Introduction
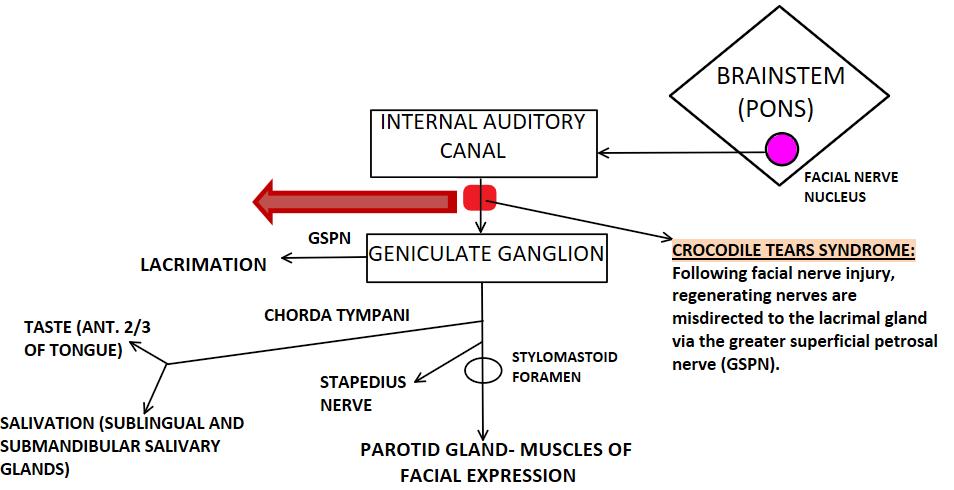
The term “crocodile tears” is derived from the ancient belief that crocodiles weep after killing their victims. “crocodile tears syndrome,” also known as Bogorad syndrome, is the shedding of tears while eating or drinking in patients recovering from Bell palsy. It is also referred to as gustatory lacrimation.[1][2] See Image. Crocodile Tears Syndrome.
Anatomy
The anatomy of the facial nerve is a mixed nerve that has motor, sensory, and parasympathetic components.
The facial nerve has the following functional components:
- The special visceral efferent component (branchial motor) innervates the muscles of facial expression, stylohyoid, posterior belly of digastric, and the stapedius muscle, which are derived from the second branchial arch.
- General visceral efferent (visceral motor) gives autonomic (parasympathetic) innervation to the lacrimal, salivary, and mucosal glands.
- Special visceral afferent (special sensory) carries taste sensation from the anterior two-thirds of the tongue.
- General somatic afferent (general sensory) carries sensation from the skin of the concha of the external ear.
Facial Nerve Nuclei
The facial motor nucleus is a collection of lower motor neurons in the lower part of the pons innervating the muscles of facial expression and stapedius. The part of the nucleus supplying the muscles of the lower half of the face receives cortico-nuclear innervation from the opposite hemisphere, whereas the part of the nucleus supplying the muscles of the upper part of the face receives bilateral corticonuclear innervation.
Behind the motor nucleus are the superior salivatory and lacrimatory nuclei, which are parasympathetic. The superior salivatory nucleus receives information from the hypothalamus and taste sensation from the oral cavity. It innervates the submaxillary and sublingual salivary glands via preganglionic fibers.
The lacrimatory nucleus receives information related to emotional responses from the hypothalamus. Information from the sensory nuclei of the trigeminal nerve is also received by the lacrimatory nucleus, which brings about reflex lacrimation upon irritation of the cornea or conjunctiva.
Facial Nerve Course and its Branches
The facial nerve consists of a motor and sensory root. The motor root loops around the abducens nucleus in the floor of the fourth ventricle and emerges at the junction of the pons and medulla along with the sensory root. The 2 roots travel along with the eighth cranial nerve to reach the internal acoustic meatus, and the 2 roots fuse at the lower part of the meatus to form a single trunk. Within the meatus, the nerve gets divided into three parts by 2 bends, following which it exits the skull via the stylomastoid foramen. The facial nerve then crosses the stylomastoid process and enters the parotid gland at its posteromedial surface. It divides into its terminal branches at the angle of the mandible:
- Temporal branches
- Zygomatic branches
- Buccal branches
- Mandibular branch
- Cervical branch
Branches Within the Facial Canal
- Greater (superficial) petrosal nerve arises from the geniculate ganglion. It carries parasympathetic preganglionic fibers and continues as the nerve of the pterygoid canal finally synapses with the pterygopalatine ganglion. Postganglionic fibers from the pterygopalatine ganglion synapse with mucosal glands of the nose, palate, pharynx, and also lacrimal gland.
- The nerve to the stapedius supplies the stapedius muscle, which dampens excess vibrations of the stapes muscle.
- Chorda tympani carries taste from the anterior two-thirds of the tongue to the brain via the middle ear.
Anatomically, the facial nerve (nervus intermedius) contains fibers for both the submandibular salivary gland and the lacrimal gland. After the facial nerve passes through the geniculate ganglion, the secretomotor fibers for the submandibular salivary gland travel with the main nerve trunk, whereas the secretory fibers to the lacrimal gland disaffiliate from the facial nerve to join the greater petrosal nerve. These secretory fibers then relay in the sphenopalatine ganglion before innervating the lacrimal gland.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
There are different theories regarding the cause of crocodile tears syndrome. The widely accepted theory is due to Bell palsy or traumatic disruption of the nervus intermedius.
Epidemiology
Bell palsy is facial nerve palsy leading to facial muscle weakness due to an unknown cause. Nemet et al. found the incidence of Bells Palsy to be 0.08% per year, and usually, the incidence increases with age (fourth to sixth decades of life).[3] In a study published by Valenca et al., females were found to be more affected by Bell palsy, and the left eye was more frequently involved as compared to the right.[4] Crocodile tears syndrome is a complication occurring of Bell palsy with an incidence of 3.3%.[4] As stated by Yamamoto et al., crocodile tears syndrome occurs approximately 6 to 9 months after Bell palsy.[5]
Pathophysiology
In the recovery period following facial nerve injury, the regenerating salivary nerve fibers undergo synkinesis or are misdirected to ultimately innervate the lacrimal gland instead of the submandibular gland. As shown in the figure below, the regenerating nerves are directed toward the lacrimal gland via the greater superficial petrosal nerve (GSPN). The result is that any stimuli, such as the smell or taste of food, instead of causing salivation, excites the lacrimal gland to produce ipsilateral tearing.[6]
Another theory put forth by Spiers et al. is a congenital abnormality. The finding supported this that few patients with crocodile tears syndrome also had underlying lateral rectus palsy or co-existing with Duane retraction syndrome. It was suspected that the lesion was in the pons adjacent to the abducens nerve.[6] Another mechanism for crocodile tears syndrome is thought to be the formation of an artificial synapse at the injury site. This synapse allows the impulses to jump from one fiber to another, and crossovers are likely, leading to crocodile tears syndrome.[7]
History and Physical
Crocodile tears syndrome involves unilateral lacrimation or tearing whenever the patient eats or drinks. However, bilateral cases have also been recorded by Speirs et al.[6] On clinical and slit-lamp examination of the eye and the lacrimal appendages, it appears within normal limits. This rules out other causes of epiphora, such as lacrimal duct obstruction, chronic dacryocystitis, punctal stenosis, conjunctivitis, and foreign body in the conjunctiva. Crocodile tears syndrome is mostly a diagnosis of exclusion in patients with a prior history of facial nerve palsy. Patients with a previous incidence of Bell palsy may give a history of acute-onset symptoms of neck, mastoid, or ear pain, altered taste or facial sensation, and hyperacusis.
Evaluation
Crocodile tears syndrome is a diagnosis of exclusion. Slit lamp examination of the eye and appendages is usually done to rule out other causes of epiphora. The basal tear secretion of an individual can be assessed by using Schirmer's test. In the case of crocodile tears syndrome, it can be performed before and after gustatory stimulation to document increased tearing after salivation. It is also important to rule out other differentials.
- Orbicularis oculi weakness due to facial palsy: The orbicularis oculi muscle is tested by asking the patient to shut his or her eyes tightly while the examiner tries to open them. The force required to open the eyelid can be graded, and accordingly, the degree of muscle weakness can be ascertained.
- Paralytic ectropion: The examiner performs the snap-back test to check for lower lid laxity. A positive test is obtained when the eyelids spring back immediately into their original position after being pulled down by the examiner.
- Nasolacrimal duct obstruction: ROPLAS (regurgitation on pressure over lacrimal sac) test is used to ascertain nasolacrimal duct obstruction.
Treatment / Management
Historically, many different treatment options have been used to stop lacrimation. A 5% solution of guanethidine was used to block the adrenergic receptors in the lacrimal gland.[6] Peroral treatment with propantheline bromide 30 mg was also tried.[6] It was also believed that instilling 1% homatropine hydrobromide in the conjunctival sac would lead to secretomotor nerve blockade.[6]However, the side effects of these pharmacological modulations outweighed their therapeutic outcome, and thus, presently, they are not the preferred line of treatment. (B3)
Surgical options include excision of the palpebral lobe of the lacrimal gland, cutting of the chorda tympani nerve, denervation of the lacrimal gland either by dissection or diathermy, and sphenopalatine ganglion blockage by alcohol or cocaine, and vidian neurectomy.[6] Nevertheless, these options are redundant, drastic, and have persistent side-effects such as vision loss and total ablation of the lacrimal gland.(B3)
The treatment of crocodile tears syndrome depends on the severity of the hyperlacrimation and the need of the patient. Mild cases are generally managed by counseling and regular monitoring. Less drastic surgical options are used, and they are proving to be an effective way to control the tearing. Subtotal resection of the palpebral lobe of the lacrimal gland is considered beneficial by McCoy et al., and pre-operative Schirmer’s test helps to control the amount of gland to be resected and thus prevent dry eye.[1] (B3)
The most widely accepted treatment of crocodile tears syndrome is botulinum toxin injection into the lacrimal gland.[8] Botulinum toxin-A is an acetylcholine release inhibitor and acts at the neuromuscular junction. It acts by stopping transmission along the aberrantly regenerated parasympathetic nerve fibers to the affected gland. It can be administered both transcutaneously and transconjunctivally to the lacrimal gland in crocodile tears syndrome patients.[7] The botulinum toxin dose injected into the lacrimal gland is 2.5 units, and its effect lasts for around 6 months.[8] The transconjunctival route of injection into the palpebral route is proven to have lesser complications than injecting transcutaneously. Montoya et al. report that the injection of botulinum toxin into the lacrimal gland in crocodile tears syndrome is a safe and effective method for treating excessive tearing.[7](B3)
Differential Diagnosis
The diagnosis of crocodile tears syndrome should be considered after excluding common differential diagnoses such as simple epiphora following Bell palsy.[9] This occurs due to loss of tone of the orbicularis oculi muscle, which leads to sagging of the lower eyelid. As the lower lid is not apposed to the eye, the normal tears cannot drain through the punctum, and they spill over, resulting in the watering of the eye.
Other differentials include nasolacrimal duct obstruction, conjunctivitis, and allergies. These conditions are not associated with hyperlacrimation, and typically the patient will give no history of increased tearing while eating food. Furthermore, in crocodile tears syndrome, the clinical examination of the eye and its appendages will be within normal limits. Also, a latency of 6 months is usually present between the onset of facial nerve palsy and crocodile tears syndrome for the nerves to regenerate.[9]
Enhancing Healthcare Team Outcomes
Since crocodile tears syndrome is a rare syndrome, it is important that it is correctly diagnosed at its onset and improve patient outcomes. At times, if the symptoms of Bell palsy are not bothersome for the patient, they frequently opt for only periodic monitoring of the condition. This was observed in a 74-year-old female in Brazil who did not get the correct diagnosis of crocodile tears syndrome for nine years.[10] (Level III)
One study on punctoplasty revealed that mild grades of punctal stenosis could be managed with rectangular 3-snip punctoplasty, but in patients with high-grade punctal lesions, there was a high recurrence rate of functional epiphora and punctal restenosis.[11]
Hence, it is important to increase awareness and knowledge about crocodile tears syndrome among physicians, physician assistants, nurse practitioners, oral and maxillofacial surgeons, and dentists who may come across these cases on a regular basis. Further, they must be able to educate patients and their families. More important, an interprofessional approach to problems of the eye can also result in early detection of other nasolacrimal duct lesions like cancers.[12] [Level 3]
Media
References
McCoy FJ, Goodman RC. The crocodile tear syndrome. Plastic and reconstructive surgery. 1979 Jan:63(1):58-62 [PubMed PMID: 432324]
Level 3 (low-level) evidenceMorais Pérez D, Dalmau Galofre J, Bernat Gili A, Ayerbe Torrero V. [Crocodile tears syndrome]. Acta otorrinolaringologica espanola. 1990 May-Jun:41(3):175-7 [PubMed PMID: 2261223]
Level 3 (low-level) evidenceNemet AY, Vinker S. Considerations and complications after Bells' palsy. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2015 Dec:22(12):1949-53. doi: 10.1016/j.jocn.2015.04.030. Epub 2015 Aug 24 [PubMed PMID: 26314659]
Valença MM,Valença LP,Lima MC, [Idiopathic facial paralysis (Bell's palsy): a study of 180 patients]. Arquivos de neuro-psiquiatria. 2001 Sep [PubMed PMID: 11593275]
Yamamoto E, Nishimura H, Hirono Y. Occurrence of sequelae in Bell's palsy. Acta oto-laryngologica. Supplementum. 1988:446():93-6 [PubMed PMID: 3166596]
Spiers AS. Syndrome of "crocodile tears". Pharmacological study of a bilateral case. The British journal of ophthalmology. 1970 May:54(5):330-4 [PubMed PMID: 5428665]
Level 3 (low-level) evidenceMontoya FJ, Riddell CE, Caesar R, Hague S. Treatment of gustatory hyperlacrimation (crocodile tears) with injection of botulinum toxin into the lacrimal gland. Eye (London, England). 2002 Nov:16(6):705-9 [PubMed PMID: 12439663]
Level 3 (low-level) evidenceNava-Castañeda A,Tovilla-Canales JL,Boullosa V,Tovilla-y-Pomar JL,Monroy-Serrano MH,Tapia-Guerra V,Garfias Y, Duration of botulinum toxin effect in the treatment of crocodile tears. Ophthalmic plastic and reconstructive surgery. 2006 Nov-Dec [PubMed PMID: 17117101]
GOLDING-WOOD PH. Crocodile tears. British medical journal. 1963 Jun 8:1(5344):1518-21 [PubMed PMID: 13948740]
Level 3 (low-level) evidencede Oliveira D, Gomes-Ferreira PH, Carrasco LC, de Deus CB, Garcia-Júnior IR, Faverani LP. The Importance of Correct Diagnosis of Crocodile Tears Syndrome. The Journal of craniofacial surgery. 2016 Oct:27(7):e661-e662 [PubMed PMID: 27536922]
Ali MJ, Ayyar A, Naik MN. Outcomes of rectangular 3-snip punctoplasty in acquired punctal stenosis: is there a need to be minimally invasive? Eye (London, England). 2015 Apr:29(4):515-8. doi: 10.1038/eye.2014.342. Epub 2015 Jan 23 [PubMed PMID: 25613844]
Level 2 (mid-level) evidenceEl-Sawy T,Frank SJ,Hanna E,Sniegowski M,Lai SY,Nasser QJ,Myers J,Esmaeli B, Multidisciplinary management of lacrimal sac/nasolacrimal duct carcinomas. Ophthalmic plastic and reconstructive surgery. 2013 Nov-Dec [PubMed PMID: 24195987]
Level 2 (mid-level) evidence