Introduction
The systemic circulation in the human body divides into the arterial blood supply and the venous drainage. These two circulations are linked together by the capillary beds. The arterial blood supply is responsible for perfusing the body with oxygenated and nutrient-rich blood, while the venous blood drainage is responsible for draining the deoxygenated blood and metabolic waste.
The venous system drains the deoxygenated blood back towards the heart. Once the venous blood is in the heart, it will get pumped into the pulmonary circulation for gas exchange. After the gas exchange, the oxygenated blood will return to the body via the arterial system. The veins in the venous system are designed to drain the majority of the blood against gravity. The veins have one-way valves. These valves work to prevent the backflow of the blood, allowing for the venous blood to be pumped back toward the heart. The venous system can further divide into superficial and deep venous systems. For example, the venous drainage of the upper limb splits into a superficial and deep venous drainage system. The superficial veins in the upper limb drain the blood from the skin and superficial fascia. The deep venous system will drain the blood from the deeper fascia, muscles, and bones. Even though the venous system may divide into superficial and deep systems, they share many connections with each other. The external forces support the venous blood vessels from the arteries and the muscles contracting to help propel the blood against gravity.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The structure of the veins in the upper extremity is similar to arteries. The chief difference between the arteries and veins is that veins contain valves in the lumen. The valves are designed to prevent the backflow of blood. Since the venous blood in the upper extremities is draining against gravity. Another characteristic of the veins is that they do not contain as much muscle in their walls as arteries. The valves and the lesser amount of muscle in the veins allow them to expand and act as a reservoir for blood. The veins have a large capacity to hold blood. The veins in the upper extremities rely on the external forces to assist in the propulsion of blood back toward the heart. The external forces exist as muscle contractions and the contractile force of the nearby arteries. The venous drainage of the upper limb divides into the superficial and deep venous systems. The venous drainage in the upper limb starts from the digits and drains toward the heart.
Superficial
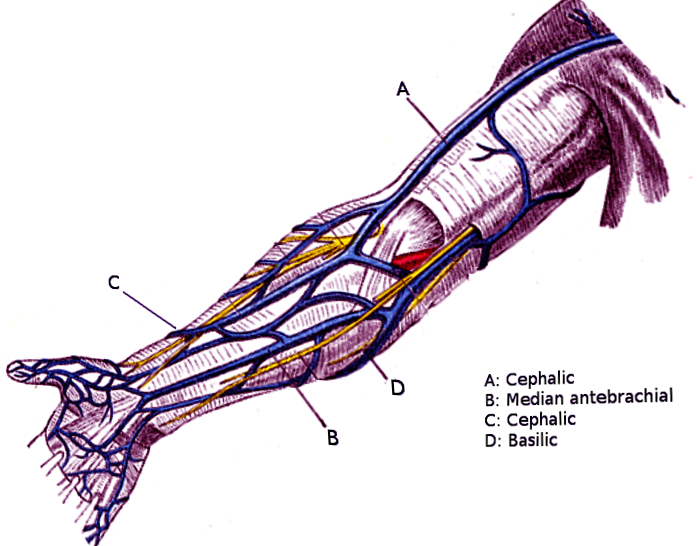
In the hand, the superficial veins will arise from the dorsal venous arch on the dorsum of the hand. The dorsal venous arch drains into the cephalic and the basilic veins. The cephalic and the basilic veins are the principal superficial veins that drain the upper limb. The cephalic vein will drain predominately the radial side of the upper extremity while the basilic vein will drain the medial side. As the cephalic and basilic veins drain towards the cubital fossa, the two veins will become connected by a vein called the median cubital vein. The median cubital vein has a connection to the cephalic vein (median cephalic vein) and a connection to the basilic vein (median basilic vein). As the veins ascend the arm they will drain back into the brachial vein, axillary vein, or subclavian vein. The cephalic vein will penetrate the deep fascia around the axilla region to drain into the subclavian vein. The basilic vein drains either into the brachial or axillary vein.[1][2]
Deep
The deep venous drainage of the upper extremity follows closely with the arterial system. In the hand, there is a venous deep and superficial palmar arch that will drain in the ulnar and radial veins. The main drainage of the hand and forearm will be directed towards the ulnar and radial veins. These veins will travel in pairs around their corresponding arteries. The pair of veins around the arteries in the forearm is called venae comitantes. Once the ulnar and radial veins reach the cubital fossa, they will merge together to form the brachial vein. At the axilla, the brachial vein is renamed the axillary vein. The blood in the axillary vein drains into the subclavian vein. The subclavian veins will merge with the internal jugular veins from the head to form the brachiocephalic veins. The brachiocephalic vein from each upper extremity will merge to form the superior vena cava. The superior vena cava drains into the right atrium of the heart.
Common Pathway
Even though the superficial veins drain mainly the superficial structures and the deep veins drain the deeper structures. The two venous drainage systems connect via perforating veins. The perforating veins ultimately drain into the deep veins all along the upper extremity.
Embryology
During fetal development, structures such as blood vessels derive from mesenchymal tissue. The mesenchymal tissue originates from the mesodermal germ layer. The veins in the upper extremity will develop from mesenchymal tissue. The veins will elongate as the limbs develop and elongate as a part of development.[3]
Blood Supply and Lymphatics
The veins in the upper extremity drain the deoxygenated blood. The drainage of blood allows for oxygenated blood to flow into the upper extremity. The veins do not perfuse the upper extremity with blood.
The lymphatics of the upper extremity follows closely with the veins. The lymphatics drainage start at the hand and drains toward the heart. The superficial lymphatic vessels on the radial side follow closely with the cephalic vein. The superficial lymphatic vessels on the radial side of the hand will drain into the infraclavicular lymph node. The lymphatics of the medial side of the hand follow the basilic vein and drain into the supratrochlear lymph nodes. The supratrochlear lymph nodes are above the medial epicondyle of the humerus. The supratrochlear lymph nodes will eventually drain into the axillary lymph nodes.
The deep lymphatic vessels follow closely with the deep veins. The deep lymphatic drainage is directed towards the axillary lymph nodes. The lymph drainage of the upper extremity will eventually return to the central circulation via the right lymphatic duct or the thoracic duct. The right lymphatic duct drains the right upper extremity, while the thoracic duct drains the left.[4]
Nerves
The primary nerves in the upper extremity originate from the brachial plexus. These nerves are:
- Axillary nerve
- Musculocutaneous nerve
- Radial nerve
- Ulnar nerve
- Median nerve
These nerves will go on and further branch into smaller branches. The smaller branches will innervate the skin and muscles. The deoxygenated blood created by the nerves will get drained via the nearby veins.
The autonomic nervous system innervates the veins. The autonomic nervous system subdivides into the sympathetic nervous system and the parasympathetic nervous system. The sympathetic nervous system can augment the diameter of the vein's lumen by vasoconstriction or the withdrawal of vasoconstriction's stimulus. The sympathetic nervous system function by the release of catecholamines in the form of epinephrine and norepinephrine. These catecholamines will act on the alpha and beta receptors to augment the diameters of the veins. The parasympathetic nervous system augments the venous diameter indirectly. The mechanism of vasodilation of the veins is by acetylcholine triggering the production of nitric oxide. The nitric oxide will diffuse into the smooth muscle that lines the veins and results in relaxation of the smooth muscle. The relaxation of the smooth muscle will cause vasodilation.
Muscles
The muscles in the upper extremity categorize into hand muscles, forearm muscles, and arm muscles. All the muscles in the upper extremity drain via the superficial and deep veins.[5]
Hand Muscles
- Lumbrical muscles
- Dorsal interosseous muscles
- Palmar interosseous muscles
- Adductor pollicis muscle
- Thenar muscles
- Abductor pollicis brevis muscle
- Opponens pollicis muscle
- Flexor pollicis brevis muscle
- Hypothenar muscles
- Opponens digiti minimi muscle
- Flexor digiti minimi muscle
- Abductor digiti minimi muscle
- Palmaris brevis muscle
The muscles in the hand drain into the dorsal venous arch, superficial palmar arch, and the deep palmar arch.
Forearm muscles
- Pronator quadratus muscle
- Flexor pollicis longus muscle
- Flexor digitorum profundus muscle
- Flexor digitorum superficialis muscle
- Pronator teres muscle
- Flexor carpi radialis muscle
- Palmaris longus muscle
- Flexor carpi ulnaris muscle
- Supinator muscle
- Abductor pollicis longus muscle
- Extensor pollicis brevis muscle
- Extensor pollicis longus muscle
- Extensor indicis muscle
- Extensor carpi radialis brevis muscle
- Extensor digitorum muscle
- Extensor digiti minimi muscle
- Extensor carpi ulnaris muscle
- Brachioradialis muscle
- Extensor carpi radialis longus muscle
The venous drainage of the muscle located in the forearm directs towards the radial and ulnar veins. The forearm muscles that have tendon attaches in the hand will also drain into the dorsal venous arch, superficial palmar arch, and deep palmar arch.
Arm Muscles
- Coricobrachialis muscle
- Biceps brachii muscle
- Brachialis muscle
- Triceps brachii muscle
The arm muscles will drain into the brachial, axillary, and subclavian vein. The muscles that have an attachment in the forearm will also drain into the ulnar and radial veins.
The venous drainage of the muscles in the upper extremity may follow the nearest vein, but ultimately the venous system for the muscles in the upper extremity has some overlap. The overlap is due to muscle origins and insertions. The connections between the superficial veins and the deep veins by the perforating veins also create collateral venous drainage.
Physiologic Variants
The venous system of the upper extremity has many variations. The network of interconnecting veins occurs at many different points. The connections between the deep veins and the superficial veins exist at many variable sites. The only consistency is that the upper extremity's veins eventually drain back into the superior vena cava via the subclavian veins.[6] The size of the veins varies greatly. Typically, the basilic vein is the larger superficial vein in the arm, but sometimes the cephalic is larger. The drainage of the basilic vein also varies. The basilic vein is found to drain directly into the brachial vein or the axillary vein.[6][7]
Surgical Considerations
The veins in the arm are sometimes used in dialysis. In surgery, the surgeon may elect to place an arteriovenous shunt or fistula for patients needing dialysis.[8][9] An arteriovenous shunt can be made by anastomosing the vein directly to the artery; this creates a blood flow that will ultimately bypass the capillary beds.[10] Dialysis is a common procedure in patients with kidney disease.
The veins in the upper extremities can also suffer from varicosities, which is a condition where the veins become engorged and enlarged due to venous insufficiency. When the veins exist as varicose veins, an individual can elect to get them removed for cosmetic reasons.[11]
Clinical Significance
In the clinical setting, the anatomy of the veins is essential for procedures that involve puncturing the veins. These procedures can range from simple venous blood sampling to intravenous catheterization. The median cubital vein is a common site for venous blood sampling. The biceps aponeurosis protects the median cubital vein; it protects the vein and prevents the formation of hematomas.
The presentation of the veins may also be used as clinical clues when treating patients. In rare cases, there could be unilateral or bilateral dilation of the veins in the upper extremities. The dilation in the upper extremities can be due to venous insufficiency or a blockage of the subclavian vein, brachiocephalic vein, or the superior vena cava.[12]
Other Issues
The veins in the upper extremities can suffer from conditions that are commonly associated with the lower extremities. The veins in both the upper and lower extremities can be affected by deep vein thrombosis (DVT).[13][14][15] DVT can result in pain and swell in the area affected. The worst outcome of a DVT is the thrombosis embolizing. The embolization can result in occlusion of the pulmonary arteries. The occlusion of the pulmonary arteries could result in right heart failure, hypoxia, pulmonary hypertension, and pulseless electrical activity. The feared outcome of a pulmonary embolism is death.
The veins in the upper extremities can also be affected by inflammation and infection; this results in a condition called thrombophlebitis. Thrombophlebitis is treatable, but if thrombophlebitis reoccurs in different locations, this is termed "migratory thrombophlebitis." Migratory thrombophlebitis is associated with adenocarcinoma, predominately pancreatic adenocarcinoma.[16]
Media
References
Radkowski CA, Richards RS, Pietrobon R, Moorman CT 3rd. An anatomic study of the cephalic vein in the deltopectoral shoulder approach. Clinical orthopaedics and related research. 2006 Jan:442():139-42 [PubMed PMID: 16394752]
Loukas M, Myers CS, Wartmann ChT, Tubbs RS, Judge T, Curry B, Jordan R. The clinical anatomy of the cephalic vein in the deltopectoral triangle. Folia morphologica. 2008 Feb:67(1):72-7 [PubMed PMID: 18335417]
Araújo RC, Pires LAS, Andrade ML, Perez MC, Filho CSL, Babinski MA. Embryological and comparative description of the cephalic vein joining the external jugular vein: A case report. Morphologie : bulletin de l'Association des anatomistes. 2018 Mar:102(336):44-47. doi: 10.1016/j.morpho.2017.10.002. Epub 2017 Nov 11 [PubMed PMID: 29133232]
Level 2 (mid-level) evidenceMa CX, Pan WR, Liu ZA, Zeng FQ, Qiu ZQ, Liu MY. Deep lymphatic anatomy of the upper limb: An anatomical study and clinical implications. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2019 May:223():32-42. doi: 10.1016/j.aanat.2019.01.005. Epub 2019 Feb 1 [PubMed PMID: 30716466]
Level 2 (mid-level) evidenceForro SD, Munjal A, Lowe JB. Anatomy, Shoulder and Upper Limb, Arm Structure and Function. StatPearls. 2023 Jan:(): [PubMed PMID: 29939618]
Sadeghi A, Setayesh Mehr M, Esfandiari E, Mohammadi S, Baharmian H. Variation of the cephalic and basilic veins: A case report. Journal of cardiovascular and thoracic research. 2017:9(4):232-234. doi: 10.15171/jcvtr.2017.40. Epub 2017 Oct 15 [PubMed PMID: 29391938]
Level 3 (low-level) evidenceLee HS, Song YR, Kim JK, Choi SR, Joo N, Kim HJ, Park P, Kim SG. Anatomical variants of upper arm veins on preoperative mapping venography for hemodialysis access in Korean adults. The journal of vascular access. 2019 May:20(3):270-275. doi: 10.1177/1129729818803870. Epub 2018 Oct 11 [PubMed PMID: 30306819]
Fontseré N, Mestres G, Yugueros X, Jiménez M, Burrel M, Gómez F, Ojeda R, Rodas LM, Lozano V, Riambau V, Maduell F. Brachiobasilic arteriovenous fistula with superficialisation and transposition the basilic vein in a one stage surgical technique. Five years of single experience. Nefrologia. 2019 Jul-Aug:39(4):388-394. doi: 10.1016/j.nefro.2018.11.010. Epub 2019 Mar 8 [PubMed PMID: 30853141]
Sheta M, Hakmei J, London M, Wooster M, Aruny J, Ross J, Illig KA. One- versus two-stage transposed brachiobasilic arteriovenous fistulae: A review of the current state of the art. The journal of vascular access. 2020 May:21(3):281-286. doi: 10.1177/1129729819862694. Epub 2019 Aug 1 [PubMed PMID: 31366302]
Gehl HB, Bohndorf K, Gladziwa U, Handt S, Günther RW. Imaging of hemodialysis fistulas: limitations of MR angiography. Journal of computer assisted tomography. 1991 Mar-Apr:15(2):271-5 [PubMed PMID: 2002107]
Brittenden J, Cooper D, Dimitrova M, Scotland G, Cotton SC, Elders A, MacLennan G, Ramsay CR, Norrie J, Burr JM, Campbell B, Bachoo P, Chetter I, Gough M, Earnshaw J, Lees T, Scott J, Baker SA, Tassie E, Francis J, Campbell MK. Five-Year Outcomes of a Randomized Trial of Treatments for Varicose Veins. The New England journal of medicine. 2019 Sep 5:381(10):912-922. doi: 10.1056/NEJMoa1805186. Epub [PubMed PMID: 31483962]
Level 1 (high-level) evidenceLindblad B, Bornmyr S, Kullendorff B, Bergqvist D. Venous haemodynamics of the upper extremity after subclavian vein thrombosis. VASA. Zeitschrift fur Gefasskrankheiten. 1990:19(3):218-22 [PubMed PMID: 2238816]
Sanson H, Gautier V, Stansal A, Sfeir D, Franceschi C, Priollet P. [Deep venous thrombosis of the upper limb in a violin player: The "bow syndrome"]. Journal des maladies vasculaires. 2016 Dec:41(6):396-402. doi: 10.1016/j.jmv.2016.10.004. Epub 2016 Nov 4 [PubMed PMID: 27823916]
Shiva C, Saini M. Paget-von Schroetter Syndrome: Upper Extremity Deep Vein Thrombosis after Continuous Lifting of Heavy Weight. The Journal of the Association of Physicians of India. 2015 Aug:63(8):84-5 [PubMed PMID: 27604444]
Rainey CE, Taysom DA, Rosenthal MD. Upper extremity deep venous thrombosis. The Journal of orthopaedic and sports physical therapy. 2014 Apr:44(4):313. doi: 10.2519/jospt.2014.0405. Epub [PubMed PMID: 24684195]
Level 3 (low-level) evidenceThayalasekaran S, Liddicoat H, Wood E. Thrombophlebitis migrans in a man with pancreatic adenocarcinoma: a case report. Cases journal. 2009 Apr 29:2():6610. doi: 10.1186/1757-1626-2-6610. Epub 2009 Apr 29 [PubMed PMID: 19829832]
Level 3 (low-level) evidence