Introduction
The pelvic floor is a unique anatomical location where the balance of the different pressures, either visceral, muscular, or liquid play a fundamental role in the physiological functioning of all the structures contained therein. The pelvis is bounded superiorly by the imaginary line between the pubis and sacral promontory and inferiorly as the line between the ischial tuberosity and the apex of the coccyx, which separates the pelvis from the perineum below. [1][2][3] From an anatomical standpoint, the pelvic floor can be divided into 4 compartments:
- Anterior or urinary (bladder, bladder neck, and urethra)
- Medium or genital (vagina and uterus in women, prostate in men)
- Posterior or anterior (anus, anal canal, sigmoid, and rectum)
- Peritoneal (endopelvic fascia and perineal membrane)
The functional classification of the pelvis is as follows:
- Diaphragm or pelvic floor (ischiococcygial muscle and levator ani muscles), closed above by the endopelvic fascia.
- The urogenital diaphragm (triangular ligament/fascia of Carcassonne) is located caudally between the ischium and the pubic symphysis and crossed by the urethra and the vagina.
- The perineum or perineal membrane is the continuation of the Carcassonne fascia, connecting the deep layer of the pelvic floor musculature, the coccyx, and the anal sphincter.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Respiration
At rest, the pelvic floor maintains a cupuliform shape resembling the respiratory diaphragm and on contraction, the pelvic floor ascends anterosuperiorly (toward the pubis) and while on relaxation, it moves in a posteroinferior direction (toward the sacral bone and the ischium) with a displacement of about 3 cm. During this action, the coccyx undergoes anterosuperior and posteroinferior motion. The pubococcygeal line is measured between the pubic symphysis and the coccyx, while the anorectal angle is considered as the angle between the posterior margin of the rectum and the line running through the central axis of the anal canal. Both of these parameters can be measured using MRI (magnetic resonance imaging) of the pelvis. In healthy patients, the base of the bladder, the upper third of the vagina, and the peritoneal cavity must be on or adjacent to the pubococcygeal line, with the anorectal angles cranial or adjacent to the previously mentioned line. When the pelvic floor contracts, the viscera ascend and the anorectal angle becomes acute. The pelvic floor supports the male and female viscera and the rectum, allowing for optimal contraction. With contraction and relaxation, the musculature creates a series of pressure changes that assist the viscera in their respective functions. A proper contraction of the pelvic floor also allows sexual function and sexual activity. When the respiratory diaphragm is lowered by inhalation, the pelvic diaphragm moves caudally, thus allowing the respiration to encounter less resistance; while the opposite movement occurs during exhalation. Hence, the pelvic diaphragm influences breathing with its contractile status.[4][5]
Posture
Another important function of the pelvic floor is the postural one, again together with the respiratory diaphragm and abdominal muscles. Muscle groups able to hold the thoracolumbar and lumbosacral column must be activated to allow twist movements of the trunk, to stand up or sit or simply to stay in orthostatism, and to cough and sneeze. Specifically, all the abdominal muscles (respiratory diaphragm, transverse and oblique), the pelvic floor (and other connected muscles such as obturators, piriformis, adductors), and the large gluteus must be simultaneously activated. There is myofascial continuity among the muscular mentioned districts. The diaphragm muscle, through the transverse muscle and the fascia, transversalis anteriorly, and the thoracolumbar fascia posteriorly merges with the anterior margin of the pelvic floor (pubis) and the posterior one (sacrum). The rectus abdominis and its fascial system merge at the level of pubic symphysis with the adductor muscles, both activated by the contraction of the pelvic floor. The pelvic floor is in anatomical continuity with the large gluteus, also involved in the pelvic contractions. Pelvic floor contractions allow the distribution of loads from the trunk and upper limbs to the lower limbs and vice versa during walking and in orthostatism, thanks to the mentioned anatomical connections. The same foot position is affected by the muscular tension of the pelvic floor, which affects the tone of the rotator muscles of the hip; the pelvic floor tension will affect the behavior of the adjacent contractile districts.
Embryology
From an embryological point of view, the muscular pelvic part, in conjunction with the first sketches of the pelvic organs, is formed by two distinct muscle groups: the pubocaudal muscle and the muscle of Gegenbauer (close to the cloaca).
The first group will form the ischio-coccygeal and the levator ani muscle, the pubosacral or pubourethral-bladder-rectosacral ligaments in the man and pubourethral-bladder-uterus-rectosacral ligament in the woman. The second group will form, after the descent of the genito-urinary septum (that separates the rectum posteriorly from the bladder and urethra in the man and urethra and vagina in the woman), the sphincter muscles (the anus and the urethra) and the bulbocavernosus, ischiocavernosus and superficial and deep transverse muscles. In the fetus, these muscular and ligamentous structures present themselves as a unity, synergistic in their contractions and functions.
Blood Supply and Lymphatics
The most important artery is the internal pudendal artery. It originates from the internal iliac artery, then divides into the lower rectal arteries and perineal arteries. Anteriorly, we find the urethral artery, the arteries of the penis (for the man), the arteries of the bulb of the vestibule and the arteries of the clitoris (for the woman). Internal pudendal veins connect to the internal iliac vein in the pelvis. The external pudendal veins, anteriorly, connect to the femoral vein of the thigh.
The deep lymphatic vessels flow mainly into the internal iliac lymph nodes in the pelvis. Lymphatic vessels from the genitals flow into the superficial inguinal lymph nodes.
Nerves
Pelvic muscle innervation is complex, involving the autonomic and somatic system: the superior hypogastric plexus with hypogastric nerves, the pelvic splanchnic nerves, and the inferior hypogastric (pelvic) plexus; the pudendal nerve. The autonomic system, especially the parasympathetic plexus, creates synapses with the myenteric plexus of the rectum and anal canal. Pelvic musculature has voluntary and involuntary control. The pelvic floor can be induced to contract consciously, such as during physiotherapy, or to act automatically, such as during arm movements, breathing, coughing, lower limbs and trunk muscles. Neural centers for such automatic synergies are little understood. Pelvic musculature is represented in the medial wall of the precentral gyrus, where it is triggered by both voluntary movements and movements of other muscles of the pelvis. This means that there is a pre-activation of the premotor cortex, but this activation only concludes if the upper centers ensure that the contraction is necessary. Another area involved in involuntary movements of the pelvic floor associated with breathing, involving the respiratory diaphragm, the abdominal wall and the tongue (during inspiration retrudes as it expires with the exhalation), is the retro ambiguous nucleus of the medulla oblongata. The neurological mechanisms involved in this are not clear.[6][7]
Muscles
The pelvic diaphragm, first named in 1861, consists of the levator ani, formed by the coccygeus muscle or ischio coccygien, ileo coccygien, pubococcygeus muscles, and the puborectal muscle.[8][9][10]
The first 3 originate from the pectineal line of the pubic bone and from the fascia of the obturator muscle, to fit the coccyx, through the ischiatic spine, the ileum and sacrum, and the triangular ligament (or urogenital diaphragm); the puborectal muscle involves the lower middle portion of the pubic branch. Pubococcyx and rectal muscles are also called pubovisceral muscles since contractile filaments are directly linked to the urethra, vagina, perineal body, and anal canal, respectively such as pubourethral, pubovaginal, puboperinal, and puboanal muscles.
About two-thirds of the contractile fibers of these muscles are red aerobic or type 1 fibers, while the rest is formed by anaerobic white fibers or type 2. These muscles work as a single unit and are difficult to distinguish separately; furthermore, the vectorial direction of their fibers is hard to describe because they work in all planes in a functional and anatomical tridimensionality. From tractography, we can derive the organization of contractile fibers, where musculature appears as a work of art.
The Urogenital Diaphragm
The urogenital diaphragm, placed beneath the pelvic floor, is constituted by the perineal media aponeurosis or fascia, including the deep transverse muscle of the perineum; is a reinforcement that joins the pelvic diaphragm to the perineum. Its anterior part is crossed by the urinary and genital tracts, lying between the 2 ischiopubic branches and pointing at the apex toward the pubic symphysis. The pre-urethral area or transverse ligament of the perineum keeps in touch with the ischiopubic branches and the obturator band, while the retro-urethral area is divided into 2 layers (superior and inferior), with Guthrie's muscle or deep transverse perineum muscle placed between. The upper aponeurotic lamina continues towards the transverse perineal muscle, while the deeper lamina blends with the band of Denonviller, with the latter covering the prostate and the seminal vesicles.
The Perineum
The perineum is the continuation of the urogenital diaphragm posteriorly and of the elevator ani muscle inferiorly, very difficult to be delimitated; it connects with muscular fibers the urethra, the vagina or the prostate, and the rectum, up to the coccyx with an ano-coccygien Rafe. The muscles and the viscera are immersed in a web of connective tissue or fascia, where just as the spider perceives the prey imprisoned thanks to the movements; all the structures immersed and wrapped in the fascia perceive the changes of tension and function in a continuum which respects the concept of biotensegrity. The fascia is a mechanical transmission force instrument that involves the entire body system; a cervical flexion movement, for example, involving the deep cervical fascia, will affect the position of the lower limb band, dragging the connective tissue upward. The fascial system precedes the birth and organization of contractile districts.
The Endopelvic Fascia
Below the peritoneum the endopelvic fascia covers the upper area of the pelvic floor: it covers the inner obturator, the piriformis, the elevator ani, to continue with the transversal band merging into the pubic periosteum. In its path it merges with the pubosacral ligament posteriorly, building a connective cup covering the entire musculoskeletal structure of the pelvic floor, the urogenital diaphragm, and perineal area. The endopelvic fascia encapsulates the viscera of the pelvic floor, further connecting them with musculature and bone structures. It guides the vascular structures in connective sheaths such as the hypogastric sheath (which connects the pubic bone to the sacrum), the umbilical-prevesical sheath (which delimits the retropubic space), the vesicorectal sheath for the vesicular-deferential arteries, and the fascia mentioned above of Denonvillier wrapping the two middle hemorrhoidal arteries.
Clinical Significance
A deficiency in pelvic floor muscle tension or an electrical abnormality of these districts will cause many disorders and pathologies, including visceral prolapse and urinary incontinence and fecal constipation. It is estimated that pelvic floor muscle disorders will increase by 35% over the next two decades, to an average of around 1.6 million visits per year for 2030. Pathogenesis is highly variable and multifactorial:
- Birth injury
- Elderly age
- Obesity
- Chronic pathological conditions that cause an increase in abdominal pressure
- Previous surgical interventions in the pelvic area
The major problems encountered in the anterior compartment include dysuria, urinary frequency, cystocele, and urinary incontinence. Vaginal or uterine prolapse usually represents central compartmental disorders. Changes in the posterior region cause pelvic and/or anal pain, constipation, rectal prolapse, and fecal incontinence. Peritoneal compartment disorders can lead to dyspareunia, constipation and low back pain due to alterations in rectum and sigma.
The Stress Urinary Incontinence
Pelvic floor issues may involve a few districts or all of them. The stress urinary incontinence (SUI), the most common of incontinence forms, occurs in the presence of stimuli such as a cough or sneezing, conditions where the increased pressure inside the pelvic cavity exceeds the muscular control ability. SUI affects about 26% of women between 30 and 59 years of age, with a peak at 40 to 49 years. The causes do not only affect the levator ani but its interaction with the adjacent muscles and joints. There is evidence that the pelvic floor acts in opposition to the respiratory diaphragm. The pelvic floor cannot properly distribute the tensions produced during trunk/ limb movements. There is a decreased electrical activity and/or electrical dissipation in the use of the muscles. A postural alteration of the lumbar spine alters the electrical behavior of the floor. The lack of pelvic tilt for lumbar hypolordosis (the pelvis is inclined posteriorly, the sacrum is displaced anteriorly in flexion, and the pubis oriented in anterior-inferior direction) cause an increase in the vertical load to the pelvic muscles, stretching the muscle fibers each time an individual walks or runs. This condition will progressively lead to the weakness of the levator ani. In healthy people with hypolordosis, visceral pressures in the pelvic cavity in the orthostatism increase, as there is an increase in the electromyographic spectrum of the elevator. Clinicians think that these events have a negative effect on continence in subjects with pelvic floor disorders. SUI in men is related to previous surgical prostatectomy.
The Prolapse of the Pelvic Organs, and Constipation
The prolapse of the pelvic organs caused by the weakness of the pelvic floor muscles is a problem affecting 30% to 50% of women, potentially leading to urinary and rectal problems, as well as disturbances to the sexual sphere. Researchers do not have accurate data on rectal prolapse in men. Constipation affects about 27% of the population, especially women, whose main causes can be related to the pelvic floor, to a paradoxical contraction of the musculature, general muscular weakness, and incomplete relaxation after contraction. Fecal accumulation in the rectum could lead to urinary and/or visceral prolapse.
Pain
Another problem related to the pelvic floor is a pain. Several dysfunctions including interstitial cystitis/bladder pain syndrome, chronic prostatitis, provoked vestibulodynia, chronic vulvar pain disorder can present with several symptoms, but always with a single common denominator: painful muscle dysfunction (spasm, trigger point, hypotonia). Myofascial pelvic pain (MPP) affects about 14% to 23% of women, but data are underestimated, and not accurate in males. MPP presents with pain arising from muscular and connective tissue and can present as a single symptom or as a series of urological, gynecological, and colorectal symptoms. The source of pain not only involves the pelvic floor, the urogenital diaphragm, and the perineal membrane, but also some myofascial structures closely related, such as the piriformis and the internal obturator muscle. The symptoms may radiate from an initial area, affecting the gluteus, the abdomen, lumbar spine, chest, pelvis, and lower limbs. The muscle may create conditions such as the presence of trigger points (TPs). The causes are different and sometimes concomitant, such as a trauma or injury, the presence of a scar, chronically altered posture, metabolic dysfunctions and food deficiencies, and psychological stress. A constant change in the length of the muscle fibers can lead to an altered circulation, hypoperfusion, and ischemia, with the formation of TPs, even latent for many years. The pain arises when the TP is stimulated, for example, for a movement or a body function when a myofascial area is stretched or compressed. A constant stimulus of the nociceptive system forces a plastic change of the nervous structures, either peripheral or central, forming what is called central sensitization. This event results in an increased response of medullary neurons (allodynia), also persisting when the causal stimulus stops (hyperalgesia), causing an altered response from other non-injured tissues, resulting in pain (secondary hyperalgesia). The same connective tissue can be a source of pain, becoming less metabolically active and less adaptable to mechanical changes. The connective tissue can directly convey pain signals; in fact, it contains nociceptors that can translate mechanical stimuli into pain information; if there are nonphysiological mechanical stimuli, the proprioceptors can turn into nociceptors. Reduced sliding of the various layers limits the functionality of the endocannabinoid system. The fascial system is also important because it acts directly on the tension of the contractile tissue. Proprioceptors located in connective tissue (ligaments) activated by stretching, due to medullary reflex, can stimulate muscle contraction useful to suppress the tension created by the fascial fibers, ensuring the proper degree of tension and release of the muscle. An alteration in the muscle tone can cause dysfunction of the pelvic joints that, and even this condition can cause pelvic pain, as the same joints become a source of pain. A vicious circle is created where the structures used to correctly transfer the loads during movement fail in their functions, leading to further pain and symptoms. The pelvic floor with an altered status may trigger unspecific symptoms such as respiratory disorders, low back pain, sacroiliac joint pain, and pelvic girdle pain. The abnormal tension of the pelvic floor muscle can cause the same neurological compression/trapping syndromes that can be easily detected for the upper and lower limbs, such as compressing or preventing the nerves from sliding. An example is pudendal nerve syndrome or Alcock's syndrome, often negatively affected by muscular hypertonia. The pudendal nerve (S2 through S4) passes into the Alcock channel, between the sacrospinous and sacrotuberous ligament at the level of the ischiatic spine, affecting the fascia of internal obturator muscle. Its entrapment will cause unilateral genital pain to the genital area, anus, and pelvic area.
Evaluation of Pelvic Floor
A general manual and instrumental medical evaluation can be found in the literature. With regard to the manual examination, there is still no inspection technique involving all the components of the pelvic floor. The evaluation begins with an anamnestic interview and visual observation of any non-physiological change. The active movements of the lower limb, the lumbar spine, and the presence of symptoms are observed. The patient's posture, orthostatism, and walking are observed, as an altered body alignment could cause compensatory stress to the pelvic floor. The current manual evaluation focuses on measuring the ability to contract the pelvic muscle, quantifying its strength, and looking for TPs. The external tissues of the abdomen, thigh, gluteus, as well as perineal area, are tested to verify the presence of TPs. Intravaginal or rectal palpation is also performed to highlight the presence of sore areas. With the internal evaluation, a clinician can ask to contract the muscle to understand its ability to control and pain presence. Tthe Q-tip test is used to explore the presence of TPs and painful areas with intravaginal palpation. The test assigns the value of the present pain, with a minimum of zero for the complete absence of pain, and a maximum of 10 to report the worst pain as possible. To the muscle strength actively evaluated can be given a score of 0 to 5, with reference to the Chirarelli scale: zero corresponds the lack of contraction, while the maximum value of 5 indicates a physiological function of the musculature. One study proposes to evaluate the coccyx externally, placing the palm on the coccygeal area, with the sitting sit and in lateral decubitus; the patient is asked to contract the pelvic floor, following the bone movement through palpation.
Diagnostic Tools
The muscular strength of the pelvic floor can also be measured with intravaginal instruments such as manometers and dynamometers. The first measures the strength expressed in millimeters of mercury, while the second instrument calculates it in newtons. Differential tests are also performed to evaluate the presence of pain in the sacroiliac joint (SIJ), such as the Active Straight Leg Raise Test (ASLRT). ASLRT is the most important test to understand the presence of pain at SIJ and to differentiate joint dysfunction of the lumbar region and hip; it is also useful to highlight a potential dislocation of the SIJ. Intravaginal cones are intravaginal instruments that can give information on the pelvic floor contraction, and feedback on response to therapy. They have different shapes and sizes, with a dual purpose: to evaluate and help the patients to understand how they can work on their own muscles. Other medical instruments used for diagnosis are intravaginal or intracranial ultrasound, or suprapubic and perineal ultrasound, depending on the physician's decision. Ultrasound can produce 2-dimensional or 3-dimensional images, giving information on muscular and visceral behavior. Electromyography (EMG) provides information on how the pelvic floor contraction, either voluntary or not, behave. The electrodes can be superficial or intramuscular, and this depends on the area to be evaluated. These can placed on the surface for more general information, while more painful investigations are needed for deeper or more specific muscle areas. The use of the EMG and the proper reading of the spectrum depend on the position of the electrodes and the posture of the patient to be examined. EMG is less intense in the supine position and with bent legs than in sitting position and in orthostatism. The preferred diagnostic tool is magnetic resonance imaging (MRI). MRI can provide precise information on what is happening in the examined pelvic area (muscular, visceral and connective) with the ability to obtain real-time measurements of how the pelvic floor is positioned and how it contracts and how the viscera behave, without discomfort for the patient. The relaxed pelvic floor descends approximately 3 cm under the previously mentioned pubo coccygien line in healthy subjects. The choice of the use of this instrument will depend on the physician's experience. Computed Tomography (CT) can provide dynamic information on pelvic floor changes during contraction and defecation, but it represents a second choice compared to MRI for the presence of rays in the examination. In all cases, the physician decides how to orient the diagnostic procedure based on the subjective necessity of the patient.
Other Issues
Recent studies show how other muscle groups are able to directly influence the behavior of the pelvic floor. The muscle insertion of the levator ani goes beyond the superior pubic branch, entering the obturator fascia. The external stimulation of the obturators stimulated the contraction of the levator ani, in particular the anatomical area of the iliococcygeus muscle (also known as the tendon arch). [11]
Remember that the gluteus maximus muscle is also capable of influencing the muscle tension of the pelvic floor, as a tendon arch deriving from the gluteus maximus inserts directly into the levator ani muscle area. [12]
Media
(Click Image to Enlarge)
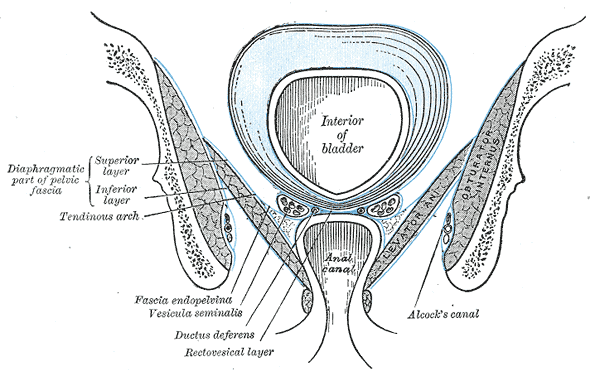
Anatomy of the Pelvic Floor, Interior of bladder, Anal Canal, Diaphragmatic part of pelvic fascia; Superior Layer and Inferior Layer, Tendinous Arch, Fascia Endopelvic, Vesicula Seminalis, Ductus Deferens, Rectovesical layer, Alcock's Canal, Obturator Internus
Henry Vandyke Carter, Public domain, via Wikimedia Commons
References
Sam P, LaGrange CA. Anatomy, Abdomen and Pelvis, Penis. StatPearls. 2024 Jan:(): [PubMed PMID: 29489230]
Simunovic M, Pinthus J, Coates AJ, DeNardi F. Anterior-entry abdominoperineal resection: a variation in the method of perineal dissection. Annals of surgical oncology. 2012 Mar:19(3):794-800. doi: 10.1245/s10434-011-2016-5. Epub 2011 Aug 23 [PubMed PMID: 21861220]
Kalra A, Wehrle CJ, Tuma F. Anatomy, Abdomen and Pelvis, Peritoneum. StatPearls. 2023 Jan:(): [PubMed PMID: 30521209]
Arbuckle JL, Parden AM, Hoover K, Griffin RL, Richter HE. Prevalence and Awareness of Pelvic Floor Disorders in Female Adolescents Seeking Gynecologic Care. Journal of pediatric and adolescent gynecology. 2019 Jun:32(3):288-292. doi: 10.1016/j.jpag.2018.11.010. Epub 2018 Dec 6 [PubMed PMID: 30529498]
Emerich Gordon K, Reed O. The Role of the Pelvic Floor in Respiration: A Multidisciplinary Literature Review. Journal of voice : official journal of the Voice Foundation. 2020 Mar:34(2):243-249. doi: 10.1016/j.jvoice.2018.09.024. Epub 2018 Nov 14 [PubMed PMID: 30447797]
Pinto RA, Corrêa Neto IJF, Nahas SC, Bustamante Lopes LA, Sobrado Júnior CW, Cecconello I. FUNCTIONAL AND ANATOMICAL ANALYSIS OF THE ANORECTUM OF FEMALE SCLERODERMA PATIENTS AT A CENTER FOR PELVIC FLOOR DISORDERS. Arquivos de gastroenterologia. 2018 Nov:55Suppl 1(Suppl 1):47-51. doi: 10.1590/S0004-2803.201800000-49. Epub 2018 Oct 4 [PubMed PMID: 30304292]
Jalalizadeh M, Alshiek J, Santoro GA, Wieczorek AP, Shobeiri SA. Six-Year Experience in Teaching Pelvic Floor Ultrasonography Using Pelvic Floor Phantoms. Obstetrics and gynecology. 2018 Aug:132(2):337-344. doi: 10.1097/AOG.0000000000002729. Epub [PubMed PMID: 29995748]
Escalona-Vargas D, Oliphant S, Siegel ER, Eswaran H. Characterizing pelvic floor muscles activities using magnetomyography. Neurourology and urodynamics. 2019 Jan:38(1):151-157. doi: 10.1002/nau.23870. Epub 2018 Nov 2 [PubMed PMID: 30387530]
Radzimińska A, Weber-Rajek M, Strączyńska A, Podhorecka M, Kozakiewicz M, Kędziora-Kornatowska K, Goch A. The impact of pelvic floor muscle training on the myostatin concentration and severity of urinary incontinence in elderly women with stress urinary incontinence - a pilot study. Clinical interventions in aging. 2018:13():1893-1898. doi: 10.2147/CIA.S177730. Epub 2018 Oct 4 [PubMed PMID: 30323575]
Level 3 (low-level) evidenceLemos AQ, Brasil CA, Alvares CM, Passos JCG, Lordêlo P, Sá KN. The relation of the pelvis and the perineal function in incontinent women: A neglected subject. Neurourology and urodynamics. 2018 Nov:37(8):2799-2809. doi: 10.1002/nau.23772. Epub 2018 Jul 19 [PubMed PMID: 30024050]
Chin HY, Peng CW, Wu MP, Chen CH, Feng YT, Fong TH. Attachment of the levator ani muscle extends to the superior ramus of the pubic bone through electrophysiological and anatomical examinations. Scientific reports. 2021 May 4:11(1):9483. doi: 10.1038/s41598-021-89041-6. Epub 2021 May 4 [PubMed PMID: 33947899]
Soljanik I, Janssen U, May F, Fritsch H, Stief CG, Weissenbacher ER, Friese K, Lienemann A. Functional interactions between the fossa ischioanalis, levator ani and gluteus maximus muscles of the female pelvic floor: a prospective study in nulliparous women. Archives of gynecology and obstetrics. 2012 Oct:286(4):931-8. doi: 10.1007/s00404-012-2377-4. Epub 2012 Jun 13 [PubMed PMID: 22692630]
