Introduction
The basilar artery is a vital vessel contributing to the posterior cerebral circulation. It is formed at the junction of the pons and medulla by the convergence of the dual vertebral arteries. The vertebral arteries join the basilar artery to form the vertebrobasilar system, which supplies blood to the posterior portion of the circle of Willis. Its crucial purpose is to serve the cerebellum, brainstem, thalamus, occipital, and medial temporal lobes of the brain with oxygen-rich blood. With an average diameter of 3 to 4 millimeters, it furnishes 20 paramedian and circumflex perforating arteries thus providing a robust collateral network to the pons and midbrain. Throughout its course, the basilar artery distributes the median, paramedian, short, and long circumferential branches. It is located on the ventral surface of the neuronal "bridge" also known as the pons (Latin for "bridge") that connects the forebrain to the cerebellum.[1][2] Overall, the basilar artery is one of the most important arteries of the human body.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The cause can occur from thromboembolism, atherosclerotic disease, or vascular dissection. The mechanism differs depending on the affected segment. Atherosclerotic disease more commonly affects the mid-portion of the basilar artery, followed by the vertebrobasilar junction. Lodging of an embolic source is much more frequent in the distal third of the basilar artery especially at the top of the basilar artery and the vertebrobasilar junction. Arterial dissection is more common in the extracranial vertebral artery and has been associated with neck injuries and cervical chiropractic adjustments. Intracranial dissections are exceedingly rare.[1]
Epidemiology
Risk factors are similar to the known general risk factors for stroke. The most common is hypertension which is found in as many as 70% of cases. Other risk factors include diabetes mellitus, coronary artery disease, peripheral vascular disease, cigarette smoking, and hyperlipidemia.
The frequency, incidence, and prevalence are not well known in the medical literature. 20% of cerebral blood flow goes through the posterior circulation (vertebrobasilar system), it is logical to understand why posterior circulation occlusions account for one-fifth of all strokes. Fortunately, basilar artery occlusions are believed to account for approximately only 1% of all strokes. Basilar artery occlusion has been reported in 2 out of 1000 post-mortem cases. Basilar artery thrombosis may explain as many as 27% of ischemic strokes occurring in the posterior circulation. An increased prevalence exists in males, with a 2:1 ratio. Occlusion due to atherosclerotic disease is most prevalent in patients of advanced age, usually in the sixth and seventh decades of life. Distal basilar artery occlusion is usually secondary to embolism and is most prevalent in the fourth decade of life.[3][4][5]
History and Physical
Most commonly, patients experiencing basilar artery occlusion exhibit acute neurologic signs including motor deficits, hemiparesis or quadriparesis, and facial palsies, dizziness, headache, and speech abnormalities–especially dysarthria and difficulty articulating words. Patients may also complain of nausea, vomiting, and changes in vision. An altered level of consciousness is commonly present.
Basilar artery thrombosis may present in three general constellations:
- Rapid onset of advanced motor and bulbar symptoms with a decreased level of consciousness.
- Insidious or stuttering symptoms over a few days as a combination of the above that end with disabling motor and bulbar symptoms, a decreased level of consciousness, or both.
- Prodromal symptoms may include headache, neck pain, loss of vision, binocular diplopia, dysarthria, dizziness, hemiparesis, paresthesias, ataxia, and tonic-clonic type movements. “Herald hemiparesis” is the phrase to describe the momentary, unilateral weakness that may precede later permanent symptoms.
An abnormal level of consciousness and focal motor weakness are the hallmark symptoms manifested in the majority of patients. Pupillary abnormalities, oculomotor signs, and pseudobulbar manifestations (facial palsy, dysphonia, dysarthria, dysphagia) are seen in more than 40% of patients.[1][6][7][8]. Variable degrees of hemiparesis or quadriparesis are part of the clinical picture. As basilar artery thrombosis presents in various ways it is very important to have high clinical suspicion to detect basilar artery thrombosis.
Evaluation
The primary goals of the evaluation are to establish the location of the vascular lesion and determine whether acute intervention is indicated to achieve recanalization in a time-sensitive manner.
Laboratory studies have limited utility but may include a complete blood count (CBC), electrolytes, blood urea nitrogen (BUN) and creatinine, international normalized ratio (INR), prothrombin time (PT), and activated partial thromboplastin time (aPTT). Younger patients or patients without evidence of atherosclerosis should be investigated for the presence of procoagulant conditions. These include protein C, protein S, and antithrombin III deficiencies, lupus anticoagulant and anticardiolipin antibodies, and homocysteine levels. An electrocardiogram helps to screen for arrhythmias that may be suggestive of a thrombotic etiology.
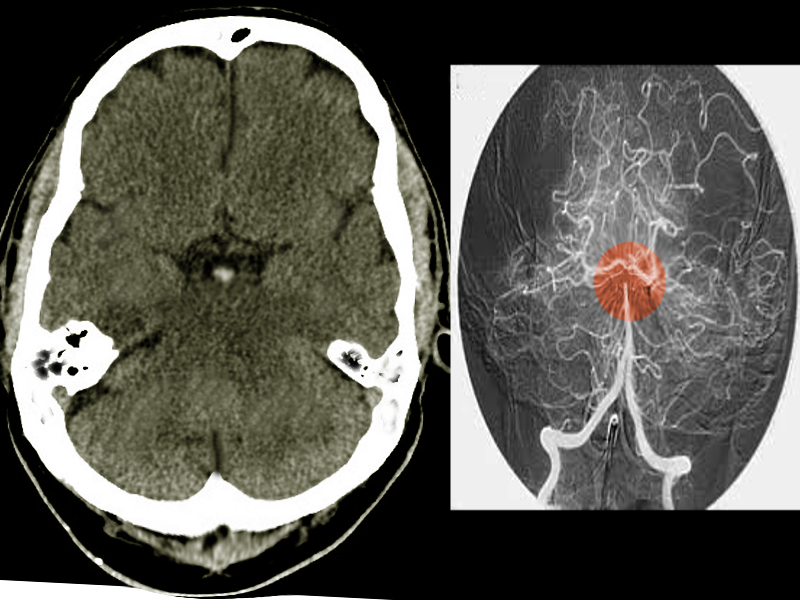
Computed tomography (CT) scanning is usually the first imaging study performed. CT may be effective at identifying larger areas of ischemic insult and can highlight hemorrhagic pathology. A hyperdense basilar artery may be present on the CT scan. However, CT scanning has a low sensitivity for early ischemia and is less effective at evaluating the brainstem, cerebellum, and posterior circulation. Ultimately, one needs a high index of suspicion in the correct clinical context to diagnosis an easily missed disease. Additional evaluation with CT angiography may be considered, and a filling defect noted within the basilar artery. Catheter angiography is still a criterion for diagnosis; however, with the availability of noninvasive imaging modalities such as magnetic resonance imaging (MRI) and angiography (MRA), the role of angiography has changed. MRI/MRA is more sensitive than CT scanning for identifying early ischemia and vascular occlusion.[6][9][10][11][12][13]. MRI is the best imaging modality for any posterior fossa lesion including acute ischemic infarction. DWI MRI sequence can show an acute brainstem or cerebellar infarct within seconds of the arterial occlusion. MR angiogram can show the site of vascular occlusion non-invasively. The presence of microhemorrhages in GRE-T2* or SWI imaging can help to indicate underlying hypertensive etiology.
Treatment / Management
Acute occlusion of the basilar artery is potentially life-threatening. All patients should be admitted to a stroke unit when available. Recanalization of the basilar artery is key to the successful treatment of basilar artery thrombosis and to improving prognosis. This can be accomplished by systemic thrombolysis (IVT), intra-arterial thrombolysis (IAT), or mechanical endovascular thrombectomy. Recanalization occurs in more than half of basilar artery occlusion patients treated with IAT or IVT. Treatment is time-sensitive; the earlier the intervention, the better the functional outcomes. There is no good large-scale study to define the treatment window for basilar thrombosis. It is clearly much longer than the accepted window of 6 to 8 hours recommended for large vessel occlusion in anterior circulation infarct. The commonly accepted time window is at least 12 hours and potentially up to 24 hours. In some situations, if the patient is having symptoms and minimal stroke on the MRI brain it is reasonable to consider for mechanical endovascular thrombectomy up to 2-3 days. Subsequent therapy for secondary prevention focuses on treating the underlying causes and modifying risk factors.[14][15][16][17][18][19](A1)
Differential Diagnosis
When considering the diagnosis, it is important to consider other etiologies that may cause similar overlapping symptoms. These include meningitis, basilar migraine, cerebellar hemorrhage with brainstem compression, cerebellar infarct or hemorrhage with edema, space-occupying lesions in the posterior fossa including metastatic disease, and supratentorial mass lesions with mass effect, herniation, and brainstem compression. Consider hypoglycemia, Todd paralysis, and conversion disorder as possible mimics.[20][21]
Prognosis
The patient mortality rate is greater than 85%, although it drops to as low as 40% in patients with recanalization. One can expect good functional outcomes in as few as 24 to 35% of patients treated with intravenous or intra-arterial thrombolysis. For symptomatic patients who survive, the risk of recurrent stroke is 10 to 15%.[15] The most important prognostic factors are the extent and duration of thrombosis. Therefore, a high index of suspicion of the diagnosis followed by expedited recanalization will give the patient the best hope of an improved outcome.
Complications
Overall outcomes can be expected to be poor in patients with basilar artery thrombosis. Advances in pharmacologic and mechanical thrombosis and endovascular therapy may reduce the subsequent mortality and disability rates. Catheter-directed thrombolysis and IV heparin also carry a risk of hemorrhage. Complications can include the following: aspiration, aspiration pneumonia, thromboembolic disease (deep vein thrombosis and pulmonary embolism), myocardial infarction, and recurrent stroke. Patients with advanced functional debility secondary to stroke are increasingly prone to contractures, pressure ulcers, and sepsis. Many patients who survive basilar artery thrombosis require ongoing physical and occupational therapy to regain and maintain functionality.[15][22]
Enhancing Healthcare Team Outcomes
Managing a patient with acute neurologic symptoms requires timely and coordinated efforts by an interprofessional team. This team might initially include a physician, nurse, pharmacist, and multiple ancillary personnel such as phlebotomists, radiography technicians, and laboratory personnel. A wide array of physician specialists such as neurologists, radiologists, interventional radiologists, internists, cardiologists, and physical medicine and rehabilitation physicians may be involved in the care of a patient with basilar artery thrombosis. With almost any acute ischemic event, not limited to basilar artery thrombosis, studies have shown that the earlier the intervention is undertaken, the better off the patient's functional outcomes might be. With the mantra "Time is of the Essence" in mind, one can recognize that the presence of an integrated multi-functional team is vitally important in providing the rapid stabilization, evaluation, diagnosis, and intervention of patients suffering from acute neurologic conditions.
The coordination of this type of specialty care has made comprehensive stroke centers (CSCs) an increasingly common part of large tertiary healthcare centers. CSCs are designated to provide more complex services, including around-the-clock availability of endovascular procedures. Many questions are worth exploring in the near future: Do CSCs offer any appreciable benefit to ischemic stroke patients? and, if so, what types? Do all patients with an acute stroke need to be referred to a CSC? Medicine looks forward to exploring these questions, and many more as the optimal outline for treating patients with ischemic intracranial pathology and basilar artery thrombosis is better defined and advanced.
Media
References
Nagel S. [Stroke due to acute occlusion of the basilar artery : Diagnosis and treatment]. Medizinische Klinik, Intensivmedizin und Notfallmedizin. 2017 Nov:112(8):679-686. doi: 10.1007/s00063-017-0347-0. Epub 2017 Sep 13 [PubMed PMID: 28905077]
Schulz UG, Fischer U. Posterior circulation cerebrovascular syndromes: diagnosis and management. Journal of neurology, neurosurgery, and psychiatry. 2017 Jan:88(1):45-53. doi: 10.1136/jnnp-2015-311299. Epub 2016 Apr 12 [PubMed PMID: 27071644]
Kjerpeseth LJ, Ellekjær H, Selmer R, Ariansen I, Furu K, Skovlund E. Risk factors for stroke and choice of oral anticoagulant in atrial fibrillation. European journal of clinical pharmacology. 2018 Dec:74(12):1653-1662. doi: 10.1007/s00228-018-2540-3. Epub 2018 Aug 16 [PubMed PMID: 30116828]
Ekker MS, Boot EM, Singhal AB, Tan KS, Debette S, Tuladhar AM, de Leeuw FE. Epidemiology, aetiology, and management of ischaemic stroke in young adults. The Lancet. Neurology. 2018 Sep:17(9):790-801. doi: 10.1016/S1474-4422(18)30233-3. Epub [PubMed PMID: 30129475]
Wang L, He M, Zhang Y. Risk factors associated with extracranial atherosclerosis in old patients with acute ischemic stroke. Scientific reports. 2018 Aug 22:8(1):12541. doi: 10.1038/s41598-018-31026-z. Epub 2018 Aug 22 [PubMed PMID: 30135472]
Ausman JI, Liebeskind DS, Gonzalez N, Saver J, Martin N, Villablanca JP, Vespa P, Duckwiler G, Jahan R, Niu T, Salamon N, Yoo B, Tateshima S, Buitrago Blanco MM, Starkman S. A review of the diagnosis and management of vertebral basilar (posterior) circulation disease. Surgical neurology international. 2018:9():106. doi: 10.4103/sni.sni_373_17. Epub 2018 May 24 [PubMed PMID: 29930872]
McDermott M, Jacobs T, Morgenstern L. Critical care in acute ischemic stroke. Handbook of clinical neurology. 2017:140():153-176. doi: 10.1016/B978-0-444-63600-3.00010-6. Epub [PubMed PMID: 28187798]
Johnson TM, Romero CS, Smith AT. Locked-in syndrome responding to thrombolytic therapy. The American journal of emergency medicine. 2018 Oct:36(10):1928.e5-1928.e7. doi: 10.1016/j.ajem.2018.07.003. Epub 2018 Jul 3 [PubMed PMID: 29983216]
Reid M, Famuyide AO, Forkert ND, Sahand Talai A, Evans JW, Sitaram A, Hafeez M, Najm M, Menon BK, Demchuk A, Goyal M, Sah RG, d'Esterre CD, Barber P. Accuracy and Reliability of Multiphase CTA Perfusion for Identifying Ischemic Core. Clinical neuroradiology. 2019 Sep:29(3):543-552. doi: 10.1007/s00062-018-0717-x. Epub 2018 Aug 21 [PubMed PMID: 30132089]
Kadoya Y, Zen K, Oda Y, Matoba S. Successful Endovascular Treatment for Aortic Thrombosis Due to Primary Antiphospholipid Syndrome: A Case Report and Literature Review. Vascular and endovascular surgery. 2019 Jan:53(1):51-57. doi: 10.1177/1538574418791355. Epub 2018 Aug 9 [PubMed PMID: 30092725]
Level 3 (low-level) evidenceSugrue G, O'Reilly MK, Byrne D, Crockett MT, Murphy S, Kavanagh EC. CT cervico-cerebral angiography in acute stroke. Can we justify aortic arch imaging? Irish journal of medical science. 2019 May:188(2):661-666. doi: 10.1007/s11845-018-1888-9. Epub 2018 Aug 24 [PubMed PMID: 30143966]
Campbell BC, Parsons MW. Imaging selection for acute stroke intervention. International journal of stroke : official journal of the International Stroke Society. 2018 Aug:13(6):554-567. doi: 10.1177/1747493018765235. Epub 2018 Mar 15 [PubMed PMID: 29543140]
Safdarian M, Rohani M. Basilar Artery Thrombosis on Brain MRI. The Neurohospitalist. 2018 Jul:8(3):NP3. doi: 10.1177/1941874417733218. Epub 2017 Sep 25 [PubMed PMID: 29977452]
Kheiri B, Osman M, Abdalla A, Haykal T, Ahmed S, Hassan M, Bachuwa G, Al Qasmi M, Bhatt DL. Tenecteplase versus alteplase for management of acute ischemic stroke: a pairwise and network meta-analysis of randomized clinical trials. Journal of thrombosis and thrombolysis. 2018 Nov:46(4):440-450. doi: 10.1007/s11239-018-1721-3. Epub [PubMed PMID: 30117036]
Level 1 (high-level) evidenceChen CJ, Chuang TY, Hansen L, Dutta S, Ding D, Buell TJ, Ironside N, Patibandla MR, Southerland AM, Worrall BB, Kalani MYS. Predictors of 30-day mortality after endovascular mechanical thrombectomy for acute ischemic stroke. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2018 Nov:57():38-42. doi: 10.1016/j.jocn.2018.08.044. Epub 2018 Aug 23 [PubMed PMID: 30145087]
Xiong YJ, Gong JM, Zhang YC, Zhao XL, Xu SB, Pan DJ, Qu WS, Tian DS. Endovascular thrombectomy versus medical treatment for large vessel occlusion stroke with mild symptoms: A meta-analysis. PloS one. 2018:13(8):e0203066. doi: 10.1371/journal.pone.0203066. Epub 2018 Aug 23 [PubMed PMID: 30138460]
Level 1 (high-level) evidenceAronov MS, Popugaev KA, Udalov YD, Samoylov AS. [Endovascular treatment of acute ischemic stroke]. Zhurnal voprosy neirokhirurgii imeni N. N. Burdenko. 2018:82(4):103-108. doi: 10.17116/neiro2018824103. Epub [PubMed PMID: 30137044]
Moussaddy A, Demchuk AM, Hill MD. Thrombolytic therapies for ischemic stroke: Triumphs and future challenges. Neuropharmacology. 2018 May 15:134(Pt B):272-279. doi: 10.1016/j.neuropharm.2017.11.010. Epub 2018 Mar 3 [PubMed PMID: 29505787]
Ritvonen J, Strbian D, Silvennoinen H, Virtanen P, Salonen O, Lindsberg PJ, Sairanen T. Thrombolysis and adjunct anticoagulation in patients with acute basilar artery occlusion. European journal of neurology. 2019 Jan:26(1):128-135. doi: 10.1111/ene.13781. Epub 2018 Sep 12 [PubMed PMID: 30134080]
Neves Briard J, Zewude RT, Kate MP, Rowe BH, Buck B, Butcher K, Gioia LC. Stroke Mimics Transported by Emergency Medical Services to a Comprehensive Stroke Center: The Magnitude of the Problem. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association. 2018 Oct:27(10):2738-2745. doi: 10.1016/j.jstrokecerebrovasdis.2018.05.046. Epub 2018 Jul 26 [PubMed PMID: 30056002]
Okano Y, Ishimatsu K, Kato Y, Yamaga J, Kuwahara K, Okumoto K, Wada K. Clinical features of stroke mimics in the emergency department. Acute medicine & surgery. 2018 Jul:5(3):241-248. doi: 10.1002/ams2.338. Epub 2018 Apr 10 [PubMed PMID: 29988676]
Chatterjee SA, Daly JJ, Porges EC, Fox EJ, Rose DK, McGuirk TE, Otzel DM, Butera KA, Clark DJ. Mobility Function and Recovery After Stroke: Preliminary Insights From Sympathetic Nervous System Activity. Journal of neurologic physical therapy : JNPT. 2018 Oct:42(4):224-232. doi: 10.1097/NPT.0000000000000238. Epub [PubMed PMID: 30138228]