:13(14):. doi: 10.3390/cancers13143543. Epub 2021 Jul 15 [PubMed PMID: 34298757]
Taniguchi Y, Yamamoto N, Hayashi K, Takeuchi A, Miwa S, Igarashi K, Higuchi T, Abe K, Yonezawa H, Araki Y, Morinaga S, Kamei J, Nugroho AE, Kaneda T, Morita H, Tsuchiya H. Anti-tumor Effects of Cyclolinopeptide on Giant-cell Tumor of the Bone. Anticancer research. 2019 Nov:39(11):6145-6153. doi: 10.21873/anticanres.13822. Epub [PubMed PMID: 31704842]
Chakarun CJ, Forrester DM, Gottsegen CJ, Patel DB, White EA, Matcuk GR Jr. Giant cell tumor of bone: review, mimics, and new developments in treatment. Radiographics : a review publication of the Radiological Society of North America, Inc. 2013 Jan-Feb:33(1):197-211. doi: 10.1148/rg.331125089. Epub [PubMed PMID: 23322837]
Siebenrock KA, Unni KK, Rock MG. Giant-cell tumour of bone metastasising to the lungs. A long-term follow-up. The Journal of bone and joint surgery. British volume. 1998 Jan:80(1):43-7 [PubMed PMID: 9460951]
Chan CM, Adler Z, Reith JD, Gibbs CP Jr. Risk factors for pulmonary metastases from giant cell tumor of bone. The Journal of bone and joint surgery. American volume. 2015 Mar 4:97(5):420-8. doi: 10.2106/JBJS.N.00678. Epub [PubMed PMID: 25740033]
Level 2 (mid-level) evidenceDomovitov SV, Healey JH. Primary malignant giant-cell tumor of bone has high survival rate. Annals of surgical oncology. 2010 Mar:17(3):694-701. doi: 10.1245/s10434-009-0803-z. Epub 2009 Nov 10 [PubMed PMID: 19902306]
Level 2 (mid-level) evidenceGoldenberg RR, Campbell CJ, Bonfiglio M. Giant-cell tumor of bone. An analysis of two hundred and eighteen cases. The Journal of bone and joint surgery. American volume. 1970 Jun:52(4):619-64 [PubMed PMID: 5479455]
Level 3 (low-level) evidenceAoki J, Watanabe H, Shinozaki T, Takagishi K, Ishijima H, Oya N, Sato N, Inoue T, Endo K. FDG PET of primary benign and malignant bone tumors: standardized uptake value in 52 lesions. Radiology. 2001 Jun:219(3):774-7 [PubMed PMID: 11376267]
Wülling M, Engels C, Jesse N, Werner M, Delling G, Kaiser E. The nature of giant cell tumor of bone. Journal of cancer research and clinical oncology. 2001 Aug:127(8):467-74 [PubMed PMID: 11501745]
Balke M, Schremper L, Gebert C, Ahrens H, Streitbuerger A, Koehler G, Hardes J, Gosheger G. Giant cell tumor of bone: treatment and outcome of 214 cases. Journal of cancer research and clinical oncology. 2008 Sep:134(9):969-78. doi: 10.1007/s00432-008-0370-x. Epub 2008 Mar 6 [PubMed PMID: 18322700]
Level 2 (mid-level) evidenceBalke M, Ahrens H, Streitbuerger A, Koehler G, Winkelmann W, Gosheger G, Hardes J. Treatment options for recurrent giant cell tumors of bone. Journal of cancer research and clinical oncology. 2009 Jan:135(1):149-58. doi: 10.1007/s00432-008-0427-x. Epub 2008 Jun 3 [PubMed PMID: 18521629]
Level 2 (mid-level) evidenceVult von Steyern F, Bauer HC, Trovik C, Kivioja A, Bergh P, Holmberg Jörgensen P, Follerås G, Rydholm A, Scandinavian Sarcoma Group. Treatment of local recurrences of giant cell tumour in long bones after curettage and cementing. A Scandinavian Sarcoma Group study. The Journal of bone and joint surgery. British volume. 2006 Apr:88(4):531-5 [PubMed PMID: 16567792]
Level 2 (mid-level) evidenceFeigenberg SJ, Marcus RB Jr, Zlotecki RA, Scarborough MT, Enneking WF. Whole-lung radiotherapy for giant cell tumors of bone with pulmonary metastases. Clinical orthopaedics and related research. 2002 Aug:(401):202-8 [PubMed PMID: 12151897]
Level 3 (low-level) evidenceBertoni F, Present D, Enneking WF. Giant-cell tumor of bone with pulmonary metastases. The Journal of bone and joint surgery. American volume. 1985 Jul:67(6):890-900 [PubMed PMID: 4019539]
Level 3 (low-level) evidenceEnneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clinical orthopaedics and related research. 1980 Nov-Dec:(153):106-20 [PubMed PMID: 7449206]
Palmerini E, Picci P, Reichardt P, Downey G. Malignancy in Giant Cell Tumor of Bone: A Review of the Literature. Technology in cancer research & treatment. 2019 Jan 1:18():1533033819840000. doi: 10.1177/1533033819840000. Epub [PubMed PMID: 30935298]
Rekhi B, Dave V. Giant cell tumor of bone: An update, including spectrum of pathological features, pathogenesis, molecular profile and the differential diagnoses. Histology and histopathology. 2023 Feb:38(2):139-153. doi: 10.14670/HH-18-486. Epub 2022 Jun 29 [PubMed PMID: 35766228]