Introduction
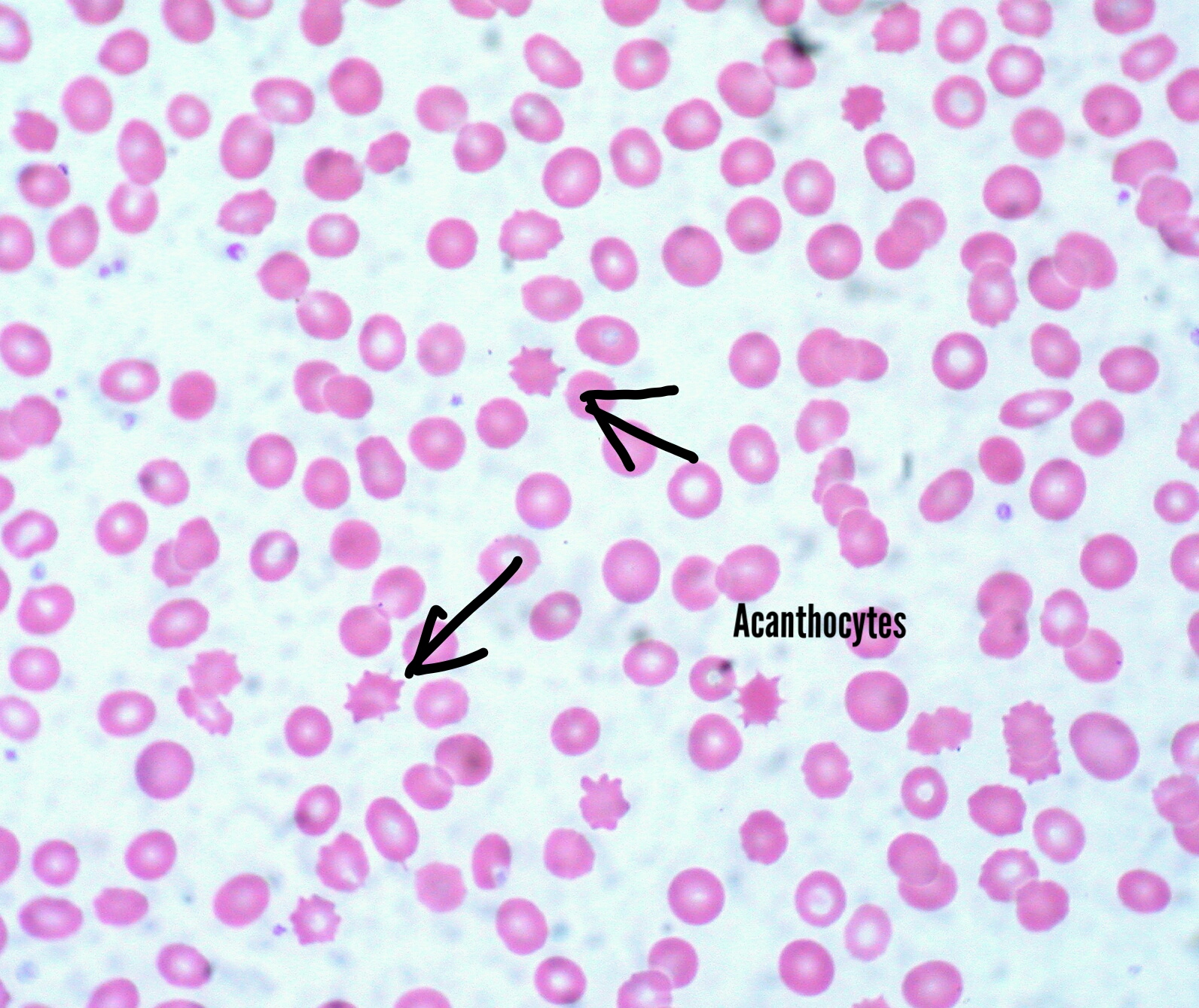
The membrane of red blood cells (RBCs) can undergo a variety of changes leading to morphologic alterations in these cells. When viewed under a freshly prepared peripheral blood smear (PBS), acanthocytes appear as cells with a few spicules of different sizes, projecting from the surface of the RBC membrane at irregular intervals. They result from alterations in membrane lipids and proteins and occur in patients with severe liver dysfunction, neuroacanthocytosis, abetalipoproteinemia, malnutrition, hypothyroidism, post-splenectomy, etc.[1] The clinical significance of acanthocytes lies in their vulnerability to splenic trapping and destruction due to their morphology, which ultimately leads to anemia.[2] When remodeled by the spleen in liver disease patients, acanthocytes develop more blunt spicules and become relatively more spherocytic; these are known as spheroacanthocytes or ‘spur cells.’
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
It is important to differentiate acanthocytes from echinocytes, which have smaller and more uniform projections and present in patients with end-stage renal disease, liver disease, pyruvate kinase deficiency, etc. The spiculated appearance of RBCs can also result from an ethylene diamine tetra-acetic acid (EDTA) artifact after a delay of more than 6 hours between storage and smear preparation. Therefore for accuracy, it is crucial to ensure that the peripheral blood smear is fresh when read. Spiculated RBCs from EDTA artifact have more uniformly distributed spicules and affect almost all of the RBCs in the film.[3]
In addition, the detection of spiculated red blood cells and hemolysis during the neonatal period shall raise the possibility of a hereditary disorder such as infantile pyknocytosis berfore considering an acquired causes of acanthocytosis. [4]
Causes
Common causes of acanthocytosis are listed here and discussed in detail in the section below:
- Severe liver dysfunction
- Abetalipoproteinemia
- McLeod syndrome and chorea-acanthocytosis syndrome
- Post-splenectomy
- Hypothyroidism
- Myelodysplastic syndromes
- Anorexia nervosa
- Medications
Clinicopathologic Correlations
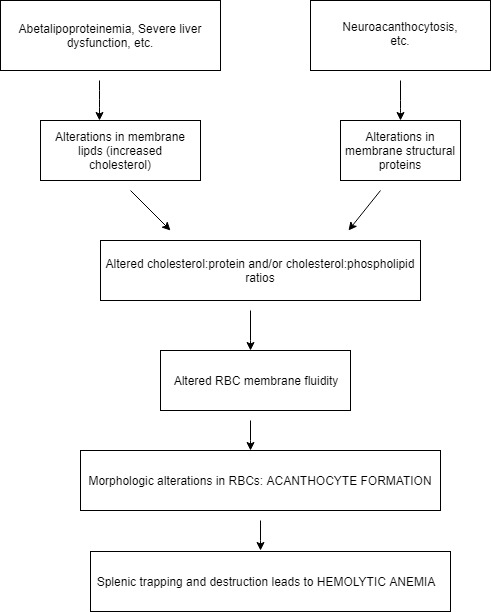
For maintenance of fluidity of RBC morphology, membrane fluidity is essential. This fluidity is, in turn, controlled by proportions of cholesterol, structural proteins, and phospholipids in the RBC membrane. Diseases such as abetalipoproteinemia, severe liver dysfunction, etc. and neuroacanthocytosis, etc. affect the cholesterol and protein content of the RBC membrane, respectively. Subsequently, the RBC membrane fluidity becomes altered, and the cells undergo morphologic changes leading to the formation of acanthocytes or spur cells. These structural modifications make them susceptible to splenic trapping and destruction, ultimately leading to hemolytic anemia.
Additionally, there has been a different hypothesis suggesting that a component of the RBC membrane skeleton, band 3 is responsible for acanthocyte formation.[5]
Clinical Significance
Clinical conditions associated with acanthocytosis:
- Severe liver dysfunction: Spur cell anemia (SCA) is a poorly studied clinical entity in liver disease, and its clinical importance remains as yet undefined. It gets diagnosed with the following: Hb is less than10 mg/dl, hemolysis, over 5% spur cells on PBS, and the exclusion of other causes of anemia. Seen in severe liver disease patients regardless of the etiology, it is known to portend an unfavorable prognosis as a majority of patients die within months of diagnosis. SCA is characteristically not amenable to treatment with blood transfusion, as transfused cells tend to undergo morphological alterations as well [2]. It is important to note that SCA is readily reversible after liver transplantation (LT).[6] Although with limited success, there have been reports that have suggested various other modalities of treatment for SCA, such as plasmapheresis, transjugular intrahepatic portosystemic shunt, etc. These treatments may be useful in patients awaiting LT or in those who are poor candidates for LT.[7][8]
- Abetalipoproteinemia: Also known as Basseg-Kornzweig Syndrome, abetalipoproteinemia is a disease that presents in infants with failure to thrive, diarrhea, vomiting, and fat malabsorption. Acanthocytes are characteristically visible on PBS, with associated hemolytic anemia, reticulocytosis, and raised bilirubin levels. Malabsorption of fat-soluble vitamins such as Vit A, D, E, and K results in the majority of the clinical manifestations. Vit K deficiency may result in a raised international normalized ratio in these patients and an increased risk of bleeding. Untreated individuals also possess a risk of development of progressive loss of night or color vision. Neuromuscular symptoms (Vit E deficiency) such as ataxia, muscle weakness, dysarthria, etc. usually manifest during the first or second decades of life. Although no formal clinical criteria exist, absent or extremely low LDL cholesterol, triglycerides, and apolipoprotein B levels are needed to establish a diagnosis of abetalipoproteinemia. Molecular genetic testing may be required to identify and confirm mutations in the MTTP gene in these individuals.
Appropriate intake of calories along with low-fat diet and supplementation of vitamins A, D, E, and K are needed to treat manifestations of the disease. Long-term follow-up to monitor growth and potential complications are needed. Identification of genetic variants in genes such as MTTP may help guide the evaluation of relatives at risk and offer genetic counseling to prospective parents.[9][10]
- Neuroacanthocytosis: Two main neuroacanthocytosis syndromes are known:
- Chorea-acanthocytosis- Autosomal recessive
- McLeod syndrome- X-linked inheritance
Clinically, the common characteristics of these two neurodegenerative disorders are as follows[11][12]:
- Chorea
- Dystonia
- Peripheral neuropathy
- Myopathy
- Seizures
- Psychiatric symptoms
Hematologically, acanthocytosis is seen on PBS in these patients. The belief is that genetic mutations lead to the absence of proteins such as XK protein in McLeod syndrome, which leads to acanthocytosis and hemolytic anemia following splenic remodeling. Males with McLeod syndrome are more likely to have acanthocytosis and hemolytic anemia than females. Increased degradation and phosphorylation of membrane proteins along with increased RBC sphingomyelin have implications in the causation of acanthocytosis in chorea-acanthocytosis patients.[13][14][15][16]
Overall, hemolytic anemia associated with acanthocytosis in neuroacanthocytosis syndromes is mild but may, on occasion, warrant blood transfusion. In patients, autologous blood transfusions may be needed to prevent immune-mediated blood transfusion reactions.
Others: Other clinical conditions associated with acanthocytosis are listed below-
- Post-splenectomy: Splenectomy leads to several morphologic changes in RBCs, including acanthocytosis.
- Hypothyroidism: Mild acanthocytosis may present in about 20% of patients with hypothyroidism. Thyroid function tests should merit consideration in patients with acanthocytosis after the exclusion of all other causes.[17]
- Hematologic abnormalities: Acanthocytosis may also occur in patients with myelodysplasia and some forms of hereditary spherocytosis. A proportion of patients with myelodysplasia may be referred to a hematologist with acanthocytosis as the presenting finding.[18]
- Anorexia nervosa: Some patients may also have acanthocytosis with anorexia nervosa. This condition may be due to changes in RBC membrane lipids or proteins and is reversible with treatment of anorexia.
- Drug-associated: Statins are one of the commonly prescribed drugs that have been found to be associated with acanthocytosis. This reversible change may result from the reduction in serum lipids caused by statins.[1] Another drug that has implications in acanthocytosis is misoprostol.[19]
Conclusions/Learning points:
- Acanthocytes appear as cells with a few spicules of different sizes, projecting from the surface of the RBC membrane at irregular intervals.
- They result from alterations in membrane lipids and proteins and occur in patients with severe liver dysfunction, neuroacanthocytosis, abetalipoproteinemia, hypothyroidism, post-splenectomy, etc.
- The clinical significance of acanthocytes lies in their vulnerability to splenic trapping and destruction due to their morphology, which ultimately leads to hemolytic anemia.
- For an accurate diagnosis of acanthocytes, it is essential to ensure that the peripheral blood smear is fresh when read.
Media
(Click Image to Enlarge)
References
Pacheco JM, Yilmaz M, Rice L. How low is too low: Statin induced hemolysis. American journal of hematology. 2016 Feb:91(2):267. doi: 10.1002/ajh.24105. Epub 2015 Oct 16 [PubMed PMID: 26147873]
Privitera G, Meli G. An unusual cause of anemia in cirrhosis: spur cell anemia, a case report with review of literature. Gastroenterology and hepatology from bed to bench. 2016 Fall:9(4):335-339 [PubMed PMID: 27895861]
Level 3 (low-level) evidenceAnoop P, Parker-Williams J. Morphological diagnosis of abetalipoproteinemia and the importance of a freshly prepared peripheral smear. European journal of haematology. 2009 Dec 1:83(6):606. doi: 10.1111/j.1600-0609.2009.01302.x. Epub 2009 Jun 22 [PubMed PMID: 19552676]
Level 3 (low-level) evidenceEl Nabouch M, Rakotoharinandrasana I, Ndayikeza A, Picard V, Kayemba-Kay's S. Infantile pyknocytosis, a rare cause of hemolytic anemia in newborns: report of two cases in twin girls and literature overview. Clinical case reports. 2015 Jul:3(7):535-8. doi: 10.1002/ccr3.288. Epub 2015 May 8 [PubMed PMID: 26273436]
Level 3 (low-level) evidenceWong P. A basis of the acanthocytosis in inherited and acquired disorders. Medical hypotheses. 2004:62(6):966-9 [PubMed PMID: 15142658]
Level 3 (low-level) evidenceMalik P, Bogetti D, Sileri P, Testa G, Blumenthal SA, Wiley TE, Layden TJ, Benedetti E. Spur cell anemia in alcoholic cirrhosis: cure by orthotopic liver transplantation and recurrence after liver graft failure. International surgery. 2002 Oct-Dec:87(4):201-4 [PubMed PMID: 12575799]
Level 3 (low-level) evidenceMiki K, Maruki T, Imashuku S. Plasmapheresis for Spur Cell Anemia in a Patient with Alcoholic Liver Cirrhosis. Case reports in hematology. 2018:2018():9513946. doi: 10.1155/2018/9513946. Epub 2018 Jun 21 [PubMed PMID: 30034891]
Level 3 (low-level) evidenceChitale AA, Sterling RK, Post AB, Silver BJ, Mulligan DC, Schulak JA. Resolution of spur cell anemia with liver transplantation: a case report and review of the literature. Transplantation. 1998 Apr 15:65(7):993-5 [PubMed PMID: 9565106]
Level 3 (low-level) evidenceAdam MP, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A, Burnett JR, Hooper AJ, Hegele RA. Abetalipoproteinemia. GeneReviews(®). 1993:(): [PubMed PMID: 30358967]
Di Filippo M, Créhalet H, Samson-Bouma ME, Bonnet V, Aggerbeck LP, Rabès JP, Gottrand F, Luc G, Bozon D, Sassolas A. Molecular and functional analysis of two new MTTP gene mutations in an atypical case of abetalipoproteinemia. Journal of lipid research. 2012 Mar:53(3):548-555. doi: 10.1194/jlr.M020024. Epub 2012 Jan 11 [PubMed PMID: 22236406]
Level 3 (low-level) evidenceJung HH, Danek A, Walker RH. Neuroacanthocytosis syndromes. Orphanet journal of rare diseases. 2011 Oct 25:6():68. doi: 10.1186/1750-1172-6-68. Epub 2011 Oct 25 [PubMed PMID: 22027213]
Hermann A, Walker RH. Diagnosis and treatment of chorea syndromes. Current neurology and neuroscience reports. 2015:15(2):514. doi: 10.1007/s11910-014-0514-0. Epub [PubMed PMID: 25620691]
Walker RH. Management of Neuroacanthocytosis Syndromes. Tremor and other hyperkinetic movements (New York, N.Y.). 2015:5():346. doi: 10.7916/D8W66K48. Epub 2015 Oct 19 [PubMed PMID: 26504667]
Asano K, Osawa Y, Yanagisawa N, Takahashi Y, Oshima M. Erythrocyte membrane abnormalities in patients with amyotrophic chorea with acanthocythosis. Part 2. Abnormal degradation of membrane proteins. Journal of the neurological sciences. 1985 May:68(2-3):161-73 [PubMed PMID: 3159851]
Olivieri O, De Franceschi L, Bordin L, Manfredi M, Miraglia del Giudice E, Perrotta S, De Vivo M, Guarini P, Corrocher R. Increased membrane protein phosphorylation and anion transport activity in chorea-acanthocytosis. Haematologica. 1997 Nov-Dec:82(6):648-53 [PubMed PMID: 9499662]
Level 3 (low-level) evidenceClark MR, Aminoff MJ, Chiu DT, Kuypers FA, Friend DS. Red cell deformability and lipid composition in two forms of acanthocytosis: enrichment of acanthocytic populations by density gradient centrifugation. The Journal of laboratory and clinical medicine. 1989 Apr:113(4):469-81 [PubMed PMID: 2703759]
Level 3 (low-level) evidencePerillie PE, Tembrevilla C. Letter: Red-cell changes in hypothyroidism. Lancet (London, England). 1975 Dec 6:2(7945):1151-2 [PubMed PMID: 53639]
Level 3 (low-level) evidenceDoll DC, List AF, Dayhoff DA, Loy TS, Ringenberg QS, Yarbro JW. Acanthocytosis associated with myelodysplasia. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 1989 Oct:7(10):1569-72 [PubMed PMID: 2778485]
Level 2 (mid-level) evidenceFilippini A, Villa G, Corrocher R, De Franceschi L. Acute hemolytic anemia with acanthocytosis associated with high-dose misoprostol for medical abortion. Annals of emergency medicine. 2007 Sep:50(3):289-91 [PubMed PMID: 17084939]
Level 3 (low-level) evidence