Introduction
Facial implants enhance the aesthetics of the aging or underdeveloped face and can correct asymmetry secondary to trauma or congenital malformations. The areas where facial implants are commonly used for enhancement include the chin, zygomas, and mandibular angles. The 2020 American Society of Plastic Surgeons member survey revealed that malar implant surgery was the most commonly performed facial implant surgery and the 3rd most frequently performed cosmetic surgical procedure. The treatment's popularity has increased by 938% since 2000. Chin implants also increased by 63% in the same time frame. Facial implants may be used on other bony surfaces, like the nose, glabella, and temple, though less commonly.[1]
The ideal implant is chemically inert, biocompatible, and easy to manipulate. However, implants are foreign bodies that come with a host of risks. Facial implants can be organic or synthetic. Synthetic facial implant materials used within the United States are numerous, but the most commonly used presently are polyethylene, silicone, and titanium. Autogenic grafts, once common, have fallen out of favor due to long-term unpredictability.[2]
One of the most common facial implant complications is poor cosmesis, often due to asymmetry. Rare but severe complications include infection and bone erosion. Fortunately, providers can remove implants if these conditions arise.[3] The implants that allow soft tissue ingrowth are more challenging to remove than solid implants that form a fibrous capsule.[4]
Software-aided comprehensive analysis helps determine the proper surgical treatment for a patient's facial defect. Facial analysis is still evolving with technological advancements, including three-dimensional (3D) treatment planning. Bony relations are easily compared in two-dimensional (2D) images and are used to help determine their soft tissue counterpart. For instance, the lateral cephalogram is the foundation for genioplasty evaluation. Midface deficiency evaluation is challenging with 2D radiographs and may improve with further studies.
Multiple criteria have been developed to help providers make objective-based decisions. Additionally, the ebb and flow of society's fads must be considered. Clinical success depends upon diagnostic accuracy, appropriate facial analysis, correct implant selection, and good surgical technique.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Vital structures must be noted when placing facial implants. The most important are the face's sensory and motor nerves, vasculature, and musculature.
Trigeminal Nerve
Cranial nerve V (CN V), the trigeminal nerve, supplies sensation to the face and motor control to a select muscle group. CN V has divisions V1 to V3, each exiting the skull through a different foramen. Some of these nerves' terminal branches reach the viscerocranium's facial surface and penetrate their targeted soft tissue.[5] Some trigeminal nerve branches are at greatest injury risk from implant placement at their exit points.
CN V1, the ophthalmic division, exits the skull through the superior orbital fissure. This nerve has 3 main branches: frontal, lacrimal, and nasociliary. The frontal branch travels through the orbit, exits superiorly, and forms the supraorbital and supratrochlear nerves. These nerves supply the sensory innervation of the upper eyelid, conjunctiva, and scalp. The lacrimal nerve is the smallest of CN V1's branches. This nerve communicates with the zygomatic nerve, supplies small skin and conjunctival areas in the lateral upper eyelid, and contributes to lacrimal gland innervation. The nasociliary nerve diverges while inside the orbit. This nerve's terminal branches include the infratrochlear and external nasal nerves, which supply the medial aspect of the upper lid and dorsum of the nose.
CN V2, the maxillary division, exits the skull through the foramen rotundum. This division has 2 main branches, the infraorbital (IO) and zygomatic. The IO nerve reaches the viscerocranium's surface via the maxilla's IO foramen and supplies the soft tissues from the lower lid to the upper lip. The zygomatic branch travels along the lateral orbit before dividing into zygomaticotemporal (ZT) and zygomaticofacial (ZF), which exit through foramina with the same names and supply the temple region and malar eminence's skin. All 3 nerves risk injury during subperiosteal dissection with zygomatic implants.
CN V3, the mandibular division, exits the skull via the forament ovale. This nerve has numerous branches, including the pterygoid, masseteric, deep temporal, buccal, auriculotemporal, lingual, and inferior alveolar nerves. The mandibular division arises from trigeminal motor and sensory fibers that fuse before exiting the skull. This division supplies the mastication muscles. The mandibular division is not at risk of injury during implant placement as the fibers penetrate their target muscles outside the dissection plane.
The inferior alveolar nerve enters the mandibular ramus medially. This nerve travels through the mandible's body and becomes the mental nerve as it exits laterally at the mental foramen apical to the 1st and 2nd premolar (see Image. Mental Nerve). The foramen is approximately 1.5 cm superior to the mandible's inferior border.[6]
After exiting its foramen, the mental nerve gives off 3 branches that run deep to the depressor anguli oris muscle. This nerve supplies sensation to the lower lip, chin, and gingival tissue associated with the mandibular incisors. The mental nerve is often encountered in genioplasties.[7]
Facial Nerve
Cranial nerve VII (CN VII), the facial nerve, supplies the facial expression muscles. CN VII branches are not directly encountered during dissection for facial implants. However, these nerves may be injured by stretching or compression during the procedure. CN VII exits the skull through the stylomastoid foramen before entering the parotid gland. The nerve has 5 branches, coursing deep to the superficial muscular aponeurotic system (SMAS). The facial nerve branches are the temporal, zygomatic, buccal, mandibular, and cervical nerves.
The temporal branch travels superiorly to innervate the frontalis and orbicularis oculi's superior aspect. The zygomatic and buccal branches course deep below the masseteric fascia. These nerves pass near the dissection plane and are thus at a higher risk of injury during subperiosteal dissection for zygomatic implant placement. The zygomatic branch innervates the orbicularis oculi's inferior aspect and nasal area muscles. The buccal branch innervates the upper lip and cheek muscles. The marginal mandibular nerve exits the parotid at the mandibular angle and follows the angle's inferior border. Injury to this nerve weakens the mentalis and depressor anguli oris—the muscles that move the lower lip. The facial nerve's cervical branch innervates the platysma.[8]
Facial Vasculature
The facial blood supply arises from external carotid artery branches. Major vessels are at the highest risk during the initial incision as they travel through the soft tissue, and dissection is carried out in the subperiosteal plane. An exception to this is when they form a neurovascular bundle and exit the viscerocranium. For example, the infraorbital and mental nerves travel with arteries and veins of similar names as they leave their foramina.
Facial Musculature
The facial expression muscles lie subcutaneously in the anterior and posterior scalp, face, and neck. Most facial muscles attach to bone or fascia, producing facial expressions by pulling the skin. The facial nerve innervates all facial muscles. Table 1 below summarizes important information about the muscles of facial expression.
Table 1. Facial Muscles
|
Muscle |
Origin |
Insertion |
Action(s) |
|
Occipitofrontalis frontal belly |
Epicranial aponeurosis |
Eyebrow and forehead skin and subcutaneous tissue |
Raises eyebrows, wrinkles forehead skin, and protracts scalp (the surprised expression) |
|
Occipitofrontalis occipital belly |
Superior nuchal line's lateral two-thirds |
Epicranial aponeurosis |
Retracts scalp, assists the frontal belly |
|
Orbicularis oculi |
Medial orbital margin, medial palpebral ligament, and lacrimal bone |
Skin around the orbital margin, superior and inferior tarsal plates |
Palpebral portion gently closes the eyelids, orbital part tightly closes the eyelids |
|
Corrugator supercilii |
Superciliary arch's medial side |
Skin superior to the supraorbital area and superciliary arch |
Pulls eyebrows inferomedially (the worried expression) |
|
Procerus and transverse nasalis part |
Facial aponeurosis over the nasal bone and lateral nasal cartilage |
Skin in the inferior forehead area and between the eyebrows |
Lowers the eyebrow's medial edge, wrinkles skin over the nose (the disgusted or disdainful expression) |
|
Alar nasalis part and levator labii superioris alaeque nasii |
Frontal maxillary process |
Major alar cartilage |
Lowers the nasal alae laterally, widens the anterior nasal aperture (nasal flaring when angry) |
|
Orbicularis oris |
Medial maxilla and mandible, mouth angle, deep perioral skin |
Lips' mucous membrane |
Closes the oral fissure, compresses and protrudes the lips (when kissing), and prevents distension (when blowing) |
|
Levator labii superioris |
Infraorbital maxillary area |
Upper lip skin |
Dilates the mouth, elevates and everts the upper lip, and deepens the nasolabial sulcus (the sad expression) |
|
Zygomaticus minor |
Anterior zygomatic border |
Upper lip skin |
Dilates the mouth, elevates and everts the upper lip, and deepens the nasolabial sulcus (the sad expression) |
|
Buccinator |
Mandible, maxilla's alveolar process, mandible's alveolar part, and pterygomandibular raphe |
Orbicularis oris and mouth angle (modiolus) |
Compresses the cheek against the molars, coordinates with the tongue during chewing, prevents distension (when blowing) |
|
Zygomaticus major |
Lateral zygomatic border |
Modiolus |
Dilates the mouth, raises the labial commissure bilaterally to smile or unilaterally to show disdain |
|
Levator anguli oris |
Infraorbital maxillary area |
Modiolus |
Dilates the mouth, widens the oral fissure (to grin or grimace) |
|
Risorius |
Parotid fascia, buccal skin |
Modiolus |
Dilates the mouth, lowers the labial commissure (to frown or express sadness) |
|
Depressor anguli oris |
Anterolateral mandibular base |
Modiolus |
Dilates the mouth, lowers the labial commissure (to frown or express sadness) |
|
Depressor labii inferioris |
Platysma, mandibular body's anterolateral aspect |
Lower lip skin |
Dilates the mouth, lowers and everts the lower lip (to pout or express sadness) |
|
Mentalis |
Mandibular body |
Chin skin |
Raises and protrudes the lower lip, raises the chin skin (the doubting expression) |
|
Platysma |
Infraclavicular and supraclavicular subcutaneous tissue |
Mandibular base, cheek and lower lip skin, modiolus, orbicularis oris |
Lowers the mandible against resistance, tightens the inferior facial and neck skin (the tense expression) |
Mastication Muscles
Chin and malar implants are placed in areas where the mastication muscles attach or closely interact with facial bones. These muscles are essential for chewing and speaking and also aid in making facial expressions. Motor supply to the mastication muscles is via the anterior mandibular nerve trunk of CN V3. Poorly placed implants can result in discomfort and impaired function of these muscles. Important information about the mastication muscles is summarized in Table 2.
Table 2. Mastication Muscles
|
Muscle |
Origin |
Insertion |
Action(s) |
|
Temporalis |
Temporal fossa floor and deep temporal fascial surface |
Coronoid process and anterior aspect of the mandibular ramus |
Raises the mandible (jaw closing), posterior portion retrudes the mandible after protrusion |
|
Masseter |
Zygomatic arch and bone’s inferior and medial aspects |
Angle and lateral aspect of the mandibular ramus |
Raises and protrudes the mandible (jaw closing), deep portion retrudes the mandible |
|
Lateral pterygoid |
Superior head: greater wing of the sphenoid bone Inferior head: lateral pterygoid plate’s lateral aspect |
Superior head: joint capsule and articular disc of the temporomandibular joint Inferior head: pterygoid fovea (on the neck of mandibular condyloid process) |
Bilaterally: protrude the mandible and lower the chin Unilaterally, alternately: produce side-to-side mandibular movements (chewing) |
|
Medial pterygoid |
Deep head: lateral pterygoid plate’s medial aspect, palatine pyramidal process Superficial head: maxilla’s tuberosity |
Medial aspect of mandibular ramus, inferior to mandibular foramen |
Bilaterally: help raise the mandible (jaw closing), protrude the mandible Unilaterally, alternately: protrude the jaw laterally, produce grinding movements |
Indications
Facial implant indications are functionally or esthetically driven and include the following:
- Loss of soft tissue support
- Volume loss
- Facial asymmetry secondary to growth discrepancies
- Congenital syndromes
Bony viscerocranial atrophy occurs in the 3rd and 4th decades of life. Decreased skeletal support can accentuate aging, especially since resorption is not even. Areas with more pronounced resorption include the infraorbital and pyriform maxillary areas, leading to midfacial deficiency. Osseocutaneous ligaments, including the zygomatic and mandibular, attach to the corresponding bone's periosteum and overlying skin.[9] The masseter ligaments span from the muscle to the skin. Weakening and decreased elasticity of these ligaments contribute to the ptotic effect of gravity.
The face consists of several fat pads separated by septa and fascia. These fat pads atrophy with age. The malar fat pads consist of superficial and deep fat pads separated by the superficial musculoaponeurotic system (SMAS). Jowls, for example, form from the bilateral descent of the superficial subcutaneous fat over the inferior mandibular borders. Jowls are due to fat loss, skin and muscle ptosis, and bony support loss. Genioplasty alone will not correct a prejowl sulcus. An osteotomy performed as part of a genioplasty can deepen a prejowl sulcus. Therefore, prejowl implant surgery is the treatment of choice for correction, although augmentation can occur at the chin alone, prejowl, or both.[10]
Asymmetries are present in numerous congenital deformities and vary in presentation. Human skull growth occurs in multiple vectors: transverse, sagittal, and vertical. The maxilla typically grows anteriorly, inferiorly, and laterally, while the condyles grow superoposteriorly, pushing the mandible anteroinferiorly. The chin stops growing before the rest of the mandible, which continues to develop transversely and vertically.[11] Deviations from the typical growth pattern introduce mandibular rotation, creating a dolichocephalic (long, retrognathic, and vertical) or brachycephalic (short, prognathic, and horizontal) appearance. Growth usually stops at 14 to 16 years old in female individuals and 16 to 18 in male individuals.[12] Individuals with hypoplastic mandibles can correct the dental malocclusion with orthodontics if present. However, the remaining skeletal defect permits further correction with orthognathic surgery, implant augmentation, or both.[13]
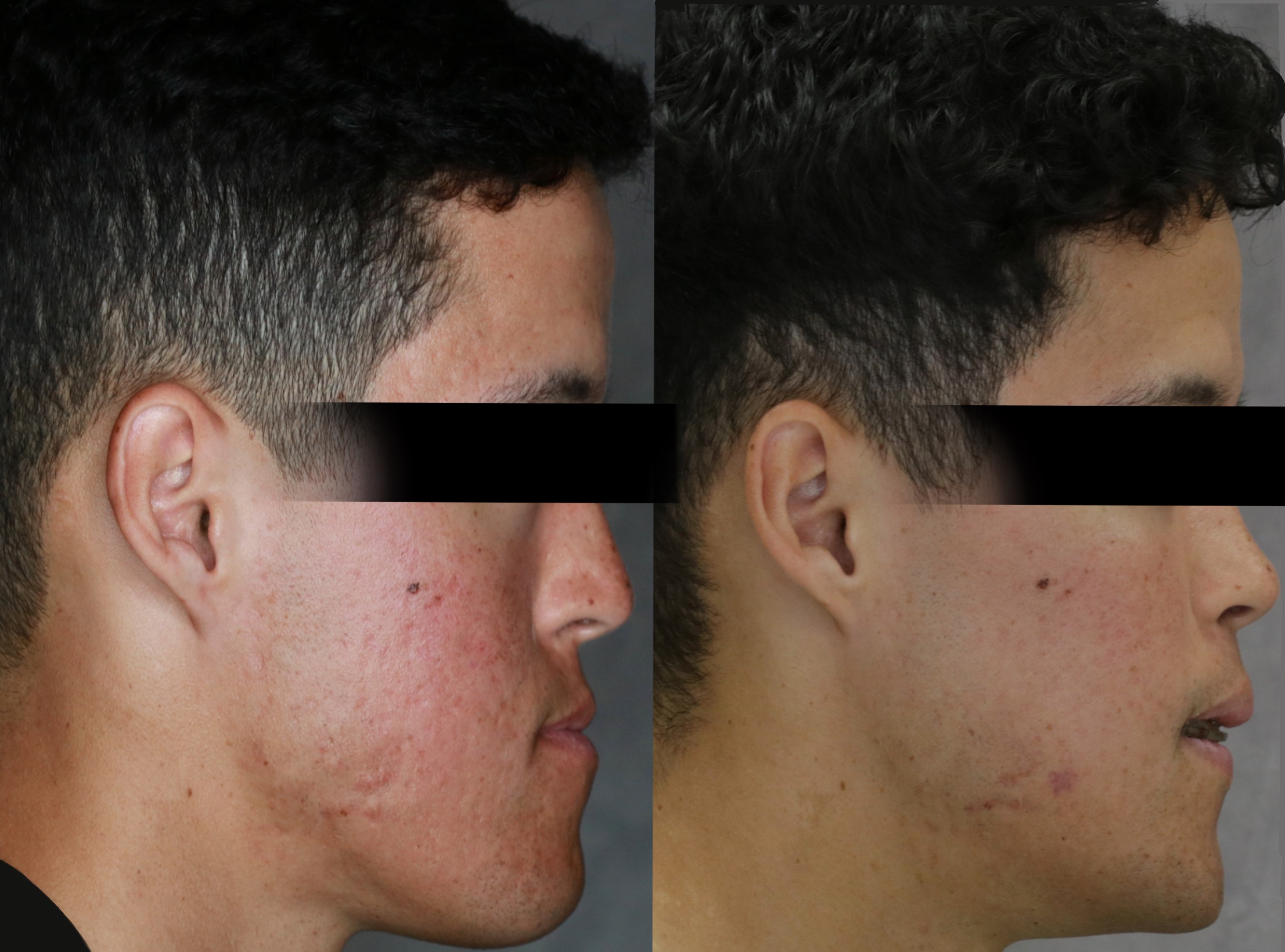
Congenital syndromes that involve the 1st and 2nd brachial arch cause various craniofacial defects. Craniofacial microsomia, for example, commonly affects the maxilla, mandible, and orbits, among other structures. This condition is the 2nd most common congenital deformity after cleft lip and palate. Craniofacial microsomia presents diversely, and multiple classification systems exist.[14] Implants may be an excellent choice for people with milder forms of the disorder. Implant procedures may also be attempted in individuals with craniofacial microsomia who previously underwent corrective procedures like orthognathic surgery. (see Image. Zygomatic Submalar Implant).
Patients with clefts usually have a midfacial deficiency, often with a hypoplastic malar region. Although Le Fort I osteotomies aid in some midface deficiencies, eg, in the lip and nasolabial angle, the role of Le Fort osteotomies in correcting the malar region is controversial. Implants can correct deficient areas after orthognathic surgery.[15]
Contraindications
Facial implant surgery has few contraindications, which include:
- Incomplete growth
- Large volume deficit better treated by other means
- Current infection
- Inadequate bony and soft tissue support
Growth patterns and predictions are important to consider when evaluating facial implants. Female individuals start and stop growing on average sooner than male individuals.[16] "Growth cessation" has many different definitions. The Craniofacial Growth Consortium Study compared different definitions of this term. Growth cessation was defined in 1 of 2 ways: growth less than 0.1 mm per year or growth rate less than 10% of the peak growth velocity. Serial cephalograms help determine growth cessation. Linear distances of series cephalograms are used to compare the growth rate.[17]
Skeletal with dental malocclusions are better suited for orthognathic surgery. Osteotomies are indicated for more extensive augmentations. However, patient preference may favor implant placement. Thin tissue limits the implant placement area size due to the increased risk of implant visibility and palpation.
Equipment
Standard facial implants are alloplastic and may consist of 1 of the following materials:
- Titanium mesh: Titanium implants are inert, nonresorbable, and rigid. Titanium implants are used for recontouring deficient mandibular angles, adding length and width. The mesh is fenestrated to allow tissue ingrowth and create stability.[18]
- High-density porous polyethylene (HDPE): These polymeric implants are rigid, noncompressible, and thermoplastic. HDPE implants come in various pore sizes and densities, ranging from 80 to 400 microns.[19] Pore size influences the tissue ingrowth type, ie, bone or fibrous tissue, occurring after implantation. The range of about 100 to 250 microns has been shown to allow bony ingrowth. However, implants with such pore sizes require fixation to prevent neovascularization disruption.[20] HDPE implants come in preformed shapes but may be recontoured owing to their thermoplasticity. Recontouring may be done by increasing the implant's temperature to 180 °F before carving with a scalpel.[21]
- Silicone: These implants are nonporous and may be composed of solid silicone or dimethylsiloxane subunits. Nonporous implants do not allow tissue ingrowth and become encapsulated, thus requiring fixation to the underlying bone for immobilization. Implant fixation can reduce the dead space between the implant and bone, reducing the chance of tissue ingrowth and seroma formation. Fixation also limits bony resorption, migration, and unaesthetic results.[22]
- Autogenous implant: Autograft use in cosmetic augmentation is limited due to bony resorption unpredictability. One reason is that autograft bone must be under stress to prevent resorption, an example of Wolff's Law. This law states that bone will adapt and remodel to withstand stress. Thus, minimal impact on implant sites leads to decreased bone density due to the absence of stimulation.[23] Autografts also create donor site morbidity, increased surgical time, and complexity.[24]
During the procedure, intravenous (IV) deep or general anesthesia induction can help attain the desired anesthesia depth. Local analgesia is then obtained using lidocaine and a longer-lasting anesthetic like marcaine. Local anesthetics are usually drawn from a vial and administered with a dental syringe and a 27-gauge needle. A #15 blade or bovie electrocautery is used for the appropriate incision.
The surgical armamentarium is similar regardless of the implant location and type. The table below summarizes the materials and equipment used for various aspects of the procedure.
Table 3. Materials and Equipment for Facial Implant Surgery
| Purpose | Materials and Equipment |
Purpose |
Materials and Equipment |
| Local anesthesia |
|
Irrigation |
|
| Incision |
|
Fixation |
|
| Tissue elevation |
|
Closure |
|
| Tissue retraction |
|
Miscellaneous |
|
| Implants |
|
Medications |
|
Personnel
The surgical team may be comprised of as few as 2 individuals: the surgeon and the assistant. However, a cosurgeon will often be present. A 2nd team may be composed of an anesthesiologist, with or without a nurse anesthetist, and may assist the surgeon by providing deep or general anesthesia.
Operating room nurses and technicians also play active roles in general anesthesia cases. Oral maxillofacial surgeons can administer deep anesthesia during procedures, but surgical teams typically have an anesthesia provider on board. Nerve testing is not routine in facial implant surgery, as the dissection plane allows tissue reflection without nerve involvement. Exposed nerves, such as the mental and infraorbital nerves, are easily identifiable and protected throughout the surgery.
Preparation
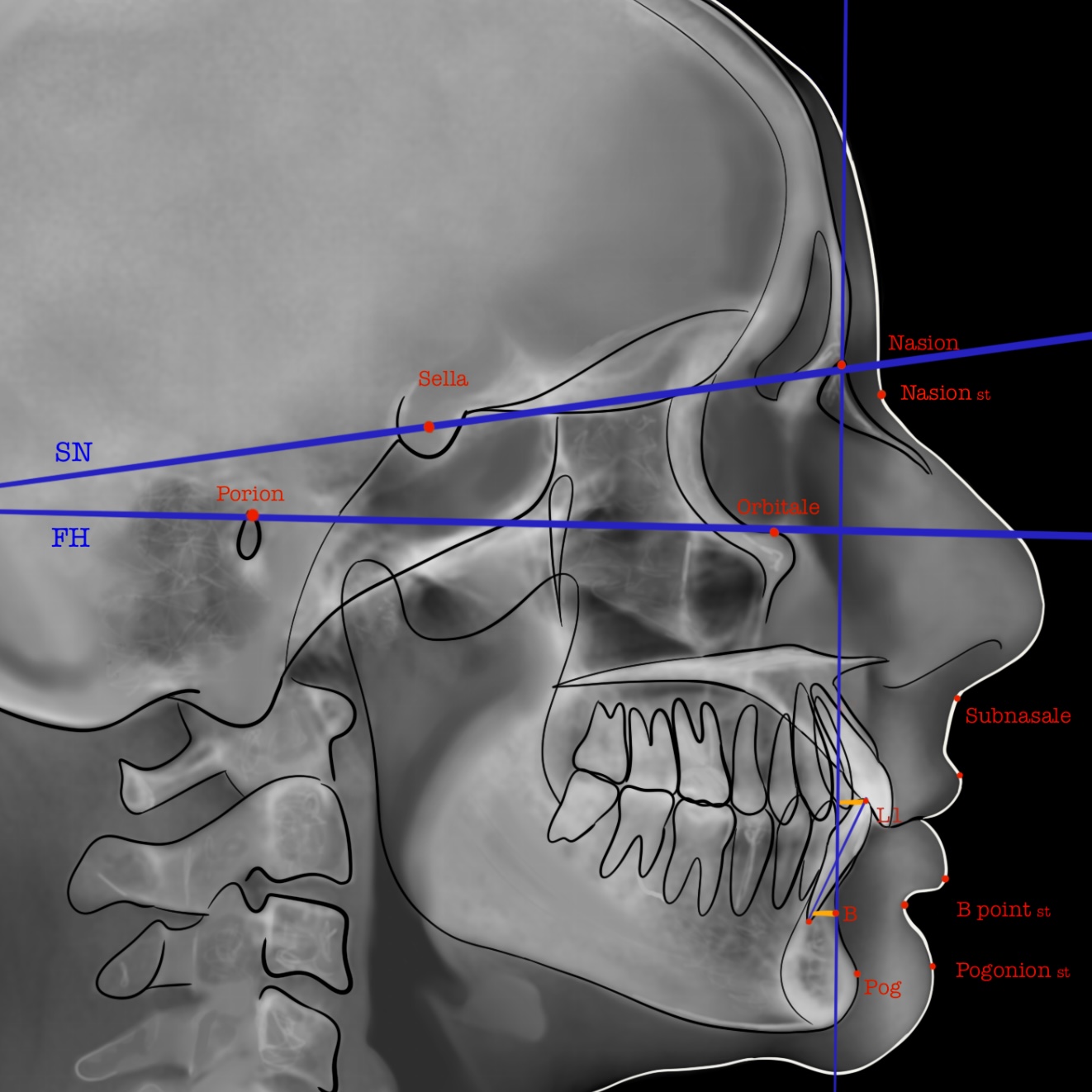
Human facial cosmetic evaluation advances as 3D technology improves. Currently, providers use 2D photos that complement both 2D and 3D radiographs. Photos are taken with the patient looking directly at the camera, at a 45° angle, and in profile view. Each photo allows facial volume visualization from different angles. The lateral cephalogram should be well studied and analyzed, as it contains critical data used for facial analysis. Well-known facial bone and soft tissue relationships are determined from this radiograph.
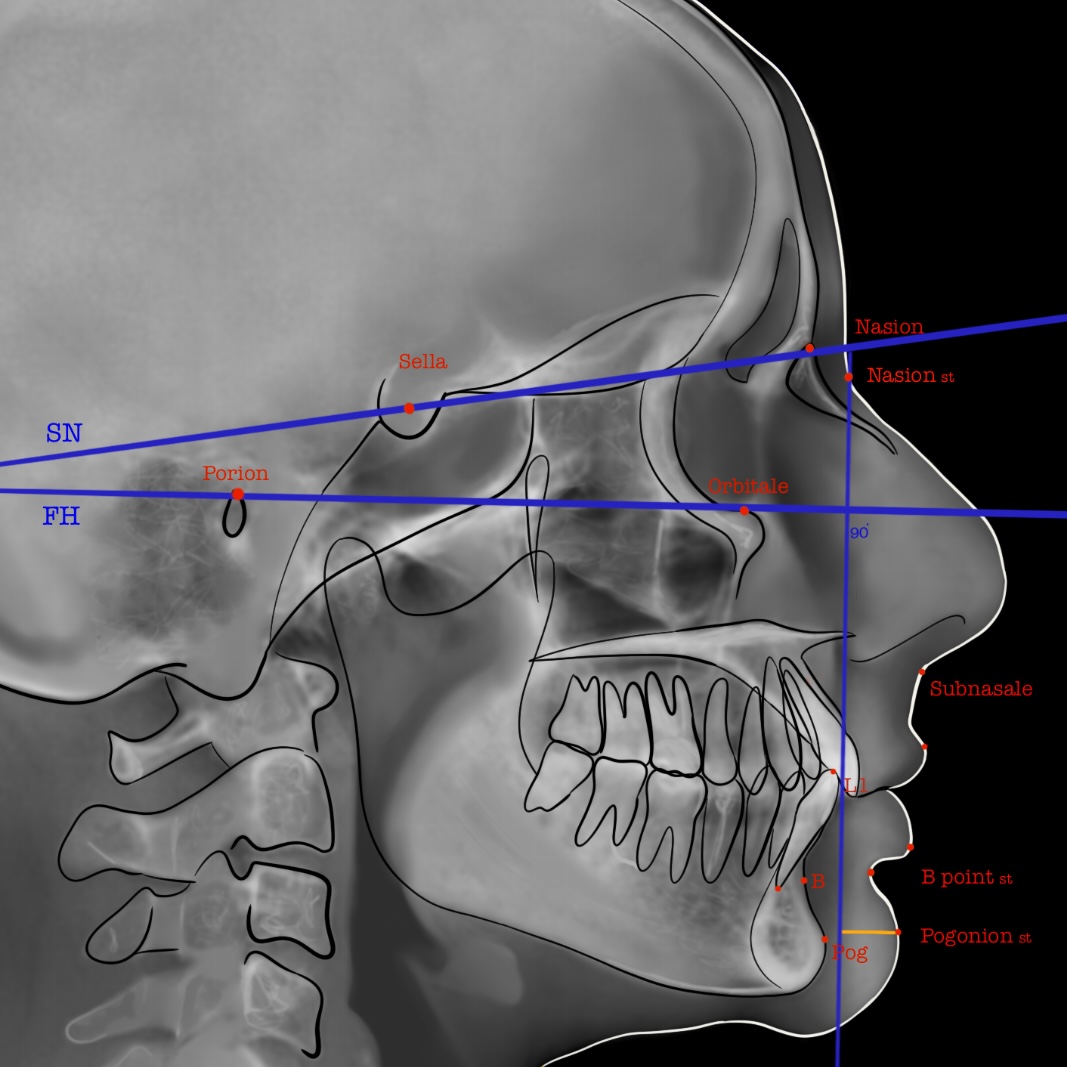
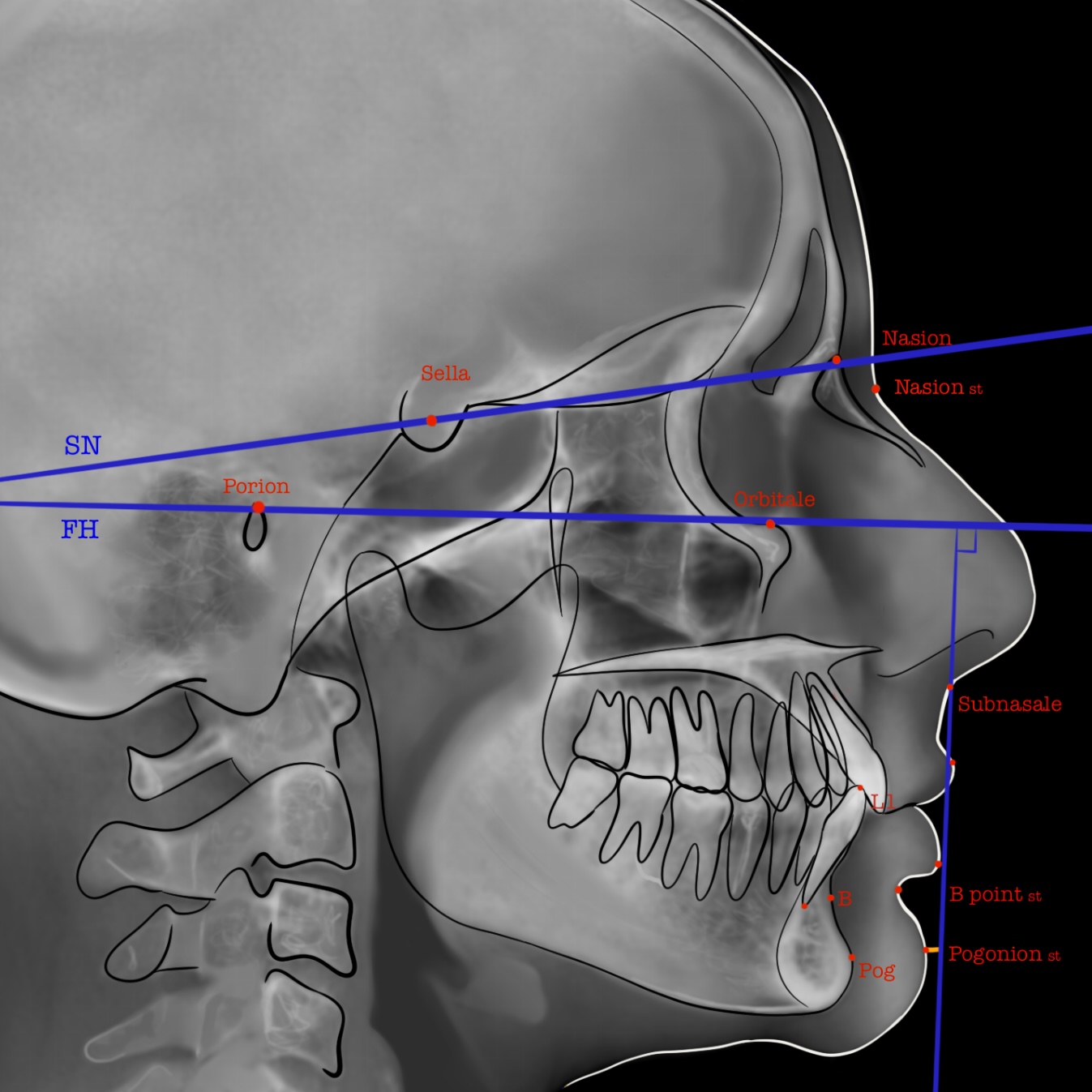
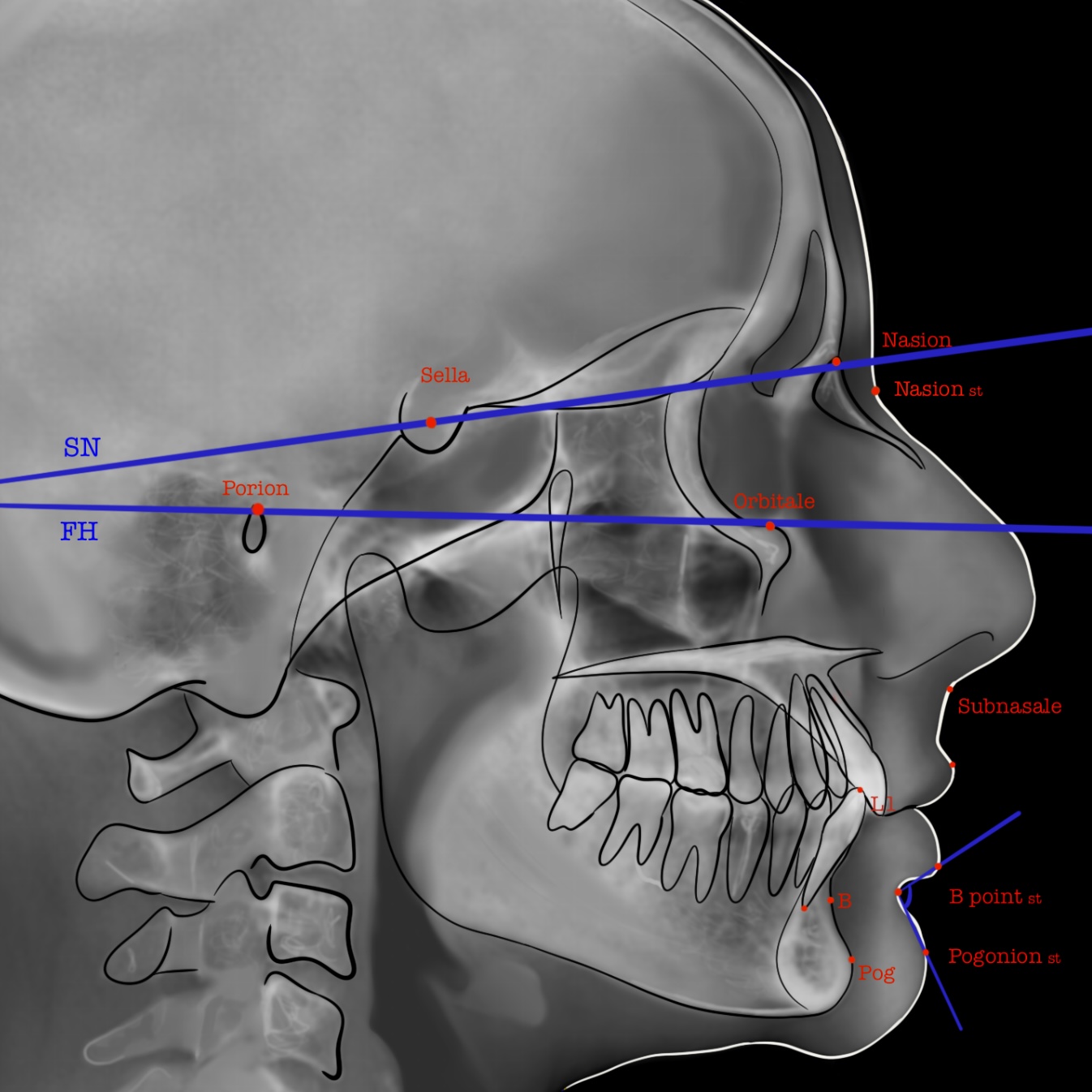
The chin's position and the lower facial structural relationships may be classified based on numerous measurements. Frequently used parameters include the following:
- Holdaway Ratio (see Image. Holdaway Ratio)
- Zero Degree Meridian Line (see Image. Zero Degree Meridian)
- True Vertical Line (see Image. True Vertical Line)
- Labiomental Angle (see Image. Labiomental Angle)
The Holdaway ratio compares the chin's bony position to the lower incisor tips. This ratio involves 4 points: the pogonion (Po), lower incisor tip (L1), nasion (N), and B point (B). Po is the bony chin's most anterior aspect. B is the anterior mandible's most concave aspect. N denotes the nasofrontal suture area. To get the Holdaway ratio, the vertical line connecting N to B is measured. The distance in millimeters from Po to N-B and L1 to N-B should be equal, ie, must have a 1:1 ratio. A deviation of more than 4 mm warrants correction. Excessive lower incisor proclination increases this ratio and distorts accurate analysis.
The zero-meridian line is a perpendicular line that crosses the Frankfort horizontal (FH) line at the nasion. This line evaluates the chin position. The FH line connects the top of the external auditory meatus to the orbit's lowest point. The distance between the pogonion and the zero-meridian line should be 0 mm for female individuals and up to 2 mm for male individuals.
The true vertical line is perpendicular to FH and transects the subnasale (Sn), the point where the nasal columella and upper lip intersect. Niani found that mandibular retrusion of up to 4 mm or protrusion of up to 2 mm from the true vertical line may not be visibly noticeable to people without specialized facial surgical training.[25]
The labiomental angle is the soft tissue convexity between the lower lip and chin. Chin structure may be classified based on convexity, a feature directly related to the labiomental angle. Convex, vertical, and posteriorly angled chins can support larger implant sizes. Vertical chins require about 8 mm implants. Posteriorly angled chins require the greatest augmentation—12 mm or more.[26] Horizontal growth patterns are associated with well-developed chins and a deep labiomental groove. Providers should not augment the thickest point of a convex labiomental angle with an implant larger than 4 mm.
Facial implants may also augment the posterior mandible in the transverse dimension. The bigonial width is the distance between the right and left mandibles' most inferior, lateral, and posterior edges. Farkas described the average bigonial widths of female and male individuals of Caucasian descent in relation to their bizygomatic width. The male bigonial width was found to be 34 mm shorter than their bizygomatic width. In contrast, the female bigonial width was found to be 36 mm shorter than their bizygomatic width.
Various soft tissue analyses target midfacial deficiencies. However, midfacial evaluation with cephalograms remains challenging. Powell stated that the malar eminence positioned at the FH plane is the most ideal aesthetically, with the malar eminence's location being 2 to 2.5 cm lateral to the lateral canthus. Meanwhile, Bell used the malar eminence's relation to the eye's cornea to determine their ideal positions. Bell stated that the eminence should be anterior to the cornea by 4 to 8 mm. Frey noted that among white individuals, the malar eminence is about 2 mm anterior to the cornea.[27] The Hinderer point, the malar region's most prominent aspect, is about 15 to 20 mm inferior and 10 mm lateral to the lateral canthus.[28]
Binder classified midfacial deficiencies into 3 categories:
- Type 1 deficiency involves a loss of malar projection secondary to skeletal hypoplasia
- Type 2 deficiency involves a loss of submalar soft tissue volume and is the most common type
- Type 3 deficiency is a combination of types 1 and 2
Each of these types warrants a different implant shape and location. Type 1 deficiency may be enhanced by a malar shell implant to increase projection and lateralization. Type 2 can improve with a submalar implant placed below the zygoma on the anterior maxilla. Type 3 may require a larger, combined implant.
Technique or Treatment
Antibiotics are essential for facial implant success. Broad-spectrum antimicrobials are routinely given preoperatively, intraoperatively, and postoperatively. Prophylactic cefazolin is a common choice for extraoral incisions to cover skin flora, including Staphylococcus species. Simultaneous administration of amoxicillin or other 3rd-generation penicillins helps cover oral gram-positive aerobes and anaerobes during intraoral incisions.[29] Ampicillin-sulbactam and cefazolin can serve as intraoperative replacements.[30] Postoperative antibiotics are controversial. Consensus is lacking regarding the timing of administration if postoperative antimicrobials are prescribed.[31]
The surgical team completes preparing the face with iodine sterilization followed by a local anesthetic injection. The anesthesia level varies. Implants are routinely placed under IV sedation or general anesthesia. The provider must consider the dissection approach to determine the anesthetic depth required for the procedure. Some anesthetic techniques are more time-intensive than others. Some procedures, like malar implant surgeries with a transconjunctival approach, may warrant paralytic administration. Other anesthetic considerations include general anesthesia costs and provider experience.
Malar implants are routinely inserted via an intraoral incision. An incision is made 0.5 to 1.0 cm above the gingival margin within the mucosa, posterior to the canine fossa. Blunt dissection with a periosteal elevator is then carried out subperiosteally posterolaterally along the anterior maxilla. Dissection proceeds superiorly to the infraorbital rim, identifying and protecting the infraorbital neurovascular bundle. Adequate dissection is essential for larger implants that may infringe upon the infraorbital foramen.
With type 2 and 3 defects, dissection is carried laterally to the masseteric tendon to allow passive seating in the submalar region. Dissection should exceed the implant size. Providers should use implant sizers to confirm the correct size and dissection. Sizers are implant manufacturer-specific and can be ordered separately or as part of a package. A 3D steriolith is a printed 3D model of the patient's face (see Image. Silicone Malar Implants). Providers may use it to visualize the correct implant size and aid in trimming. Implants and sizers are soaked in antibiotics before use. The dissection pocket is also rinsed with antibiotics before insertion. Sizers confirm the correct esthetic outcome and implant size and also ensure that the dissection is adequate.
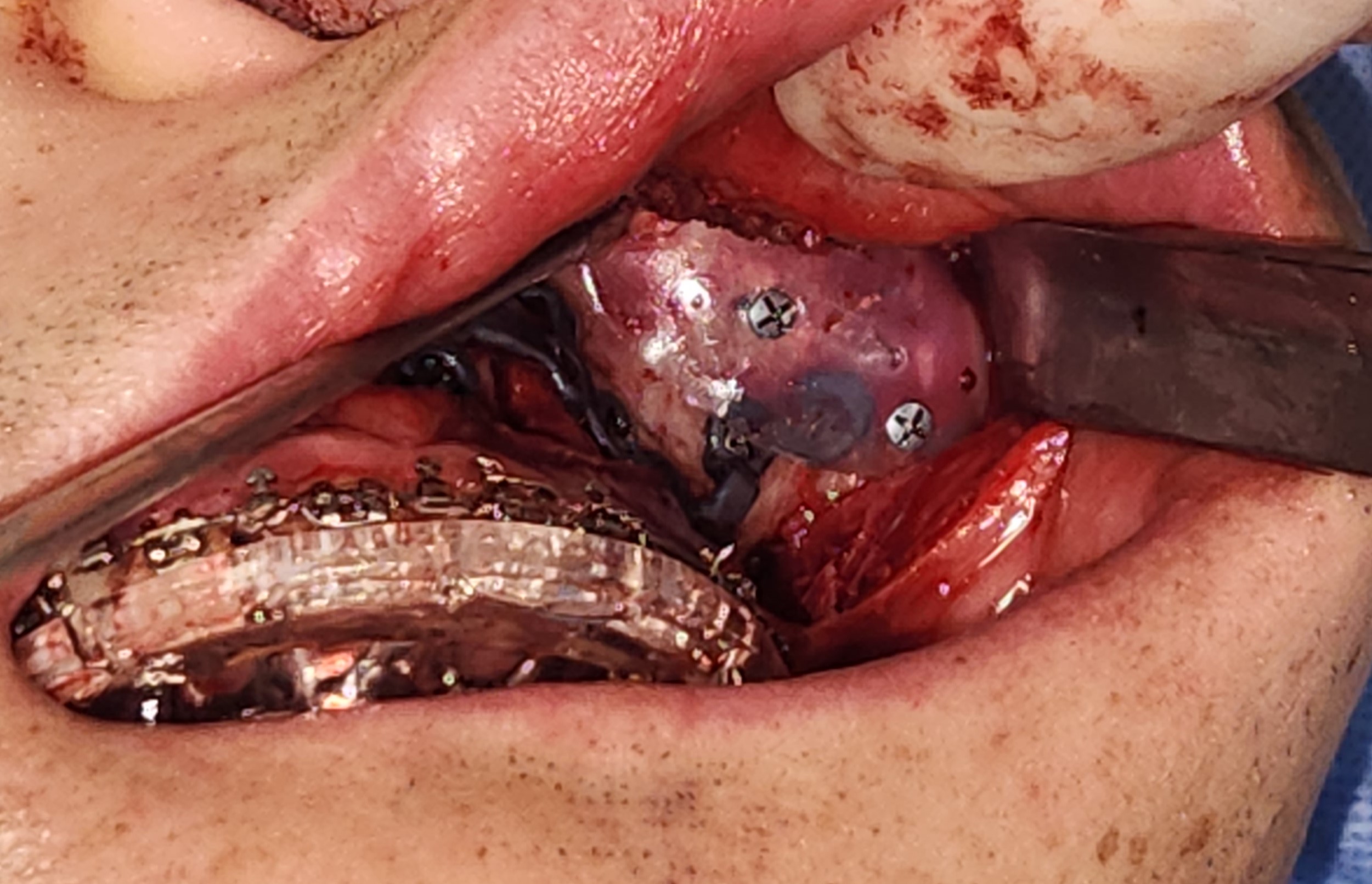
The implant is inserted carefully to limit folding and improve facial symmetry. Nonresorbable sutures or titanium screws secure the implant (see Image. Malar Implant). The incision is then closed, and the compressive wrap is placed to help compress any dead space created during surgery. Various compressive therapies are available. An elastic compressive head wrap is a noninvasive type generally worn continuously for the first 7 days after showering. After the 1st week, the dressing is worn only during sleep. Lymphatic drainage improves, and swelling subsides while the area is relieved of compression.[32]
Cheek bolsters, which consist of cotton rolls fixated with transcutaneous sutures, allow for more invasive malar implant placement. Bolsters permit firm and constant compression and are easily removed 1 to 2 days postsurgery. The periosteum and bone will reapproximate within 24 to 48 hours.
Chin implants are inserted either intraorally or submentally. An intraoral incision is made in the anterior mandibular vestibule, spanning from canine to canine. The incision is made with a blade or bovie electrocautery device through the mucosa until the mentalis muscle is visualized. The muscle bellies can be cut with a bovie electrocautery device, scissors, or a blade. A cuff of mentalis muscle should be left attached to the mandible and lip.
Muscle tissue on opposing sides of the incision will help reapproximation and prevent ptosis. The mandible is exposed using blunt subperiosteal dissection. Dissection should extend laterally along the mandible's inferior border before proceeding superiorly to identify the mental foramen and nerve (see Image. Mentalis Dissection). Dissection proceeds from the symphysis' inferior border and then superiorly to just beyond the planned implant size's border. Dissection should be larger than the planned implant size to avoid complications such as implant migration, symmetry, and soft tissue compression.
Sizers are placed to confirm dissection and implant size adequacy, serving as guides to avoid injuring the mental nerve. Aufricht retractors help improve visualization and protect the nerve if lateral dissection is inadequate. The surgical site is irrigated in the same manner as previously discussed. The implant is secured using either a nonresorbable suture or a titanium tacking screw. Layered closure is then performed. The mentalis muscle layer is closed first, completed by reapproximating the opposing cuffs using 2 to 4 3-0 Vicryl single interrupted sutures. The mucosa is then reapproximated using a faster resorbing suture like a 3-0 chromic gut.
Subperiosteal dissection exposes the mandibular angles and ramus to the sigmoid notch. A pterygomasseteric-sling release allows titanium mesh implant placement on the inferior and posterior mandibular border. Monocortical titanium screws fixate the implant, and the dissection is closed in layers.
Mandibular angle implants may be inserted via an intraoral or extraoral incision, depending on the implant type and size. A 1.5 cm intraoral incision lateral to the external oblique ridge is made above the depth of the vestibule. Subperiosteal dissection exposes the mandibular angle and ramus to the sigmoid notch. Soft tissue is then stripped from the anterior, inferior, lateral, and posterior aspects of the mandible and the pterygomasseteric sling. The pterygomasseteric sling is released to place titanium mesh implants on the inferior and posterior mandibular borders.
Monocortical titanium screws fixate the implant, and the dissection is closed in layers. The mandibular nerve is identified and protected if a nonmaleable implant is placed and a larger incision is needed. A transcutaneous incision lateral to the implant facilitates the use of a trocar system to anchor the implant to the lateral ramus and body with titanium monocortical screws. Securing the implant decreases dead space and allows for predictable augmentation volumes. Layered closure using resorbable sutures decreases infection and scar formation risk.
Close follow-up is essential to detecting and treating early or late complications.[33] A soft-food diet is recommended for posterior mandibular augmentation, which requires mastication muscle stripping.
Complications
Facial implant complications may occur early during recovery or months to years after placement. The definition of "early" and "late" varies between research studies. For this activity, "early" refers to the first few weeks of soft-tissue healing.[34] Complications may include the following.
- Hematoma
- Seroma
- Infection
- Wound dehiscence
- Alveolar ridge resorption
- Poor or undesired aesthetic outcome
- Displacement or malpositioning
- Scarring
- Nerve injury
Bleeding is an early complication and may result in an expanding hematoma requiring drainage. This complication is secondary to poor hemostasis during surgery. Seromas are also reported after implant placement, arising from inadvertent local gland dissection or the body's inflammatory response to the implant or surgical manipulation. A conservative dissection can help prevent fluid collection. Treatment options include observation with or without antibiotic administration, fluid drainage, and follow-up surgery for bleeding control.
Late complications include infection, mobilization, extrusion, and bone resorption. Stringer reported an infection risk of 0.7% to 14.6% for alloplastic facial implants. Infection occurrence ranged from 0.9% to 12.5%. For silicone implants, the infection rate has been reported to be as low as 1%.
Intraoral incisions help avoid visible scars. The infection rate may increase with these incisions, but this view is controversial. Nevertheless, the implant must be removed if an infection develops and persists despite antibiotic therapy.
The risk of bony erosion occurs more frequently with solid implants than with porous implants. The erosion depth increases as the implant size increases or becomes more rigid.[35] Theories as to why bony erosion occurs include mobility, inflammation, and stress on the overlying soft tissue.
Improper implant size, shape, or placement can result in lip incompetence. For chin implants, active engagement of the mentalis muscle, which strains to compensate for weakness, increases pressure on the underlying implant. Placing the implant at the inferior mandibular border where the cortex is thicker and further from the mentalis insertion has been shown to cause less resorption. Implant fixation helps eliminate micro-movements that can contribute to continual erosion. Although controversial, erosion has been reported to be self-limiting. Fixation is assumed to play a role in self-limiting erosion.
Esthetic asymmetry can occur from implant folding or migration from poor fixation, above-periosteum placement, or dissection-size inadequacy. Sizers can help with proper implant sizing when used before final implant placement. Poor placement or displacement is corrected with a second operation to secure the implant at the proper position or replace it with a more appropriately sized and shaped implant.
Another cause of poor cosmesis is poor mentalis muscle reapproximation. The mentalis muscle is encountered and incised with an intraoral approach in chin implant procedures. The mentalis originates from the mandibular incisive fossa and inserts on the chin's dermis. The mentalis elevates the chin. Poor dissection, incision, and reapproximation techniques may result in ptosis or "witch's chin." An extraoral incision eliminates the risk of mentalis ptosis. However, this incision can create an extraoral scar at the submental fold.
Dysesthesia, hypoesthesia, and anesthesia can occur if the mental nerve is damaged. The mental nerve supplies sensation to the ipsilateral chin and lower lip. This nerve must be identified and protected during chin augmentation. Mental nerve injury has been reported to occur in 2.4% of cases, often secondary to alveolar ridge resorption. The implant may be removed or exchanged for a better-fitting prosthesis if nerve dysfunction persists.
Clinical Significance
Facial implant surgery is highly versatile and offers an alternative to more invasive procedures, such as genial horizontal osteotomies. Less invasive procedures generally reduce costs using inexpensive hardware and anesthetic alternatives and incur less surgical time. Facial implant procedures are routinely performed under general anesthesia and intravenous sedation. However, awake implant placements under local anesthesia may also be performed. A 2014 UCLA research revealed that operating room costs could reach $35 per minute.[36] Alternative anesthetics reduce general anesthetic risk and monetary constraints for individuals who want to undergo facial implant surgery but have health and monetary restrictions. Patient recovery after implant placement is based on soft-tissue healing and requires only a few weeks. In contrast, bony surgery requires a significantly longer period to be considered stable.
Chin implants can increase the chin's projection both laterally and anteriorly. Chin implants may also be placed to make the chin look narrow. These implants can provide a more balanced facial appearance without the need for osteotomies. Malar implants increase midfacial projection, making the face appear more harmonious and youthful.
Angle implants can provide a better-defined jawline and widen the lower face. An increased bigonial width, ie, a wider jaw, may be created by implant placement in patients needing posttraumatic jaw reconstruction and facial growth abnormality correction. Individuals seeking a more masculine facial structure as part of gender affirmation surgery may also undergo mandibular angle implant surgery. Implants can enhance the aging face, which loses volume and skeletal support in 3 dimensions.
Given the proper training and practice, facial implant placement can be a safe and quick procedure. Whether a patient is seeking facial harmonization, a more youthful appearance, or a facial structure that aligns with their gender identity, facial implant surgery gives patients an alternative option to more extensive surgeries. This procedure also allows interprofessional teams like otorhinolaryngology and anesthesia to come together for gender-affirmation surgeries.
Enhancing Healthcare Team Outcomes
An interprofessional approach enhances facial implant surgery outcomes. The primary care or cosmetic physician first recognizes the problem and refers the patient to the appropriate surgeon. Specialists who can perform the procedure include plastic and maxillofacial surgeons and otolaryngologists. Once evaluated by the surgeon, active patient participation throughout the planning, surgical, and recovery stages is essential to ensure the procedure's success.
In outpatient settings, local anesthesia may be given by the surgical specialist if an awake procedure is preferred. The anesthesiologist lends expertise if the patient requires deep anesthesia or more complex pain management techniques like nerve blocks, whether in an in-hospital or outpatient setting. The nurse assists the surgeon during the procedure, monitors the patient while recovering from anesthesia, administers medications, and reinforces patient education. The collaborative approach helps ensure patient safety and high-quality care.
The Food and Drug Administration closely monitors implantable medical devices, but the range of FDA-approved materials is ever-growing. The team must inform the patient of the risks of using the selected implantable device. For instance, silicone materials show no increase in reactive oxygen species or genotoxicity but may cause bony erosion when placed on the chin, as previously mentioned.[37]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
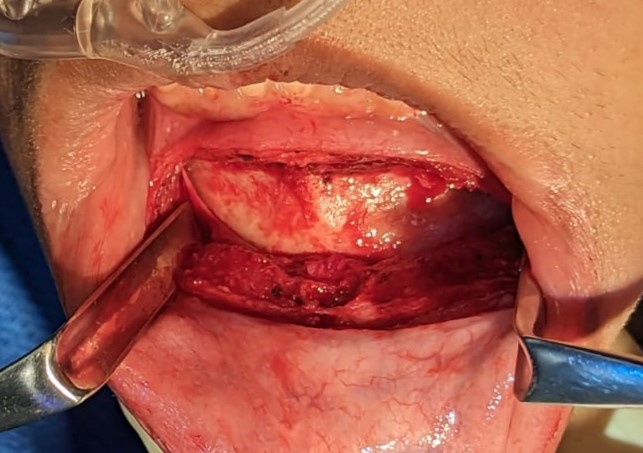
Mentalis Dissection. Dissection carried out to bone for future implant placement. Two Aufrich retractors are used to expose the lateral extend of the dissection. Both bellies of the mentalis muscle are visible, bisected with cuffs present on both on the inferior and superior aspects of the incision.
Contributed by Kevin Smith, DDS
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Binder WJ, Azizzadeh B. Malar and submalar augmentation. Facial plastic surgery clinics of North America. 2008 Feb:16(1):11-32, v [PubMed PMID: 18063245]
Cuzalina LA, Hlavacek MR. Complications of facial implants. Oral and maxillofacial surgery clinics of North America. 2009 Feb:21(1):91-104, vi-vii. doi: 10.1016/j.coms.2008.10.009. Epub [PubMed PMID: 19185798]
Lutz JC, Assouline Vitale LS, Graillon N, Foletti JM, Schouman T. Standard and Customized Alloplastic Facial Implants Refining Orthognathic Surgery: Outcome Evaluation. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2020 Oct:78(10):1832.e1-1832.e12. doi: 10.1016/j.joms.2020.05.009. Epub 2020 May 15 [PubMed PMID: 32574606]
Niamtu J 3rd. Essentials of cheek and midface implants. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2010 Jun:68(6):1420-9. doi: 10.1016/j.joms.2009.12.004. Epub 2010 Apr 9 [PubMed PMID: 20381942]
Romano N, Federici M, Castaldi A. Imaging of cranial nerves: a pictorial overview. Insights into imaging. 2019 Mar 15:10(1):33. doi: 10.1186/s13244-019-0719-5. Epub 2019 Mar 15 [PubMed PMID: 30877408]
Level 3 (low-level) evidenceHazani R, Rao A, Ford R, Yaremchuk MJ, Wilhelmi BJ. The safe zone for placement of chin implants. Plastic and reconstructive surgery. 2013 Apr:131(4):869-872. doi: 10.1097/PRS.0b013e3182818e6c. Epub [PubMed PMID: 23542258]
Hu KS, Yun HS, Hur MS, Kwon HJ, Abe S, Kim HJ. Branching patterns and intraosseous course of the mental nerve. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2007 Nov:65(11):2288-94 [PubMed PMID: 17954327]
Azizzadeh B, Mashkevich G. Nerve injuries and treatment in facial cosmetic surgery. Oral and maxillofacial surgery clinics of North America. 2009 Feb:21(1):23-9, v. doi: 10.1016/j.coms.2008.10.003. Epub [PubMed PMID: 19185792]
Mendelson B, Wong CH. Changes in the facial skeleton with aging: implications and clinical applications in facial rejuvenation. Aesthetic plastic surgery. 2012 Aug:36(4):753-60. doi: 10.1007/s00266-012-9904-3. Epub 2012 May 12 [PubMed PMID: 22580543]
Fattahi T. The prejowl sulcus: an important consideration in lower face rejuvenation. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2008 Feb:66(2):355-8. doi: 10.1016/j.joms.2006.11.032. Epub [PubMed PMID: 18201622]
Cronin RJ Jr, Oesterle LJ, Ranly DM. Mandibular implants and the growing patient. The International journal of oral & maxillofacial implants. 1994 Jan-Feb:9(1):55-62 [PubMed PMID: 8150513]
Op Heij DG, Opdebeeck H, van Steenberghe D, Quirynen M. Age as compromising factor for implant insertion. Periodontology 2000. 2003:33():172-84 [PubMed PMID: 12950850]
Yaremchuk MJ. Mandibular augmentation. Plastic and reconstructive surgery. 2000 Sep:106(3):697-706 [PubMed PMID: 10987481]
Birgfeld C, Heike C. Craniofacial Microsomia. Clinics in plastic surgery. 2019 Apr:46(2):207-221. doi: 10.1016/j.cps.2018.12.001. Epub [PubMed PMID: 30851752]
Schwaiger M, Echlin K, Atherton D, Haers P. The use of Medpor implants for midface contouring in cleft patients. International journal of oral and maxillofacial surgery. 2019 Sep:48(9):1177-1184. doi: 10.1016/j.ijom.2019.02.008. Epub 2019 Mar 11 [PubMed PMID: 30871847]
Aarts BE, Convens J, Bronkhorst EM, Kuijpers-Jagtman AM, Fudalej PS. Cessation of facial growth in subjects with short, average, and long facial types - Implications for the timing of implant placement. Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2015 Dec:43(10):2106-11. doi: 10.1016/j.jcms.2015.10.013. Epub 2015 Oct 23 [PubMed PMID: 26548528]
Hardin AM, Knigge RP, Oh HS, Valiathan M, Duren DL, McNulty KP, Middleton KM, Sherwood RJ. Estimating Craniofacial Growth Cessation: Comparison of Asymptote- and Rate-Based Methods. The Cleft palate-craniofacial journal : official publication of the American Cleft Palate-Craniofacial Association. 2022 Feb:59(2):230-238. doi: 10.1177/10556656211002675. Epub 2021 May 17 [PubMed PMID: 33998905]
Stringer D, Brown B. Correction of mandibular asymmetry using angled titanium mesh. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2009 Aug:67(8):1619-27. doi: 10.1016/j.joms.2008.12.068. Epub [PubMed PMID: 19615573]
Level 3 (low-level) evidenceMaas CS, Merwin GE, Wilson J, Frey MD, Maves MD. Comparison of biomaterials for facial bone augmentation. Archives of otolaryngology--head & neck surgery. 1990 May:116(5):551-6 [PubMed PMID: 2158331]
Level 3 (low-level) evidenceOliveira RV, de Souza Nunes LS, Filho HN, de Andrade Holgado L, Ribeiro DA, Matsumoto MA. Fibrovascularization and osteogenesis in high-density porous polyethylene implants. The Journal of craniofacial surgery. 2009 Jul:20(4):1120-4. doi: 10.1097/SCS.0b013e3181abb4ab. Epub [PubMed PMID: 19553849]
Level 3 (low-level) evidenceRomo T 3rd, Lanson BG. Chin augmentation. Facial plastic surgery clinics of North America. 2008 Feb:16(1):69-77, vi [PubMed PMID: 18063247]
Danieletto-Zanna CF, Ferreira GZ, Ferreira O, Pavan AJ, Camarini ET. Infected Silicone Chin Implant After Implant-Supported Jaw Rehabilitation: Case Report and Literature Review. The Journal of oral implantology. 2022 Aug 1:48(4):307-311. doi: 10.1563/aaid-joi-D-20-00112. Epub [PubMed PMID: 34091685]
Level 3 (low-level) evidenceRowe P, Koller A, Sharma S. Physiology, Bone Remodeling. StatPearls. 2024 Jan:(): [PubMed PMID: 29763038]
Frodel JL, Lee S. The use of high-density polyethylene implants in facial deformities. Archives of otolaryngology--head & neck surgery. 1998 Nov:124(11):1219-23 [PubMed PMID: 9821923]
Level 3 (low-level) evidenceNaini FB, Donaldson AN, McDonald F, Cobourne MT. Assessing the influence of chin prominence on perceived attractiveness in the orthognathic patient, clinician and layperson. International journal of oral and maxillofacial surgery. 2012 Jul:41(7):839-46. doi: 10.1016/j.ijom.2012.01.012. Epub 2012 Feb 15 [PubMed PMID: 22340990]
Fanous N, Yoskovitch A. Estimating implant size in chin augmentation: A simplified approach. The Canadian journal of plastic surgery = Journal canadien de chirurgie plastique. 2003 Fall:11(3):161-5 [PubMed PMID: 24115862]
Doddamani GM,Swathi PV,Tan KFH, Assessment of anterior malar projection using visual photographs and lateral cephalograms: A comparative study. Journal of orthodontic science. 2018; [PubMed PMID: 30271760]
Level 2 (mid-level) evidenceHinderer UT. Malar implants for improvement of the facial appearance. Plastic and reconstructive surgery. 1975 Aug:56(2):157-65 [PubMed PMID: 1096196]
Caruso SR, Yamaguchi E, Portnof JE. Update on Antimicrobial Therapy in Management of Acute Odontogenic Infection in Oral and Maxillofacial Surgery. Oral and maxillofacial surgery clinics of North America. 2022 Feb:34(1):169-177. doi: 10.1016/j.coms.2021.08.005. Epub 2021 Oct 30 [PubMed PMID: 34728145]
Khorasani M, Janbaz P, Rayati F. Maxillofacial reconstruction with Medpor porous polyethylene implant: a case series study. Journal of the Korean Association of Oral and Maxillofacial Surgeons. 2018 Jun:44(3):128-135. doi: 10.5125/jkaoms.2018.44.3.128. Epub 2018 Jun 26 [PubMed PMID: 29963494]
Level 2 (mid-level) evidenceOranges CM, Grufman V, di Summa PG, Fritsche E, Kalbermatten DF. Chin Augmentation Techniques: A Systematic Review. Plastic and reconstructive surgery. 2023 May 1:151(5):758e-771e. doi: 10.1097/PRS.0000000000010079. Epub 2022 Dec 20 [PubMed PMID: 36729154]
Level 1 (high-level) evidenceWang MW, Rodman RE. Gender Facial Affirmation Surgery; Techniques for Feminizing the Chin. Facial plastic surgery clinics of North America. 2023 Aug:31(3):419-431. doi: 10.1016/j.fsc.2023.04.006. Epub [PubMed PMID: 37348985]
Al-Jandan B, Marei HF. Mandibular angle augmentation using solid silicone implants. Dental and medical problems. 2018 Oct-Dec:55(4):367-370. doi: 10.17219/dmp/99531. Epub [PubMed PMID: 30648361]
Rojas YA, Sinnott C, Colasante C, Samas J, Reish RG. Facial Implants: Controversies and Criticism. A Comprehensive Review of the Current Literature. Plastic and reconstructive surgery. 2018 Oct:142(4):991-999. doi: 10.1097/PRS.0000000000004765. Epub [PubMed PMID: 29994843]
Guyuron B. MOC-PS(SM) CME article: genioplasty. Plastic and reconstructive surgery. 2008 Apr:121(4 Suppl):1-7. doi: 10.1097/01.prs.0000305931.98111.c3. Epub [PubMed PMID: 18379385]
Childers CP, Maggard-Gibbons M. Understanding Costs of Care in the Operating Room. JAMA surgery. 2018 Apr 18:153(4):e176233. doi: 10.1001/jamasurg.2017.6233. Epub 2018 Apr 18 [PubMed PMID: 29490366]
Level 3 (low-level) evidenceVijayalakshmi P, Geetha CS, Mohanan PV. Assessment of oxidative stress and chromosomal aberration inducing potential of three medical grade silicone polymer materials. Journal of biomaterials applications. 2013 Feb:27(6):763-72. doi: 10.1177/0885328211426353. Epub 2011 Nov 15 [PubMed PMID: 22090429]
Level 3 (low-level) evidence