Introduction
Bennett fracture is the most common fracture involving the base of the thumb. This fracture refers to an intraarticular fracture that separates the palmar ulnar aspect of the first metacarpal base from the remaining first metacarpal.[1] The injury is typically caused by axial loading on a partially flexed metacarpal and may be associated with other carpal bone fractures or ligament injuries.[2] Radiographs are essential in the evaluation of these injuries and in helping to plan a surgical approach for reduction, as these fractures are considered unstable. The surgical treatment is varied for these fractures. It may consist of closed reduction with percutaneous pinning or open reduction with either pins or inter-fragment pinning. If there is a good alignment of the fracture fragments at postsurgical fixation, clinical outcomes are generally good.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
This fracture is due to an axial load that occurs on a partially flexed metacarpal and may be associated with fractures involving the adjacent carpal bone (trapezium) and/or associated ulnar collateral ligament injuries of the thumb metacarpophalangeal (MCP) joint.[2]
Epidemiology
Bennet fracture is a subtype of fractures involving the thumb. Total fractures that involve the thumb have been found to occur most commonly in children and the elderly. In children between ages of infant to 16 years, 22% of all tubular bone fractures involved the first ray; whereas in patients older than 65 years, 20% of hand fractures occurred in the thumb. In the elderly population, the thumb was the most common tubular bone fractured with the fracture pattern tending to be oblique and intraarticular.[3]
Pathophysiology
The fracture pattern is distinct. The base of the first metacarpal is fractured with intraarticular extension due to the palmar ulnar fragment of the first metacarpal held in place by its ligamentous attachment to the trapezium (known as the anterior oblique ligament) during the axial loading with the rest of the metacarpal moving in the opposite direction and the main fracture line occurring along this point of weakness.[4] Due to this fracture, the first metacarpal shaft subluxes dorsally, proximally, and radially due to the pull of the abductor pollicis longus, extensor pollicis longus, extensor pollicis brevis, and the adductor pollicus brevis, which remain attached to the fracture fragment.
History and Physical
The findings include pain and swelling localized to the base of the thumb.
Evaluation
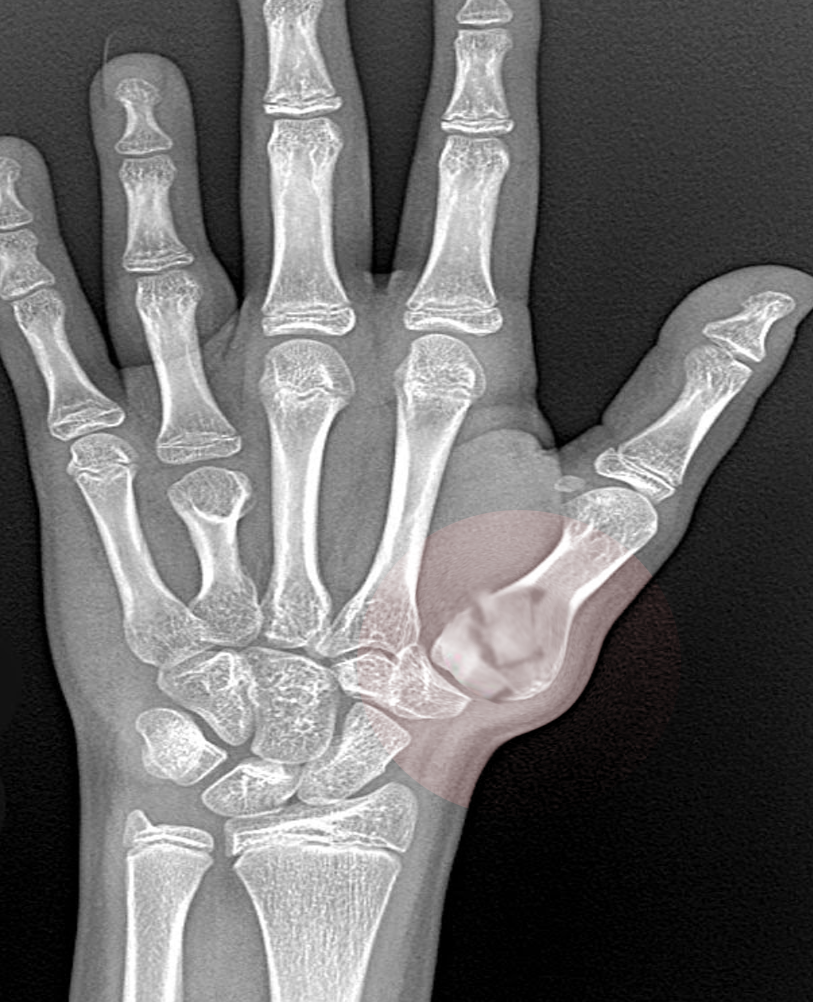
Standard hand radiographs include anteroposterior (AP), lateral, and oblique views. Additional dedicated views of the thumb can be obtained to provide additional information about the injury, including Robert's view.[4] This view is a true AP view of the first carpal-metacarpal joint; it is performed with hyperpronation of the forearm having the dorsal aspect of the thumb placed against the radiographic plate and the x-ray beam directed 90 degrees to the plate. Another view is the Bett's view[4], which is obtained with the palm overpronated 20 degrees from flat against the radiograph plate and the beam directed 15 degrees proximal to distal. Stress radiographs can also be performed by pressing the radial aspect of the thumbs together on an AP view, which may demonstrate subluxation of the metacarpal base radially relative to the trapezium on the symptomatic side.
Based upon the radiographic appearance, Gredda classified Bennett fractures into three types, with type 1 being a fracture with a single ulnar fragment and subluxation of the metacarpal base, type 2 an impaction fracture without subluxation of the first metacarpal, and type 3 an injury with a small ulnar avulsion fragment in association with metacarpal dislocation.[5]
Treatment / Management
Proper reduction requires traction in an axial direction with palmar abduction, and pronation while applying external pressure over the first metacarpal base.[4] Thumb extension (known as the hitchhiker position) has been shown to cause fracture displacement and should be avoided.[1]
In the initial article by Bennett, he described the treatment of these fractures with closed reduction and splinting, which remained the preferred method of treatment until the 1970s.[6][7] Historical reports have shown good outcomes with this treatment, although more recent studies have shown poor outcomes when treating these fractures with casting alone.[8] Surgical treatment of Bennett fractures is varied but generally consists of either closed reduction with percutaneous pinning or open reduction with either pins or interfragmentary screws. All methods of fixation have been shown to be effective in case reviews and series. Treating with closed reduction with intermetacarpal fixation from the first to the second metacarpal and/or to the trapezium is usually effective in reducing the first metacarpal shaft subluxation. If it is decided to treat this fracture with open reduction, it is most commonly performed through a Wagner incision.[4] The decision to treat these fractures with either open reduction or closed reduction is still a matter of debate.
There is a debate in the literature regarding the amount of articular step-off at the fracture site that is acceptable in the nonathlete populations. Some authors have found no correlation between the quality of articular reduction and radiographic or subjective outcomes,[9][10] while biomechanical studies have demonstrated that 2 mm of persistent articular surface step-off does not alter the contact pressures at the location of the step off.[11] It is therefore concluded that bony apposition of the fragments within 2 mm and the correction of any joint subluxation will be tolerated without increasing the risk of posttraumatic arthritis. Despite is biomechanical evidence suggesting good outcomes, many clinical studies have suggested that anatomic reduction is preferred.[7]
Differential Diagnosis
Rolando fracture which is a comminuted fracture at the base of the first metacarpal with a maintained volar carpal ligament, preventing displacement of the volar fragment.
Prognosis
The range of motion exercises may begin 5 to 10 days post screw fixation and after four weeks after pinning (after the pins are removed).[12] Long-term outcomes based on the study of Kjaer-Petersen which reviewed 41 Bennett fractures note that based on the quality of the fracture reduction. Eighty-six percent of patients with an anatomic reduction (less than 1 mm step off) had no residual symptoms, where only 46% of patients with good or poor reduction (greater than 1 mm step off) remained asymptomatic.[6]
Definitive treatment algorithms are lacking due to the small number of patients that are encountered with this fracture, lack of long-term imaging follow up, and lack of randomized prospective data.
Pearls and Other Issues
- Despite a relatively simple appearance on radiographs, Bennett fractures are considered unstable.
- In evaluating and treating these fractures positioning the patient with thumb extension (hitchhikers position) should be avoided as this will cause further fracture displacement.
- Favorable long-term outcomes are based upon the degree of anatomic reduction with most patients having less than 1 mm articular surface step off having no residual symptoms.
Enhancing Healthcare Team Outcomes
The management of Bennet fracture is complex and best done with an interprofessional team that includes a hand surgeon or orthopedic surgeon, specialty care nurse, and physical therapist. When the fracture is encountered by the emergency department physician and nurse practitioner, it is important to refer the patient promptly to a hand surgeon. Poorly treated bennet fracture has very high morbidity. Even after adequate treatment, extensive rehabilitation is required. An orthopedic nurse provides patient and family education, assists with referrals, and provides status updates to the team. The outcomes for Bennet fracture are guarded.[13][14] [Level 5]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Edmunds JO. Traumatic dislocations and instability of the trapeziometacarpal joint of the thumb. Hand clinics. 2006 Aug:22(3):365-92 [PubMed PMID: 16843802]
McGuigan FX, Culp RW. Surgical treatment of intra-articular fractures of the trapezium. The Journal of hand surgery. 2002 Jul:27(4):697-703 [PubMed PMID: 12132098]
Level 2 (mid-level) evidenceStanton JS, Dias JJ, Burke FD. Fractures of the tubular bones of the hand. The Journal of hand surgery, European volume. 2007 Dec:32(6):626-36 [PubMed PMID: 17993422]
Level 2 (mid-level) evidenceCarlsen BT, Moran SL. Thumb trauma: Bennett fractures, Rolando fractures, and ulnar collateral ligament injuries. The Journal of hand surgery. 2009 May-Jun:34(5):945-52. doi: 10.1016/j.jhsa.2009.03.017. Epub [PubMed PMID: 19411003]
GEDDA KO. Studies on Bennett's fracture; anatomy, roentgenology, and therapy. Acta chirurgica Scandinavica. Supplementum. 1954:193():1-114 [PubMed PMID: 13188578]
Kjaer-Petersen K, Langhoff O, Andersen K. Bennett's fracture. Journal of hand surgery (Edinburgh, Scotland). 1990 Feb:15(1):58-61 [PubMed PMID: 2307882]
Oosterbos CJ, de Boer HH. Nonoperative treatment of Bennett's fracture: a 13-year follow-up. Journal of orthopaedic trauma. 1995 Feb:9(1):23-7 [PubMed PMID: 7714650]
Timmenga EJ, Blokhuis TJ, Maas M, Raaijmakers EL. Long-term evaluation of Bennett's fracture. A comparison between open and closed reduction. Journal of hand surgery (Edinburgh, Scotland). 1994 Jun:19(3):373-7 [PubMed PMID: 8077832]
Cannon SR, Dowd GS, Williams DH, Scott JM. A long-term study following Bennett's fracture. Journal of hand surgery (Edinburgh, Scotland). 1986 Oct:11(3):426-31 [PubMed PMID: 3794490]
Demir E, Unglaub F, Wittemann M, Germann G, Sauerbier M. [Surgically treated intraarticular fractures of the trapeziometacarpal joint -- a clinical and radiological outcome study]. Der Unfallchirurg. 2006 Jan:109(1):13-21 [PubMed PMID: 16133289]
Cullen JP, Parentis MA, Chinchilli VM, Pellegrini VD Jr. Simulated Bennett fracture treated with closed reduction and percutaneous pinning. A biomechanical analysis of residual incongruity of the joint. The Journal of bone and joint surgery. American volume. 1997 Mar:79(3):413-20 [PubMed PMID: 9070532]
Kadow TR, Fowler JR. Thumb Injuries in Athletes. Hand clinics. 2017 Feb:33(1):161-173. doi: 10.1016/j.hcl.2016.08.008. Epub [PubMed PMID: 27886832]
Hashiguchi H, Iwashita S, Yoneda M, Takai S. Factors influencing outcomes of nonsurgical treatment for baseball players with SLAP lesion. Asia-Pacific journal of sports medicine, arthroscopy, rehabilitation and technology. 2018 Oct:14():6-9. doi: 10.1016/j.asmart.2018.08.001. Epub 2018 Sep 5 [PubMed PMID: 30202738]
Fischborn T, Beckenbauer D, Held M, Daigeler A, Medved F. Analysis of Operative Techniques of Fractures of the First Metacarpal Base. Annals of plastic surgery. 2018 May:80(5):507-514. doi: 10.1097/SAP.0000000000001293. Epub [PubMed PMID: 29319570]