Introduction
As innovative technology has progressed throughout the field of medicine, so too has the ability to visualize the heart and its vasculature noninvasively. Several cardiac imaging modalities have become essential in the practice of modern cardiovascular medicine not only in diagnosis but also in the management of various cardiovascular diseases as well as in the guidance of invasive procedures. These modalities include echocardiography, myocardial perfusion imaging via nuclear scintigraphy, magnetic resonance imaging (MRI), and computed tomography (CT). The gold standard imaging modality for the visualization of the coronary arteries remains the invasive technique of coronary angiography via coronary catheterization. Each modality can be used individually or in combination depending on desired diagnostic needs. These studies are now routinely used together with history taking, physical examination, laboratory testing and have come to define the practice of modern cardiovascular medicine. Additionally, appropriateness guidelines for the use of these imaging techniques are now standard in the assessment of the ideal imaging modality to be used in specific patient situations to optimize diagnostic and cost efficiency as well as minimize risk to the patient.[1][2][3][4]
Equipment
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Equipment
Echocardiography uses high-frequency sound waves, essentially ultrasound, to penetrate the body and bounce off structures of interest to produce an image (see Image. Echocardiography Is Central to Cardiac Imaging). Transducers emit sound waves that are sensed by the receiver up to one hundred frames per second, making it possible to generate moving images in real time. Fluid or blood appears black. Reflective surfaces such as calcified structures appear white while muscle tissue appears gray. Transthoracic echocardiography involves the combination of multiple images from various scanning locations on the chest wall. A variation of transthoracic echo is the transesophageal echo in which the transducer is placed on an endoscope that is inserted into the esophagus. This allows for better visualization of cardiac structures with less obstruction from the chest wall, muscles, and ribs. The need for less penetration allows for better image quality and spatial resolution of various cardiac structures. Transesophageal echocardiography requires both topical anesthetics of the oropharynx and sedation of the patient. The procedure is usually performed under conscious sedation. Consent is required, and the patient needs continuous monitoring during as well as following the procedure in the recovery period.[5][6]
In addition to imaging, echocardiography can determine the velocity of blood flow through the heart and vessels via its Doppler function. Pressure differences between chambers and even valves can be determined using the velocity. Doppler helps visualize not only blood flow but also identifies turbulent regions of accelerated flow. This can be used to determine valvular insufficiency. Stress (either exercise or pharmacologic) echocardiography is routinely used to evaluate cardiac function in the setting of exercise. Three-dimensional echocardiography is a newer echocardiographic technique that allows for the acquisition of three-dimensional datasets that can be analyzed and can specifically assess chamber volumes, valvular abnormalities, and other structural pathology. Additionally, strain rate imaging is a method used for measuring a regional or global deformation of the heart muscle to assess the change in shape and dimensions during the cardiac cycle.
Classical echocardiographic equipment has been large and confined to special rooms dedicated to performing tests. Over the last several years, smaller portable ultrasound equipment has become available to be used at the bedside and can even be carried during medical rounds. Although most handheld devices lack all the functionality of their larger counterparts, they are often able to provide crucial information rapidly and efficiently.
Nuclear imaging involves the injection of intravenous radioactive tracers that become trapped in the myocytes after traveling through the vasculature surrounding the myocardium. Various tracers are used depending on their half-life and the diagnostic purpose of the study. These radioactive tracers emit radioactive rays that can be detected by specialized scanners that can convert the rays into perfusion images of the heart. Like with echocardiography, nuclear imaging can be performed during stress (either exercise or pharmacologic) to assess for evidence of ischemia.
Cardiac computed tomography uses multiple x-ray beams from a CT scanner at various angles to create cross-sectional images. The x-ray beams pass through the body and are collected by a detector array that can generate an image. Depending on the path of the beam through tissues of varying densities, a gray scale is created. Bone appears white; the air is black, blood and muscle are various shades of gray. To better differentiate the cardiac chambers from the vascular structures, contrast is often used. These images can also be used to produce a three-dimensional image of the heart. CT coronary angiography uses contrast dye to produce a three-dimensional image of the heart vasculature without the need for invasive coronary catheterization.[7]
Cardiac magnetic resonance imaging (CMR) takes advantage of protons in hydrogen molecules to create an image. The human body is made up of a majority of water. Therefore hydrogen molecules are plentiful. An MRI machine creates a magnetic field and alters the spin of the protons. Depending on the surroundings, the frequencies of the spins change. These frequencies are detected, and an image is reconstructed. The cardiac structure is very well-visualized with MRI. The contrast between tissue and vasculature is more pronounced than cardiac CT.
Invasive cardiac catheterization is an invasive technique utilizing a fluoroscopic technique that allows for the assessment of coronary anatomy and remains the gold standard in cardiac imaging. It involves gaining direct access to the coronary arteries via the peripheral anatomy usually through the wrist or the groin vessels. Percutaneous access is gained with a flexible sheath inserted into the vessel that allows for catheters to be advanced towards the heart. The catheter has diagnostic value and can be used to measure hemodynamic pressure changes in the right and left ventricle. The main diagnostic value of catheterization remains with its use for coronary angiography. With the use of contrast agents, direct visualization of the coronaries in real time during the cardiac cycle is possible. Cardiac catheterization is both diagnostic as well as therapeutic with options available for reperfusion of the myocardium with the use of balloon angioplasty and stent placement.[8]
Complications
The technique and the need for sedation during transesophageal echocardiography expose the patient to a variety of risks. These may include damage to the esophagus such as perforation, aspiration, and complications related to anesthesia. These complications are very rare, especially at experienced centers.
Cardiac CT leads to exposure to ionizing radiation, which is well-known to have harmful side effects. The risk for malignancy following exposure is difficult to determine and likely small, nonetheless remains a possibility. Risk versus benefit must be discussed when considering these imaging modalities, and consideration of cumulative exposure should also be ascertained especially with repeat imaging studies and in performing these tests in patients at a young age.
The use of contrast agents has a substantial impact on the diagnostic value of radiologic imaging and is commonly used for cardiac CT, cardiac catheterization, and CMR. The most feared complication remains contrast-induced nephropathy. In those with normal renal function, it is a self-limiting side effect. However, in those with baseline renal abnormality, especially with those that are diabetic; progression to chronic kidney disease remains high.
Cardiac magnetic resonance imaging uses a magnetic field to generate an image. As a result, the presence of metallic hardware remains a major risk during testing. In 2011, the first CMR compatible pacemaker became available, however, at this time a permanent pacemaker remains a contraindication to CMR. The same goes for implantable defibrillators.
Cardiac catheterization remains the most invasive modality and has the most potential for harmful side effects. These include as mentioned renal injury and possible renal failure from contrast exposure, myocardial infarction, stroke, induction of arrhythmias and vascular complications such as bleeding. There are no absolute contraindications to cardiac catheterization. However, relative contraindications do exist. They include decompensated heart failure, bacteremia, acute stroke, and acute renal failure.
Clinical Significance
Echocardiography allows for direct visualization of the heart including the size of the chambers, the thickness of the ventricular walls, and any structural abnormalities. It also allows for an assessment of contractility and left ventricular ejection fraction. Transesophageal echocardiography has become the test of choice for detecting valvular vegetations and thrombi within the heart. Transesophageal echo also allows visualization of the left atrial appendage, which is often too difficult to visualize with standard transthoracic echocardiography. In the setting of renal dysfunction, transesophageal echo has become the modality of choice for evaluation of aortic dissection. Stress echocardiography is routinely used to evaluate cardiac function in the setting of exercise and can determine myocardial ischemia. For those able to exercise, echocardiography is performed during the use of a treadmill or bicycle. For those unable to exercise, pharmacologic stimulation is used to simulate exercise as an echocardiogram is performed. Wall motion abnormalities are used to signify areas of possible ischemia. Echocardiography is unique in that it can provide a great deal of clinical data and remain safe without any exposure to radiation.
Radionuclide imaging is most often used for evaluation in those patients with known or suspected coronary artery disease. Nuclear imaging allows for not only diagnosis but also for risk stratification and can be used for the assessment of myocardial viability before revascularization. Radioactive tracers mark areas where blood can reach the capillaries, a sign of myocardial perfusion. Areas with hypoperfusion are indicative of regions of myocardial ischemia. Nuclear imaging can also be used as a stress test with imaging before and after stress again precisely marking areas of decreased perfusion as areas of ischemia.[9]
Cardiac CT allows for direct visualization of coronary vasculature in three dimensions without the need for an invasive procedure like coronary catheterization. CT also allows for calcium scoring which is the ability to detect the presence of coronary artery calcification; calcification has been associated with atherosclerosis and mortality. CT angiography has emerged as imaging study of choice for rapid assessment of cardiac vasculature especially in the setting of suspected aortic dissection given normal renal function. Newer applications utilizing cardiac CT for perfusion and fractional flow reserve are on the horizon and are set to expand the diagnostic armamentarium of cardiac CT.
Cardiovascular MRI is mainly used to assess cardiac structure as well as function. The contrast between cardiac tissue and vasculature is better visualized leading to a sharper definition when compared to cardiac CT. CMR perfusion utilizing first pass gadolinium imaging is also employed to test for myocardial ischemia and has been compared with other imaging modalities. Late gadolinium enhancement CMR is used for the identification of infarcted myocardial tissue. This technique is routinely used along with perfusion CMR to assess whether a territory in question is ischemic or infarcted (scar). Additionally, phase contrast and myocardial tagging sequences utilizing CMR allow for valvular and flow assessment as well as myocardial performance assessment in patients. CMR has a wide range of diagnostic capability. However, it requires attention to detail especially in the proper acquisition sequences used, and analysis of these images is reserved to be performed in centers with clinical training and expertise in this imaging modality.[10]
Coronary angiography via cardiac catheterization allows for the comprehensive evaluation of coronary anatomy and severity of cardiac disease. Not only does it allow for visualization but also allows for interventions to reperfuse the myocardium. Cardiac catheterization is the treatment of choice in emergency situations such as acute myocardial infarction and therefore remains the gold standard for assessment of coronary anatomy. Intravascular ultrasound is an invasive technique utilized during cardiac catheterization that uses ultrasound to visualize the lumen and the wall of blood vessels. This can be especially useful in the assessment of plaques in the arteries that may be significant but are not causing major stenosis to blood flow. Another complementary technique used during cardiac catheterization is fractional flow reserve assessment. Fractional flow reserve determines the ratio between the achieved blood flow in a stenosed coronary artery and the expected maximum flow in a normal coronary artery. By this measurement, a luminal stenosis which may be borderline (approximately 40% to 60%) can be functionally assessed to determine its clinical hemodynamic significance. Finally, transcatheter structural invasive procedures are now performed (for example, transcatheter aortic valve replacement or transcatheter mitral valve repair). These procedures are generally guided by noninvasive cardiac imaging both before the procedure for patient evaluation and selection (transthoracic and transesophageal echocardiography, cardiac CT, cardiac MRI), during the procedure for direct guidance (transesophageal echocardiography), and after the procedure for survey of the procedure results and possible complications (echocardiography).
Enhancing Healthcare Team Outcomes
When patients present with symptoms of heart disease, the primary care provider, nurse practitioner, internist and the emergency department physician have available numerous imaging methods to assess heart function. In order to avoid redundancy or duplication, it is important to consult with the cardiologist to confirm the best imaging test. The type of cardiac imaging test depends on the urgency of the problem and the symptoms.[11][12][13]
Media
(Click Image to Enlarge)
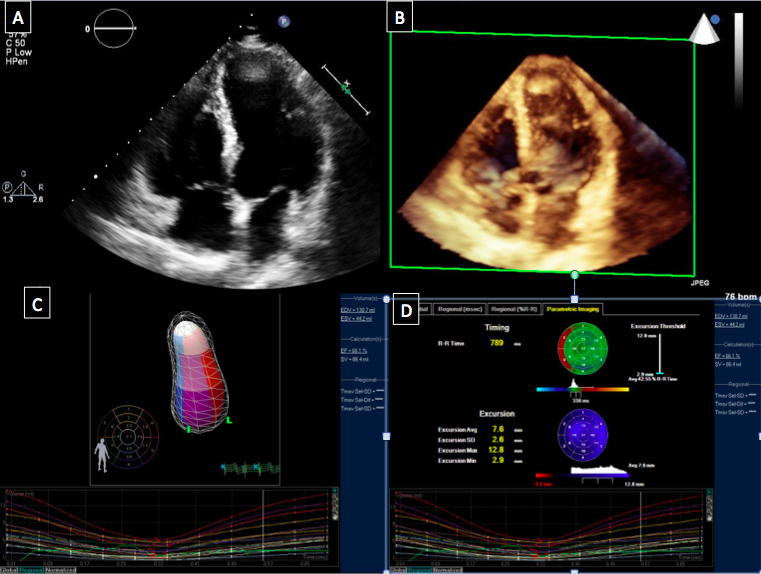
Echocardiography Is Central to Cardiac Imaging. Apical 4-chamber two-dimensional transthoracic image (A). Apical 4-chamber three-dimensional transthoracic image (B). Quantification of ventricular volume and function that is made possible by 3-dimensional imaging and advanced quantitation packages (C,D).
Contributed by A Makaryus, MD
References
Guglielmo M, Baggiano A, Muscogiuri G, Fusini L, Andreini D, Mushtaq S, Conte E, Annoni A, Formenti A, Mancini EM, Gripari P, Guaricci AI, Rabbat MG, Pepi M, Pontone G. Multimodality imaging of left atrium in patients with atrial fibrillation. Journal of cardiovascular computed tomography. 2019 Nov-Dec:13(6):340-346. doi: 10.1016/j.jcct.2019.03.005. Epub 2019 Mar 30 [PubMed PMID: 30952613]
Williams MC, Newby DE, Nicol ED. Coronary atherosclerosis imaging by CT to improve clinical outcomes. Journal of cardiovascular computed tomography. 2019 Sep-Oct:13(5):281-287. doi: 10.1016/j.jcct.2019.03.007. Epub 2019 Mar 29 [PubMed PMID: 30952611]
Level 2 (mid-level) evidenceAntoniades C, Kotanidis CP, Berman DS. State-of-the-art review article. Atherosclerosis affecting fat: What can we learn by imaging perivascular adipose tissue? Journal of cardiovascular computed tomography. 2019 Sep-Oct:13(5):288-296. doi: 10.1016/j.jcct.2019.03.006. Epub 2019 Mar 29 [PubMed PMID: 30952610]
Singh M, Sporn ZA, Schaff HV, Pellikka PA. ACC/AHA Versus ESC Guidelines on Prosthetic Heart Valve Management: JACC Guideline Comparison. Journal of the American College of Cardiology. 2019 Apr 9:73(13):1707-1718. doi: 10.1016/j.jacc.2019.01.038. Epub [PubMed PMID: 30947924]
Pettemerides V, Turner T, Steele C, Macnab A. Does stress echocardiography still have a role in the rapid access chest pain clinic post NICE CG95? Echo research and practice. 2019 Jun 1:6(2):17-23. doi: 10.1530/ERP-18-0082. Epub [PubMed PMID: 30893640]
Calogero E, Fabiani I, Pugliese NR, Santini V, Ghiadoni L, Di Stefano R, Galetta F, Sartucci F, Penno G, Berchiolli R, Ferrari M, Cioni D, Napoli V, De Caterina R, Di Bello V, Caramella D. Three-Dimensional Echographic Evaluation of Carotid Artery Disease. Journal of cardiovascular echography. 2018 Oct-Dec:28(4):218-227. doi: 10.4103/jcecho.jcecho_57_18. Epub [PubMed PMID: 30746325]
Rischpler C, Woodard PK. PET/MR Imaging in Cardiovascular Imaging. PET clinics. 2019 Apr:14(2):233-244. doi: 10.1016/j.cpet.2018.12.005. Epub 2019 Feb 1 [PubMed PMID: 30826021]
Yannopoulos D, Bartos JA, Aufderheide TP, Callaway CW, Deo R, Garcia S, Halperin HR, Kern KB, Kudenchuk PJ, Neumar RW, Raveendran G, American Heart Association Emergency Cardiovascular Care Committee. The Evolving Role of the Cardiac Catheterization Laboratory in the Management of Patients With Out-of-Hospital Cardiac Arrest: A Scientific Statement From the American Heart Association. Circulation. 2019 Mar 19:139(12):e530-e552. doi: 10.1161/CIR.0000000000000630. Epub [PubMed PMID: 30760026]
Wu J, Liu C. Recent advances in cardiac SPECT instrumentation and imaging methods. Physics in medicine and biology. 2019 Mar 13:64(6):06TR01. doi: 10.1088/1361-6560/ab04de. Epub 2019 Mar 13 [PubMed PMID: 30726779]
Level 3 (low-level) evidenceBhatia S, Anstine C, Jaffe AS, Gersh BJ, Chandrasekaran K, Foley TA, Hodge D, Anavekar NS. Cardiac magnetic resonance in patients with elevated troponin and normal coronary angiography. Heart (British Cardiac Society). 2019 Aug:105(16):1231-1236. doi: 10.1136/heartjnl-2018-314631. Epub 2019 Apr 4 [PubMed PMID: 30948519]
Misra A, Sriram C, Gupta P, Humes R. The Adult with Post-operative Congenital Heart Disease: a Systematic Echocardiographic Approach. Current cardiology reports. 2019 Mar 18:21(5):29. doi: 10.1007/s11886-019-1116-x. Epub 2019 Mar 18 [PubMed PMID: 30887232]
Level 1 (high-level) evidenceZoghbi WA, Asch FM, Bruce C, Gillam LD, Grayburn PA, Hahn RT, Inglessis I, Islam AM, Lerakis S, Little SH, Siegel RJ, Skubas N, Slesnick TC, Stewart WJ, Thavendiranathan P, Weissman NJ, Yasukochi S, Zimmerman KG. Guidelines for the Evaluation of Valvular Regurgitation After Percutaneous Valve Repair or Replacement: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Angiography and Interventions, Japanese Society of Echocardiography, and Society for Cardiovascular Magnetic Resonance. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2019 Apr:32(4):431-475. doi: 10.1016/j.echo.2019.01.003. Epub 2019 Feb 20 [PubMed PMID: 30797660]
Gill EA, Blaha MJ, Guyton JR. JCL roundtable: Coronary artery calcium scoring and other vascular imaging for risk assessment. Journal of clinical lipidology. 2019 Jan-Feb:13(1):4-14. doi: 10.1016/j.jacl.2019.01.008. Epub [PubMed PMID: 30773212]
