Introduction
Fine needle aspiration (FNA) is a type of biopsy that is performed with a small (21 to 25 gauge) needle to obtain samples of tissue and fluid from solid or cystic breast lesions. It is one of the many different modalities for diagnosing breast masses outside of formal excision. Other methods include core needle biopsy (CNB) and Mammotome vacuum-assisted stereotactic biopsy. FNA and CNB can be performed with the assistance of imaging guidance (namely ultrasound) or done “free-hand” in the case of palpable breast lesions. Vacuum-assisted biopsy is performed with sonography, mammography, or MRI assistance.[1][2][3][4] Controversy exists regarding which is the preferred method for diagnosing, as each has strengths and weaknesses, and their incorporation into the breast surgeon’s practice varies. FNA has many advantages and potential uses making it a popular option for the diagnosis and treatment of certain breast lesions.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The breasts of an adult female are located on the anterior portion of the chest wall and play a vital role in milk production. The breast tissue lies on the pectoralis major muscle and is supported by many ligaments that arise from either side of the sternum. Each breast consists of 20 lobes that are dispersed evenly below the nipple. Surrounding each lobe is fatty tissue that gives the breast its shape and size. Each of the lobes consists of numerous lobules which produce milk in response to prolactin and the female sex hormones. The female breast can develop cystic and solid lesions in the lobes. In general, the majority of cystic lesions are benign, and the majority of solid lesions are malignant. Breast cysts tend to develop at the terminal end of the ducts and accumulate fluid.[5]Most breast cysts are small ranging in diameter from 5 mm to 20 mm and may fluctuate in size over the course of the menstrual cycle. A female may develop one or multiple cysts. Most of these cysts are painless, but some women may have discomfort or discover them during palpation of the breast.
Breast cysts are strongly influenced by hormones and are most common in women of childbearing age. Because of the concern of malignancy, women often seek medical attention. [6][7] While a breast cyst may be palpable, sometimes it can be confused with a solid mass. Hence, one of the first approaches to management is a fine needle aspiration biopsy. Some physicians will even order an ultrasound before the FNA to determine the depth, number, and location of the cyst or cysts.
Indications
Diagnosis
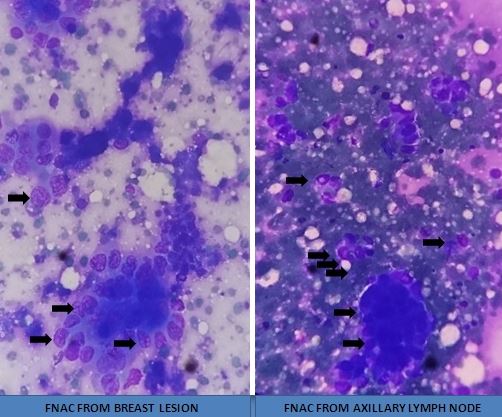
FNA is indicated for patients with a mammographic abnormality or palpable breast lesions. FNA remains controversial for the diagnosis of suspected malignant lesions due to the relatively small amount of breast tissue that is sampled and the high rate of non-diagnostic or inadequate samples. In this case, the “triple test” is performed using a combination of the physical exam, imaging studies and cytology to make this diagnosis to increase diagnostic accuracy. Though the Z0011 study is changing the treatment of axillary disease, axillary ultrasound with FNA sampling of suspicious appearing nodes is advisable.[8][9]
Therapeutic
FNA is indicated for breast cysts that are large, symptomatic, display vegetations, or imaging abnormalities.[10]
Contraindications
FNA should not be done in the following situations:
- Presence of a skin infection
- Patient is on anticoagulant therapy
- Patient has a bleeding disorder
- Patient does not give consent
- Presence of a coagulopathy
- The lesion is deep and not palpable
Equipment
The technique uses alcohol swabs, povidone-iodine solution, sterile gloves, and drapes, a 21 gauge needle with a semiopaque needle hub and a 3 ml or 5 ml syringe. A plastic bandage with soft gauze is needed to close the hole. The use of local anesthesia is not necessary unless the patient is anxious. However, if the lesion is deep and one is going to make multiple attempts, 1% lidocaine should be infiltrated in the skin area.
Preparation
Fine needle aspiration can be done in a clinic or operating room. The procedure should be done in a strict sterile manner. The area of the breast should be prepped and draped in a sterile fashion. The performer should use sterile equipment including gloves.
Technique or Treatment
FNA is performed percutaneously using a small needle (usually a 21 to 25 gauge). The skin is prepared with alcohol, chlorhexidine, or betadine then numbed with a local anesthetic. The mass is localized by palpation or by ultrasound guidance. The mass in question is punctured while negative pressure is created and maintained in the syringe (increasing diagnostic yield). Multiple passes of the needle are made through solid lesions. The puncture is repeated with slightly different needle trajectories to sample different territories. If the lesion is cystic, the liquid is aspirated fully. Then the samples are sent for evaluation in pathology. The area around the puncture site is check for evidence of bleeding or hematoma.
Complications
Even though FNA appears to be a simple procedure, a number of complications can occur which include the following:
- Bruising
- Hematoma
- Infection
- Pneumothorax if the needle is advanced deep in the chest area
- Pain
So far there is no evidence to show that FNA causes seeding of breast cancer or worsens survival or prognosis. More important, FNA does not affect the number of falsely positive mammograms as long as the radiologist has prior information of where the FNA was performed.
Clinical Significance
Advantages of FNA over other Modalities
- Cost-effective (declines with inconclusive results/need for repeat biopsies)
- Less invasive/less painful secondary to smaller needle size
- Can be performed in the clinic or office
- Appropriate for patients who are being anticoagulated with low risk of hematoma/bleeding
- Can be used to sample axillary tissue
Disadvantages
Lower diagnostic yield than core needle biopsy
- Four percent to 13% of samples found to be inadequate or nondiagnostic
- More difficult to distinguish invasive versus in-situ carcinoma
- May require more experienced cytopathologist for diagnosis
- Non-diagnostic results necessitate repeat biopsy (typically CNB or vacuum-assisted)
Accuracy
Certain studies have cited the sensitivity of aspiration cytology for malignancy at 64% for one aspiration sample and 91% in patients with three samples. Specificity was 56% (inadequate or unsatisfactory cytological preparations.
Follow-up
If the FNA reveals a non-bloody aspirate and the cyst resolves, no more follow up is required. Some physicians do follow up with an ultrasound to ensure that the cyst has completely resolved. Re-evaluation is usually done 4 to 6 weeks later.
If the cyst persists after aspiration or contains bloody fluid, the patient should be referred to a surgeon for a formal biopsy.
Conservative management is recommended for patients in whom the clinical, sonography findings and aspiration features are pertinent with the diagnosis of galactocele. Therefore, repeated aspiration or surgical management excision is only indicated if the galactocele is bothersome to the mother. Characteristic features of a mass that is hypoechoic, compressable, wider more than tall, with thin echogenic walls, heterogeneous contents with fluid clefts, and without any solid components, are pertinent with galactocele. Fine-needle aspirations usually reveal a thick, creamy material with a dark green tinge.[11]
Enhancing Healthcare Team Outcomes
FNA is a very common procedure done by the primary care provider, nurse practitioner, internist, radiologist, surgeon, and many others. The key is to know the anatomy and potential complications. It is also important to know that FNA has a low yield and thus a negative result should never be accepted if there is high suspicion of something more sinister. In such scenarios, it is important to communicate with other professionals on the best workup of the patient.[12]
Performing a FNA requires an interprofessional approach. The nurse should be familiar with the procedure, preparation, and technique and should support the surgeon during the procedure making sure that sterile technique is maintained. Often surgeon may need assistance with positioning the patient or anatomical position of the breast for the procedure. In addition, films need to be available and often will require the nurse to assist in holding them during the procedure in locating the mass. After the procedure, the nurse must monitor the patient's vital signs and report back to the surgeon if any untoward complications develop. Further, on discharge, the nurse should provide instructions to the patient and if it is unclear the patient is not understanding the followup, the nurse should consult the surgeon to assist in educating the patient. The patient should be monitored by the nurse for signs of infection post-procedure and again the surgeon contacted if there are concerns. Only through an interprofessional approach to this procedure will optimal outcomes be achieved. [Level V]
Nursing, Allied Health, and Interprofessional Team Monitoring
- Vital signs
- Wound checks
- Signs of infection
- Signs or symptoms of an allergic reaction to medications used pre and postoperatively
Any signs of untoward events should be reported to the surgeon and interprofessional team.
Media
(Click Image to Enlarge)
References
Yii N,Read T,Tan CC,Ng SL,Bennett I, Diagnosing phyllodes tumours of the breast: how successful are our current preoperative assessment modalities? ANZ journal of surgery. 2018 Oct; [PubMed PMID: 30141271]
Brennan SB,D'Alessio D,Kaplan J,Edelweiss M,Heerdt AS,Morris EA, Positive predictive value of biopsy of palpable masses following mastectomy. The breast journal. 2018 Sep; [PubMed PMID: 30033648]
Jairajpuri ZS,Jetley S,Rana S,Khetrapal S,Khan S,Hassan MJ, Diagnostic challenges of tubercular lesions of breast. Journal of laboratory physicians. 2018 Apr-Jun; [PubMed PMID: 29692584]
Mišković J,Zorić A,Radić Mišković H,Šoljić V, Diagnostic Value of Fine Needle Aspiration Cytology for Breast Tumors Acta clinica Croatica. 2016 Dec; [PubMed PMID: 29117654]
Ibikunle DE,Omotayo JA,Ariyibi OO, Fine needle aspiration cytology of breast lumps with histopathologic correlation in Owo, Ondo State, Nigeria: a five-year review. Ghana medical journal. 2017 Mar; [PubMed PMID: 28959065]
Shirian S,Daneshbod Y,Haghpanah S,Khademi B,Noorbakhsh F,Ghaemi A,Mosayebi Z, Spectrum of pediatric tumors diagnosed by fine-needle aspiration cytology. Medicine. 2017 Feb; [PubMed PMID: 28178123]
Giamanco NM,Jee YH,Wellstein A,Shriver CD,Summers TA,Baron J, Midkine and pleiotrophin concentrations in needle biopsies of breast and lung masses. Cancer biomarkers : section A of Disease markers. 2017 Sep 7; [PubMed PMID: 28946562]
Ahmadinejad M,Hajimaghsoudi L,Pouryaghobi SM,Ahmadinejad I,Ahmadi K, Diagnostic Value of Fine-Needle Aspiration Biopsies and Pathologic Methods for Benign and Malignant Breast Masses and Axillary Node Assessment Asian Pacific journal of cancer prevention : APJCP. 2017 Feb 1; [PubMed PMID: 28345843]
Ferré R,Omeroglu A,Mesurolle B, Sonographic Appearance of Lesions Diagnosed as Lobular Neoplasia at Sonographically Guided Biopsies. AJR. American journal of roentgenology. 2017 Mar; [PubMed PMID: 28075608]
Delaloge S,Bonastre J,Borget I,Garbay JR,Fontenay R,Boinon D,Saghatchian M,Mathieu MC,Mazouni C,Rivera S,Uzan C,André F,Dromain C,Boyer B,Pistilli B,Azoulay S,Rimareix F,Bayou el-H,Sarfati B,Caron H,Ghouadni A,Leymarie N,Canale S,Mons M,Arfi-Rouche J,Arnedos M,Suciu V,Vielh P,Balleyguier C, The challenge of rapid diagnosis in oncology: Diagnostic accuracy and cost analysis of a large-scale one-stop breast clinic. European journal of cancer (Oxford, England : 1990). 2016 Oct; [PubMed PMID: 27569041]
Parker S,Saettele M,Morgan M,Stein M,Winkler N, Spectrum of Pregnancy- and Lactation-related Benign Breast Findings. Current problems in diagnostic radiology. 2017 Nov - Dec; [PubMed PMID: 28189388]
Kanchanabat B,Kanchanapitak P,Thanapongsathorn W,Manomaiphiboon A, Fine-needle aspiration cytology for diagnosis and management of palpable breast mass. The Australian and New Zealand journal of surgery. 2000 Nov; [PubMed PMID: 11147439]