Introduction
The atlantoaxial joint is a type of synovial joint that is classified as a uniaxial pivot joint. This joint resides in the upper part of the neck between the first and second cervical vertebrae, also known as the atlas and axis, respectively. The pivot joint classification means that it allows for rotation only and is formed by a central pivoting, bony structure that rotates around craniovertebral ligaments.[1]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
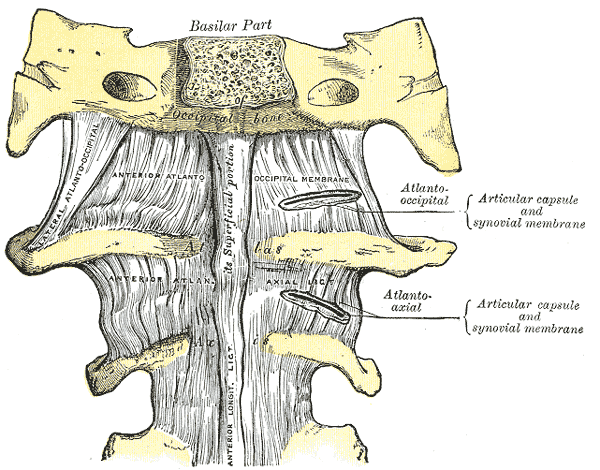
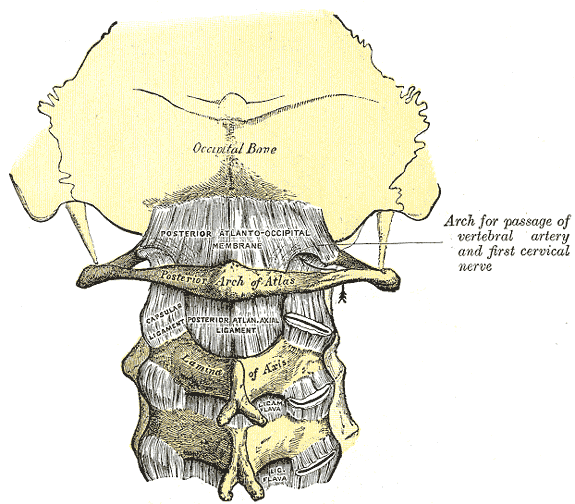
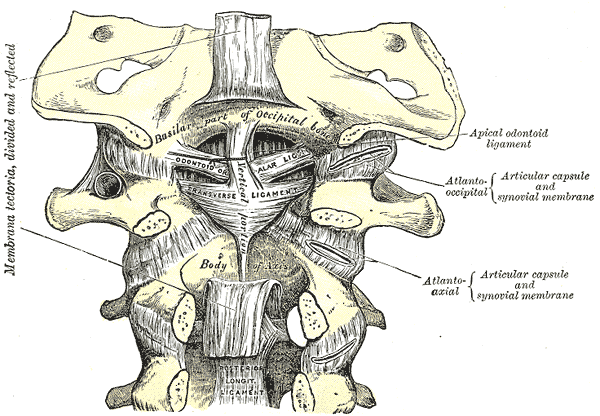
The atlantoaxial joint is a unique joint with multiple distinct structural aspects contributing to its crucial function for cervical stability and mobilization. It consists of three distinct synovial joints: one medial joint and two lateral atlantoaxial joints. The median atlantoaxial joint's structure is formed by the dens of C1 vertebrae and two ligamentous structures anteriorly and posteriorly.[1] These structures are the osteoligamentous rings of the atlas and the transverse ligament, respectively. The two bilateral atlantoaxial joints found laterally are classified as gliding joints. The uppermost parts of the cervical spine that make up the atlantoaxial joint are the atlas (C1) and the axis (C2). As they reside in the craniovertebral junction at the convergence of the skull and the cervical spine, these two vertebrae are unique among the rest of the cervical spine due to their specific anatomical structure. This joint is unique among the rest of the cervical spine due to its lack of an intervertebral disk.
The multipurpose function of the atlantoaxial joint is crucial in practical applications, allowing the head to rotate and turn to the left or right. Without the atlantoaxial joint, the kinematic capability of the head and neck would not allow for the nearly 600 movements per hour that we make as humans.[2] The function of this joint in the cervical spine is multifaceted. In general, it stabilizes the head and supports the weight in a neutral position. This cervical unit also facilitated a protective aspect of the spinal cord from external compression. It also allows for blood supply to the brain through the passage of the vertebral artery. In addition to the protection and stabilization of the head, neck, and internal structures, the atlantoaxial joint also facilitates head-neck movements along with the neck muscles. The atlantoaxial joint is also surrounded by an articular capsule, which functions to connect the margins of the atlas at the lateral masses with the posterior surface of the axis.
Atlas (C1)
The atlas is a circular shape that articulates with the cranium above it with the zygapophyseal joints or lateral masses. Below, the atlas articulates with the axis through its bilateral condyles.[2] The atlas also lacks a spinous process or vertebral body, which distinguishes its structure from the rest of the cervical vertebrae. The atlas also contains the transverse ligament between two superior articular facets, an anterior arch and a posterior arch, which acts as a groove for the vertebral artery.
Axis (C2)
This vertebra is the C2 vertebra and possesses a characteristic feature called the dens or odontoid process. This structure is on the vertebrae's anterior portion and extends superiorly, articulating with the axis above. Other features of the axis are the superior articular facets, bifid spinous process, and bilateral transverse foramina.[2]
Embryology
During gestation and the first two weeks following fertilization, several cellular divisions occur, leading to blastocyst formation. At the end of the second week, the blastocyte undergoes a process called gastrulation, which involves formation into a stratified structure composed of the ectoderm, mesoderm, and endoderm. In the formation of the cervical spine and atlantoaxial joint, mesodermal structures called somites begin to migrate into their mature, functional form as vertebrae.
As the notochord involutes and somites evolve into their mature forms as vertebrae at primary ossification centers. The normal development of the cervical spine in embryogenesis includes the following steps: gastrulation and somatic mesodermal formation, condensation of mesoderm into somites, dermomyotome and sclerotome reorganization, segmentation of somites, chondrification and ossification of the vertebrae. The axis contains one ossification center for the vertebral body, two for both neural arches, and one for the dens.
These ossification centers of the dens are particularly important since they can be confused as fractures in pediatric patients since the junction between the dens and body of the axis does not complete fusion until about six years of age. The body of the axis and the odontoid process are known to fuse by 4 to 6 years of age and complete development by age 25.[3]
Blood Supply and Lymphatics
The vertebral arteries are by far the most important in the contextual location of the head and neck. The atlantoaxial joint as a whole receives blood supply from surrounding branches of the deep cervical, occipital, and vertebral arteries. In relation to the atlantoaxial joint, the vertebral arteries exit the axis transverse foramen, then course slightly laterally to the transverse foramen of the atlas as they enter the cranium.[4]
The collateral branches of the vertebral arteries supply the vertebral bodies of the cervical spine and the cervical radicular arteries. Arising from the subclavian arteries, the vertebral arteries travel cephalad bilaterally; they converge together to form a single structure called the basilar artery, which directly supplies the brainstem.[5]
Nerves
The innervation of the atlantoaxial joint is primarily by the branches of the second cervical spinal nerve. In general, each cervical vertebrae has two nerve roots that arise from the spinal cord and extend out from each side. The ventral segment of the vertebrae contains the ventral root, and the dorsal segment of the vertebrae contains the dorsal root. As the nerve roots converge together in the spinal foramen, they are termed spinal nerves. Although there are seven cervical vertebrae, eight pairs of spinal nerves exist. Usually, the spinal nerves exit above each corresponding vertebrae. However, the C8 nerve root exits below the C7 vertebrae.[6]
Muscles
Since the most mobile portion of the cervical spine is the atlantoaxial joint, the main stabilization sources are the two major surrounding and stabilizing ligaments: the transverse ligament and the alar ligament. Several muscles in the posterior neck and suboccipital triangle act to stabilize the cervical vertebrae and joints as they enable rotatory, extension/flexion, and side-bending. The suboccipital muscle group, which includes the posterior occipital triangle muscles, acts as attachments, postural stabilizers, and craniocervical movement initiators. They also prevent posterior shifting of the occiput on C1. These four muscles include the rectus capitis posterior major and minor and the obliquus capitis superior and inferior.
The craniovertebral ligaments that play a role in the stability of the atlantoaxial joint are the following:
- Cruciform ligament (transverse ligament of the atlas)
- Tectorial membrane
- Alar ligaments
- Apical ligament of dens
Physiologic Variants
In general, in between cervical vertebrae, there lies an intervertebral disc that is not present between C1 and C2 of the atlantoaxial joint. Additionally, a bifid spinous process is only consistently seen in C2-C4. The literature accounts for roughly 0.3% of the population possess a bifid spinous process as low as C7. These are examples of normal physiologic variation. However, the odontoid process and even the transverse ligament can potentially undergo incomplete formation leading to an anatomical variant and potential harmful predisposition to instability and injury.[3]
Os odontoideum - a controversial congenital or traumatic variation of the dens where the superior margin of a hypoplastic den contains an ossific density. It is usually seen in the early development of the spine, as in children, and can be classified as orthotopic or dystopic.[7][8]
Persistent ossiculum terminal - this congenital malformation refers to the secondary ossification centers that fail to fuse on the superior edge of the dens. This malformation is most of the time stable but can be found incidentally. Ossification variation describes any arrest or partial interruption of bony ossification that may pose an obstacle to the anatomical structure and physiologic functional capabilities of the atlantoaxial joint. These disruptions can lead to significant cervical vertebrae anomalies due to growth plate dysfunction.[9]
Surgical Considerations
External Reduction Fixation
Surgical repair of the odontoid process, or dens, fractures is often an immediate necessity. Type I fractures are extremely rare and are usually stable, not needing any surgical fixation. Type II fractures, however, are unstable and need stabilization either by external fixation education and immobilization or internal fixation. Without surgical stabilization, there is a potential risk of nonunion with non-surgical intervention. There are certain nonunion risk factors to consider before opting out of surgery. These include but are not limited to age greater than 50 years old at the time of injury, displacement of the dens is greater than 6 mm, and if moderate fracture comminution is present. It is shown that with an anterior approach to fixation, there are higher success rates of surgical repair.[10][11]
Halo Immobilization
This nonsurgical approach carries a lesser risk of nonunion if the patient is younger than 50 years of age at injury, has minimal dens displacement, and has no comminution. This technique can be achieved using a halo vest immobilizer (HVI), which functions to provide an extremely rigid external support for the immobilization of the upper cervical spine, including the atlantoaxial joint. It restricts C1-C2 joint flexion by 75%.[12]
Clinical Significance
Atlantoaxial Dislocation/Subluxation
Most of the time, atlantoaxial dislocation or dissociation (AOD) is due to high-energy trauma such as motor vehicle accidents. These injuries are affiliated with high mortality rates due to proximity to the brainstem and potential vascular structures. There are three types of AOD, and all three are believed to all share the same mechanism of injury of extreme hyperextension followed by lateral flexion. It is important to note that the method for detecting an AOD on imaging is to look for the basion-dens distance. If greater than 10 mm, this is highly likely of an atlantoaxial dissociation.[13]
Type I - Ventral Dislocation
- Most common
- Ventral dislocation of the occiput
Type II - Longitudinal Distraction
- Most unstable
Type II - Dorsal Dislocation[13]
Nontraumative Subluxation
Certain disease states carry an increased incidence of atlantoaxial joint instability. This is primarily due to ligamentous laxity, which carries a higher risk for subluxation. Some of these conditions include spontaneous hyperemic dislocation, nasopharyngeal torticollis, also known as Grisel syndrome, rheumatoid arthritis, trisomy 21, Morquio syndrome, and Marfan syndrome.[14][15] Other congenital syndromes can cause anatomical variants of the atlantoaxial joint, such as incomplete odontoid process formation or underdeveloped transverse ligament.
Traumatic Rotatory Subluxation
Age-related bony architecture plays a role in tendencies for trauma. In elderly populations, there is more pronounced bony degeneration and decreased bone density, which also leads to cartilaginous loss. This may account for a thinner joint space and predispose the patient to endure a life-threatening injury if they sustain an atlantoaxial distraction or subluxation. Also, children tend to have a higher likelihood of having hypermobility in their joints and ligaments. Therefore, traumatic rotational subluxation due to hyperflexion and rotational forces may be seen more often in pediatric populations.[16]
Fractures of the Atlas with Subsequent Transverse Ligament Rupture
Jefferson fracture is the name given to describe an atlas fracture. When the weakest portion of the vertebral body is impacted with intense axial loading, the anterior and posterior arches are usually affected. This type of fracture is often seen when a patient has a history of diving headfirst into shallow water. Specific subtypes of the atlas due to high-intensity axial loading can be classified into 3 subtypes: posterior arch, burst, and lateral mass injuries. Sometimes, the transverse and alar ligaments may be torn without fracture to the atlas. These injuries are best evaluated by computed tomography and magnetic resonance imaging (MRI).[10][17]
Dens Fractures[3]
- Type I - avulsion fracture of the odontoid tip at the alar ligament insertion site
- Type II - a fracture at the base of the odontoid process
- Type III - a fracture that extends into the axis body
Cervicogenic Headache
This is a subtype of chronic headache, which is likely a secondary headache stemming from pathology in the upper cervical joints or the atlantooccipital joint. With ipsilateral, pericranial muscle pain being the main symptom of a cervicogenic headache, the C1-C3 nerve roots are thought to be a nociceptive origin for referred pain up to the occiput. It is important to distinguish a cervicogenic headache from other headache subtypes and more ominous pathology, such as cervical artery dysfunction, intracranial pathology, and cervical myelopathy.[18][19]
Occipital Neuralgia
The posterior cervical plexus, also known as Cruveilhier’s plexus, can be entrapped by a collection of muscle fibers. As the nerve fibers from the posterior rami of C1-C3 exit, hypertonic suboccipital muscles and even the superficial muscles, such as the trapezius and splenius capitis, can compress and ensnare the surrounding nerve structures. Hypertonic muscles can subsequently inhibit the functions of the nerve fibers leading to inflammation, injury, and severe piercing or throbbing-like sensation in the upper heck and occiput. This condition is known as occipital neuralgia.[20]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
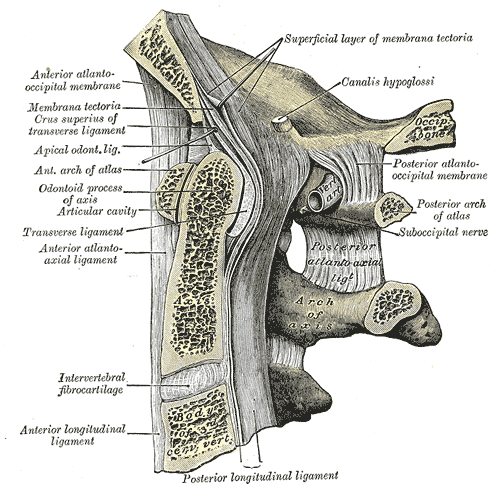
Cervical Region of Spine Anatomy. Anatomy includes median sagittal section, occipital bone, first three cervical vertebrae, superficial layer of membrana tectoria, calais hypoglossi, anterior atlantooccipital membrane, spine, membrana tectoria, crus superius, transverse ligament, apical odontoid ligament, anterior arch of atlas, odontoid process, odontoid, anterior atlantoaxial ligament, intervertebral fibrocartilage, anterior longitudinal ligament, axis.
Gray's Anatomy
References
Juneja P, Munjal A, Hubbard JB. Anatomy, Joints. StatPearls. 2024 Jan:(): [PubMed PMID: 29939670]
Bland JH, Boushey DR. Anatomy and physiology of the cervical spine. Seminars in arthritis and rheumatism. 1990 Aug:20(1):1-20 [PubMed PMID: 2218549]
O'Brien WT Sr, Shen P, Lee P. The Dens: Normal Development, Developmental Variants and Anomalies, and Traumatic Injuries. Journal of clinical imaging science. 2015:5():38. doi: 10.4103/2156-7514.159565. Epub 2015 Jun 30 [PubMed PMID: 26199787]
Al-Habib A, Albadr F, Ahmed J, Aleissa A, Al Towim A. Quantitative assessment of vertebral artery anatomy in relation to cervical pedicles: surgical considerations based on regional differences. Neurosciences (Riyadh, Saudi Arabia). 2018 Apr:23(2):104-110. doi: 10.17712/nsj.2018.2.20170448. Epub [PubMed PMID: 29664450]
Elgueta MF, Ortiz Jimenez J, Wang NN, Pérez Lara A, Chankowsky J, Charghi R, Tran DQ, Finlayson RJ. Anatomical Variations of the Vertebral Artery in the Upper Cervical Spine: Clinical Relevance for Procedures Targeting the C1/C2 and C2/C3 Joints. Regional anesthesia and pain medicine. 2018 May:43(4):367-371. doi: 10.1097/AAP.0000000000000734. Epub [PubMed PMID: 29346229]
AydoĞmuŞ E, Çavdar S. Morphometric Study of the Cervical Spinal Canal Content and the Vertebral Artery. International journal of spine surgery. 2020 Aug:14(4):455-461. doi: 10.14444/7060. Epub 2020 Jul 31 [PubMed PMID: 32986564]
Sardi JP, Iwanaga J, Oskouian RJ, Tubbs RS. First Gross Anatomic Findings of an Os Odontoideum. World neurosurgery. 2017 May:101():813.e1-813.e3. doi: 10.1016/j.wneu.2017.03.066. Epub 2017 Mar 23 [PubMed PMID: 28344179]
Zhang LM, Xu Y, Zhu JY. [Traction for the treatment of traumatic atlantoaxial subluxation in adults]. Zhongguo gu shang = China journal of orthopaedics and traumatology. 2020 Sep 25:33(9):883-6. doi: 10.12200/j.issn.1003-0034.2020.09.018. Epub [PubMed PMID: 32959580]
Strohm PC, Müller CA, Bley TA, Köstler W, Südkamp NP. [Ossiculum terminale (Bergmann). Differential diagnosis of an odontoid fracture of the Anderson I type]. Der Unfallchirurg. 2003 Dec:106(12):1054-6 [PubMed PMID: 14727042]
Level 3 (low-level) evidenceZou X, Ouyang B, Wang B, Yang H, Ge S, Chen Y, Ni L, Zhang S, Xia H, Wu Z, Ma X. Motion-preserving treatment of unstable atlas fracture: transoral anterior C1-ring osteosynthesis using a laminoplasty plate. BMC musculoskeletal disorders. 2020 Aug 12:21(1):538. doi: 10.1186/s12891-020-03575-w. Epub 2020 Aug 12 [PubMed PMID: 32787814]
Das S, Palaniandy K, Abu Bakar A, Idris Z, Abdullah JM. Rare and Unique Case of Midline Anterior Arch of Atlas Non-formation Mimicking Jefferson Type 1 Fracture. Cureus. 2020 Feb 3:12(2):e6850. doi: 10.7759/cureus.6850. Epub 2020 Feb 3 [PubMed PMID: 32181085]
Level 3 (low-level) evidenceKoutsogiannis P, Weisbrod LJ, Dowling TJ. Halo Brace. StatPearls. 2024 Jan:(): [PubMed PMID: 32491478]
Mingsheng T, Long G, Ping Y, Feng Y, Xiangsheng T, Haoning M, Qinying H. New Classification and Its Value Evaluation for Atlantoaxial Dislocation. Orthopaedic surgery. 2020 Aug:12(4):1199-1204. doi: 10.1111/os.12734. Epub 2020 Jul 25 [PubMed PMID: 32710601]
Level 2 (mid-level) evidenceLisitskiy IY, Kiselev AM, Kiselev SE. [Rheumatoid atlanto-axial dislocation: a surgical approach]. Zhurnal voprosy neirokhirurgii imeni N. N. Burdenko. 2018:82(1):41-47. doi: 10.17116/neiro201882141-47. Epub [PubMed PMID: 29543214]
Allegrini D, Autelitano A, Nocerino E, Fogagnolo P, De Cillà S, Rossetti L. Grisel's syndrome, a rare cause of anomalous head posture in children: a case report. BMC ophthalmology. 2016 Mar 1:16():21. doi: 10.1186/s12886-016-0197-1. Epub 2016 Mar 1 [PubMed PMID: 26931792]
Level 3 (low-level) evidenceMissori P, Marruzzo D, Peschillo S, Domenicucci M. Clinical remarks on acute post-traumatic atlanto-axial rotatory subluxation in pediatric-aged patients. World neurosurgery. 2014 Nov:82(5):e645-8. doi: 10.1016/j.wneu.2014.07.020. Epub 2014 Jul 30 [PubMed PMID: 25084168]
Wu LA, Liu HM, Wang CW, Chen YF, Hong RL, Ko JY. Osteoradionecrosis of the upper cervical spine after radiation therapy for head and neck cancer: differentiation from recurrent or metastatic disease with MR imaging. Radiology. 2012 Jul:264(1):136-45. doi: 10.1148/radiol.12111714. Epub 2012 Apr 10 [PubMed PMID: 22495686]
Level 2 (mid-level) evidenceIskra DA, Koshkarev MA, Litvinenko IV, Dyskin DE, Kovalenko AP. [Manual differential diagnosis of migraine and cervicogenic headache]. Zhurnal nevrologii i psikhiatrii imeni S.S. Korsakova. 2019:119(5):80-85. doi: 10.17116/jnevro201911905180. Epub [PubMed PMID: 31317894]
Shen YF, Zhou QY, Li SL, Jia Y, Qiu ZY. [Clinical manifestations and imaging analysis of cervicogenic headache]. Zhongguo gu shang = China journal of orthopaedics and traumatology. 2019 Feb 25:32(2):130-135. doi: 10.3969/j.issn.1003-0034.2019.02.007. Epub [PubMed PMID: 30884928]
Level 2 (mid-level) evidenceFlorman JE, Cushing DA, England EC, White E. How to Transect the C2 Root for C1 Lateral Mass Screw Placement: Case Series and Review of an Underappreciated Variable in Outcome. World neurosurgery. 2019 Jul:127():e1210-e1214. doi: 10.1016/j.wneu.2019.04.100. Epub 2019 Apr 17 [PubMed PMID: 31004854]
Level 2 (mid-level) evidence