Introduction
Amebiasis is a parasitic infection caused by the protozoan, Entamoeba histolytica; transmitted through fecal-oral route. The infection can manifest ranging from an asymptomatic state to multiple complications associated with liver abscesses. Amebic liver abscess is the most common extraintestinal manifestation of amebiasis. Men between the ages of 18 and 50 are most commonly affected. Areas with high rates of amebic infection include India, Africa, Mexico, and Central and South America. Approximately 80% of patients with this disease will develop symptoms within 2 to 4 weeks, including fever and right upper quadrant abdominal pain with 10% to 35% of patients experiencing associated gastrointestinal symptoms. The diagnosis is based on the clinical symptoms and relevant epidemiology coupled with radiographic studies and serologic tests. Optimal treatment includes the use of Metronidazole followed by a luminal agent such as Paromomycin. Rarely, therapeutic aspiration is indicated. [1],[2] Sir William Osler diagnosed the first case of liver abscess in the USA[3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Entamoeba histolytica is a parasitic protozoan that is a common cause of amoebic colitis. This particular amoeba causes about 40 million infections annually, with deaths of up to 100,000 per year. [4] In comparison to E. despar, which also occurs in humans via the fecal-oral route, it is nonpathogenic and may present as an asymptomatic carrier. [4] Many Entamoeba species, namely E. dispar and E. moshkovskii infect humans, but only E. histolytica causes amebiasis. The only natural host for E. histolytica includes both human and Non-Human primates, which accounts for the infection that occurs. [5]
Epidemiology
Amebic liver abscess is uncommon in children and ten times more common in men than in women, particularly in individuals between the ages of 18 and 50. The reason for such a striking difference is not clear but thought to be due to factors such as hormonal effects and alcohol consumption. In the United States, most cases are found in immigrants from endemic areas and people living in states bordering Mexico. Worldwide, areas with high rates of infection include India, Africa, and Mexico and parts of Central and South America. Most individuals are infected by ingesting contaminated food or water although other modes of transmission include oral and anal sex, particularly among men who have sex with men.[6][4] Around 2% to 5% of patients with intestinal amebiasis may end up with liver abscess.[3] This organism is distributed throughout the world, posing a substantial risk in countries without adequate sanitation of municipal water supplies. [4]
Pathophysiology
The life cycle of Entameba Histolytica was first explained by Clifford Dobell in 1928. The organism has 2 stages of life, the cystic stage which is the infective stage and the trophozoite stage which ends up causing invasive disease[3]Upon ingestion of contaminated food and water; the infection starts with ingestion of the quadrinucleate cyst of E. histolytica. Excystation in the small intestinal lumen is followed by production of motile, potentially invasive trophozoites. In most infections, the trophozoites form new cysts and are limited to the intestinal mucin layer. In other cases, the trophozoites adhere to and lyse the colonic epithelium with subsequent invasion of the colon. Neutrophils respond, resulting in further cellular damage at the invasion site. Once the trophozoites invade the colonic epithelium, subsequent spread to extraintestinal sites such as the liver (by hematogenous spread through the portal circulation) and peritoneum can occur. [7]The organism causes hepatic inflammation followed by necrosis which results in an abscess formation[8]
Toxicokinetics
Adherence of E. histolytica to colonic epithelial cells is thought to be through the galactose/N-acetylgalactosamine-specific lectin. E. histolytica carries cytolytic capabilities and also kills mammalian cells through programmed apoptosis. Once E. histolytica trophozoites reach the liver, they create abscesses comprising well-circumscribed areas of cellular debris, dead hepatocytes, and liquefied cells. The lesion is surrounded by a rim of connective tissue with some inflammatory cells and amebic trophozoites. In humans, the small number of organisms compared to the actual dimensions of the abscess supports the concept that E. histolytica can destroy hepatocytes without contact with the cells.
History and Physical
Patients can present with amebic liver abscess months to years after travel to an endemic area, making a thorough travel history and knowledge of epidemiologic risk factors imperative. In the United States, the typical patient with an amebic liver abscess is an immigrant (usually Hispanic male) between the ages of 20 and 40. Eighty percent of patients will develop symptoms within 2 to 4 weeks of exposure, including fever, dull and aching right upper quadrant or epigastric abdominal pain, and cough. Patients who present subacutely will have weight loss and less frequent development of fever and abdominal pain. Ten percent to 35% of patients have gastrointestinal symptoms including nausea, vomiting, abdominal cramps, diarrhea, constipation, or abdominal distension. On exam, hepatomegaly with point tenderness either over the liver, below the ribs, or in the intercostal spaces is typical for liver abscess.
Evaluation
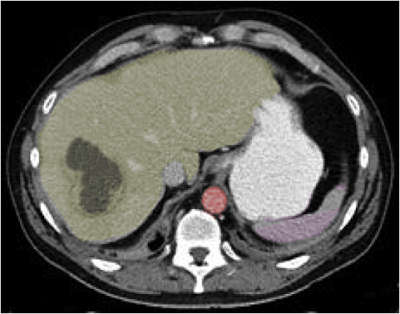
Patients with an amebic liver abscess will typically have evidence of leukocytosis, elevated serum transaminases, alkaline phosphatase on laboratory evaluation. On imaging, most amebic liver abscesses will be found in the right lobe. Imaging modalities include ultrasound which might show around, hypo-echoic mass, CT scan can identify a low-density mass with peripheral enhancing rim, and MRI typically shows low signal intensity on the T1-weighted image and high signal intensity on T2-weighted image, which are fairly sensitive but without absolute specificity for an amebic liver abscess. Travel history to an endemic area, coupled with typical signs and symptoms and visualization of lesions on imaging should make one consider this entity and should be followed by doing the serologic testing. Serum antigen detection has a sensitivity of over 95% with serologic testing (indirect hemagglutination) having a sensitivity of 70% to 80% in acute disease and greater than 90% in the convalescent state. It should be noted that in the first week of the disease course, there may be false-negative serologic tests. On the other hand, stool microscopy, has a sensitivity of only 10% to 40%. [9]
Treatment / Management
Treatment entails the use of a Nitroimidazole, preferably Metronidazole at a dose of 500 mg to 750 mg by mouth 3 times per day for 7 to10 days. Alternatively, Tinidazole 2 gm by mouth daily for 3 days can be used. Since the parasites can persist in the intestine in 40% to 60% of patients, treatment with a Nitroimidazole should always be followed with a luminal agent such as Paromomycin 500 mg 3 times a day for 7 days or Iodoquinol 650 mg three times a day for 20 days[8]. Metronidazole and Paromomycin should not be given at the same time because diarrhea, a common side effect of paromomycin, can make assessing response to therapy difficult. Around 15% of patients with amebic liver abscess fail medical treatment. Therapeutic aspiration can be done either by percutaneous needle aspiration or by percutaneous catheter drainage. These options should be considered in patients with no clinical response to antibiotics within 5 to 7 days, in those with a high risk of abscess rupture (cavitary diameter over 5 cm or presence of lesions in the left lobe), or in cases of bacterial coinfection of amebic liver abscess.[10]. Between percutaneous needle aspiration and percutaneous catheter drainage, studies have shown that the latter is superior with higher success rate and quicker resolution[11](A1)
Differential Diagnosis
- Bacterial Liver abscess
- Echinococcus Granulosus
- Candida
- Salmonella Typhi
Prognosis
For simple abscess, the prognosis is excellent.
Complex abscesses and large abscesses can rupture and may be associated with a high mortality.
Overall, most patients have a favorable outcome with prompt treatment.
Complications
An amebic liver abscess may rupture into the chest, abdomen or pericardium
Rare complications include Inferior vena cava Thrombosis, Hepatic vein thrombosis, Intra abdominal mass
Consultations
- General surgeon
- interventional Radiologist
- Infectious disease
Deterrence and Patient Education
Preventive measures include reducing fecal contamination of food and water and emphasizing the use of safe sexual practices, particularly in men who have sex with men. An effective vaccine would be instrumental in improving health in developing countries, particularly in children. Once considered a fatal infection, amebic liver abscess is now considered a curable condition.
Pearls and Other Issues
Diligence in maintaining local water sources and emphasis on counseling men who have sex with men regarding safe sexual practices are of paramount importance in preventing amebiasis.
Stool studies have less than 50% positive results
Serology studies can be negative in the first week of infection
Treatment with a Nitroimidazole should always be followed with a luminal agent
Enhancing Healthcare Team Outcomes
The care of amebic liver abscess depends on the complexity of the liver abscess. The treatment of amebic liver abscess requires an interprofessional team to lower the morbidity and mortality of the disorder. [12]
- The laboratory technologist is essential for the diagnosis. Serum antigen detection and stool microscopy are often the first laboratory studies ordered to make the diagnosis and rule out other pathologies.
- For complex abscesses, Interventional radiologist will need to be consulted for image-guided drainage.
- If the abscess is multi-locular, then the general surgeon may have to perform an open or laparoscopic surgery to help drain the collections.
- Because many of the drugs used to treat amebic liver abscess have adverse effects, the pharmacist will need to monitor the patients. Emetin is used as a second-line drug, but it is important to monitor the patient as the drug can cause cardiac arrhythmias.
- The nurse may need to monitor the patient in outpatient clinics to ensure that the patient is symptom-free. More importantly, the nurse plays a vital role in public education regarding sanitary measures, personal hygiene, and food washing.
- Patients considering travel to areas where amebiasis is endemic may wish to schedule an infectious disease consult on precautions to take such as boiling drinking water, washing food regularly, and changing sexual practices to avoid fecal-oral contamination.
Outcomes
When an interprofessional team approach is undertaken, the prognosis for most patients with an amebic liver abscess is excellent.[13] To avoid complications like rupture into the lung, pericardium, or abdomen, patients with amebic liver abscess need a prompt referral to an infectious disease expert for treatment. Current evidence reveals that drainage of complex abscess can improve outcomes as opposed to medical management.[14] (Level III)
Media
(Click Image to Enlarge)
References
Lardière-Deguelte S, Ragot E, Amroun K, Piardi T, Dokmak S, Bruno O, Appere F, Sibert A, Hoeffel C, Sommacale D, Kianmanesh R. Hepatic abscess: Diagnosis and management. Journal of visceral surgery. 2015 Sep:152(4):231-43. doi: 10.1016/j.jviscsurg.2015.01.013. Epub 2015 Mar 12 [PubMed PMID: 25770745]
Wijewantha HS. Liver Disease in Sri Lanka. Euroasian journal of hepato-gastroenterology. 2017 Jan-Jun:7(1):78-81. doi: 10.5005/jp-journals-10018-1217. Epub 2017 May 5 [PubMed PMID: 29201778]
Arellano-Aguilar G, Marín-Santillán E, Castilla-Barajas JA, Bribiesca-Juárez MC, Domínguez-Carrillo LG. A brief history of amoebic liver abscess with an illustrative case. Revista de gastroenterologia de Mexico. 2017 Oct-Dec:82(4):344-348. doi: 10.1016/j.rgmx.2016.05.007. Epub 2017 Apr 21 [PubMed PMID: 28438363]
Level 3 (low-level) evidenceKannathasan S, Murugananthan A, Kumanan T, de Silva NR, Rajeshkannan N, Haque R, Iddawela D. Epidemiology and factors associated with amoebic liver abscess in northern Sri Lanka. BMC public health. 2018 Jan 10:18(1):118. doi: 10.1186/s12889-018-5036-2. Epub 2018 Jan 10 [PubMed PMID: 29316900]
Stanley SL Jr. Amoebiasis. Lancet (London, England). 2003 Mar 22:361(9362):1025-34 [PubMed PMID: 12660071]
Level 3 (low-level) evidenceKannathasan S, Murugananthan A, Kumanan T, Iddawala D, de Silva NR, Rajeshkannan N, Haque R. Amoebic liver abscess in northern Sri Lanka: first report of immunological and molecular confirmation of aetiology. Parasites & vectors. 2017 Jan 7:10(1):14. doi: 10.1186/s13071-016-1950-2. Epub 2017 Jan 7 [PubMed PMID: 28061872]
Albenmousa A, Sanai FM, Singhal A, Babatin MA, AlZanbagi AA, Al-Otaibi MM, Khan AH, Bzeizi KI. Liver abscess presentation and management in Saudi Arabia and the United Kingdom. Annals of Saudi medicine. 2011 Sep-Oct:31(5):528-32. doi: 10.4103/0256-4947.84635. Epub [PubMed PMID: 21911993]
Level 2 (mid-level) evidenceWuerz T, Kane JB, Boggild AK, Krajden S, Keystone JS, Fuksa M, Kain KC, Warren R, Kempston J, Anderson J. A review of amoebic liver abscess for clinicians in a nonendemic setting. Canadian journal of gastroenterology = Journal canadien de gastroenterologie. 2012 Oct:26(10):729-33 [PubMed PMID: 23061067]
Wong WK, Foo PC, Olivos-Garcia A, Noordin R, Mohamed Z, Othman N, Few LL, Lim BH. Parallel ELISAs using crude soluble antigen and excretory-secretory antigen for improved serodiagnosis of amoebic liver abscess. Acta tropica. 2017 Aug:172():208-212. doi: 10.1016/j.actatropica.2017.05.017. Epub 2017 May 12 [PubMed PMID: 28506795]
Waghmare M, Shah H, Tiwari C, Khedkar K, Gandhi S. Management of Liver Abscess in Children: Our Experience. Euroasian journal of hepato-gastroenterology. 2017 Jan-Jun:7(1):23-26. doi: 10.5005/jp-journals-10018-1206. Epub 2017 May 5 [PubMed PMID: 29201767]
Cai YL, Xiong XZ, Lu J, Cheng Y, Yang C, Lin YX, Zhang J, Cheng NS. Percutaneous needle aspiration versus catheter drainage in the management of liver abscess: a systematic review and meta-analysis. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2015 Mar:17(3):195-201. doi: 10.1111/hpb.12332. Epub 2014 Sep 10 [PubMed PMID: 25209740]
Level 1 (high-level) evidenceKouamé N, N'goan-Domoua AM, Akaffou E, Konan AN. [Multidisciplinary management of amebic liver abscesses at the University Hospital of Yopougon, Abidjan, Côte d'Ivoire]. The Pan African medical journal. 2010:7():25 [PubMed PMID: 21918712]
Level 2 (mid-level) evidenceKale S, Nanavati AJ, Borle N, Nagral S. Outcomes of a conservative approach to management in amoebic liver abscess. Journal of postgraduate medicine. 2017 Jan-Mar:63(1):16-20. doi: 10.4103/0022-3859.191004. Epub [PubMed PMID: 27652983]
Lübbert C, Wiegand J, Karlas T. Therapy of Liver Abscesses. Viszeralmedizin. 2014 Oct:30(5):334-41. doi: 10.1159/000366579. Epub [PubMed PMID: 26287275]