Epidemiologic and Etiologic Considerations of Obesity
Epidemiologic and Etiologic Considerations of Obesity
Introduction
For much of the twentieth century, cigarette smoking was the most common preventable cause of morbidity and mortality. However, there has been a paradoxical decrease in tobacco use and a subsequent increase in obesity.[1] In simple terms, obesity occurs when caloric intake exceeds energy expenditure.[2] This chronic and often progressive condition is debilitating and has far-reaching implications extending far beyond the afflicted and into society.[3] The causes of obesity involve genetics, socioeconomic, diet, physical activity, medications, medical conditions, and culture.[4]
Genome-wide databases have identified more than 500 specific gene loci related to the development of obesity. Those genes can have profound lifelong implications (e.g., Prader-Willi syndrome, Bardet-Biedl syndrome).[5] Researchers have discovered racial disparities in the development of obesity. Various prenatal/childhood factors and normal aging has an association with the development of adult obesity. In addition, those with sedentary lifestyles tend to make poor choices in food selection and adopt a daily caloric intake that does not match their energy expenditure. As a result, this caloric excess is the primary driver in the development of obesity.[6]
Health professionals should be aware of various medications known to cause obesity. In addition, various medical conditions affecting the hypothalamic-pituitary axis (HPA) can contribute to obesity onset. Recently, investigators have become interested in the role of the gut microbiome in the development of obesity, particularly in the proportion of two-bacterial strains (Bacteriodes and Firmicutes) in the gut microbiome and the role of endocrine-disrupting chemicals.[7][8][9]
Finally, the development of chronic obesity produces a cascade of downstream molecular targets leading to the development of dyslipidemia, hypertension, and diabetes. This unique cluster of conditions in conjunction with obesity has been coined metabolic syndrome and substantially increases morbidity and mortality.[10]
The above-reviewed factors are quintessential to understanding how to treat this chronic disease. Previously, healthcare professionals have struggled with understanding these known causes of obesity. These deficiencies have led to missed opportunities and failure to educate patients on up-to-date treatment options for chronic obesity.[11]
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
Historically, malnourishment was considered the most pressing medical problem in society. Fortunately, social programs, charitable organizations, improved technology, and increased availability of pre-packaged foods in developed societies have made nutrition readily accessible. Notwithstanding, the relative improvement of availability has ushered in a fundamental shift in population health, replacing caloric deficit with caloric excess.[12]
We now see increased body mass index (BMI), expanding waistlines, and an increasing prevalence of comorbid chronic medical conditions led by obesity. Obesity is considered a multifactorial, progressive, and chronic systemic medical problem which can often be complex and relatively difficult to treat.
From a clinical perspective, patients are aware of their need to lose weight and have likely been told by previous healthcare providers to "take charge" of their weight loss. Unfortunately, there have been little-to-no non-surgical strategies to ensure successful and sustainable weight loss until recently. Emerging research has reinforced that the simplest way to ensure successful weight loss over the long term is a graded caloric restriction strategy and physical exercise deployed over several months using monitored compliance. Fundamentally, humans are "creatures of habit." Breaking the reward-feedback loop associated with eating is paramount to controlling dietary habits.[13]
Achieving this control requires understanding the complex behavioral elements of obesity. One must first begin at the molecular level by discussing how food becomes storable energy and how storable energy becomes fat.
Molecular and Physiological Processes Associated With Fat Storage and Energy Utilization
Food consumption must undergo a rigorous and elaborate digestion process to break down into nutrients used for essential bodily functions. At its core, the fundamental building blocks for all cells in our body rely on fats, carbohydrates, and proteins, which we collectively call macronutrients (macros).
Simplistically put, digestion exists in 3-phases: the cephalic phase, the gastric phase, and the intestinal phase. These phases have complex stimulatory/activating and inhibitory hormones that work together to achieve proper food degradation.
In the cephalic phase, sight, smell, and the mere thought of food activate an innate biological reflex. The oral cavity is the location for the mechanical and early enzymatic breakdown of food. The cephalic phase activates salivary glands to produce saliva, which contains lingual lipase and amylase, beginning the process of digestion. This reflex response is triggered by the cerebral cortex acting on the hypothalamus and medulla oblongata, sending signals to the vagus nerve to stimulate gastric juices. This action of pre-signaling will activate and prime the gastrointestinal tract in preparation for the meal. The gastric phase begins upon entry of masticated food into the stomach.
A feedback loop is activated when stretch receptors within the stomach activate a vaso-vagal reflex to trigger the vagus nerve, further stimulating gastric secretory activity. The gastric lumen is an intricate set of epithelial cells with specific secretory activity. These cells protect the stomach lining and assist in secreting enzymes to aid digestion. The intestinal phase arrives when partially digested foods mixed with gastric juices enter the small intestine, where the systemic absorption of macronutrients begins.[14][15][16]
The outlined digestion process breaks down carbohydrates starting in the mouth to their absorbable form (monosaccharides) in the small intestine. Fats become reduced to fatty acid chains and monoglycerides by bile salts secreted from the liver and lipase from the pancreas. Finally, protein is broken down into amino acids by pepsin released from the stomach and various other protein degrading enzymes released from the pancreas.[17]
The fate of monosaccharides, fatty acids, and amino acids depends on the person's energy requirements; if one is in the fed state, the metabolic pathway shifts towards energy storage. Conversely, the metabolic pathway shifts towards oxidizing macronutrients for immediate energy consumption if in the fasting state. Through differing metabolic pathways, monosaccharides, fatty acids, and amino acids can produce acetyl-CoA, which can enter the Kreb cycle and eventually generate energy through oxidative phosphorylation via the electron transport chain in the form of ATP.
Glycogen, primarily stored in the liver, can readily raise serum glucose through glycogenolysis. However, the glycogen storage used is depleted within 12 to 18 hours while in the fasting state. Due to this limitation, the liver possesses the tools to convert non-carbohydrate precursors into glucose, called gluconeogenesis. This process can take place in the liver or cortex of the kidneys and can use precursors such as glycerol (from fatty acids), lactate (from anaerobic metabolism), and glutamine/alanine.[18]
The entire process outlined above works through a delicate balance of hormone regulation. Leptin is a hormone stored in fat cells, and ghrelin is stored in the enteroendocrine cells of the gastrointestinal tract. Leptin suppresses food intake and is considered anorexigenic. Ghrelin stimulates the hunger reflex centrally at the level of the hypothalamus and is deemed to be orexigenic. Ghrelin is believed to be the primary hormone responsible for ushering in the cephalic phase of digestion.
However, existing research has only begun to understand the complex role of these hormones in obesity. For example, subjects with obesity tend to have elevated leptin levels and reduced levels of ghrelin, which is paradoxical to our understanding of the function of these two hormones. However, similar to type 2 diabetes mellitus and insulin, it is postulated that patients with obesity are leptin resistant, but the precise mechanism of obesity induction is yet to be fully elucidated.[19] An intricate understanding of the above molecular and physiological responses is essential to treat this chronic disease properly.
Genetic Factors
The induction of obesity is multifactorial, drawing from genetic, environmental, behavioral, physiological, social, and cultural factors. The possibility of hereditary variables in persons with obesity has been shown by studies comparing adiposity in twins, adoptees, and their parents (biological vs. adoptive) and within families. Studies imply that 40 to 70% of an adult's BMI is inherited.[20][5]
Adolescents with one obese parent have a three- to a fourfold higher chance of becoming obese.[21] The risk of obesity is more than ten times higher if you have two obese biological parents. Unfortunately, even with the extensive composite data of obesity-related gene loci, clinical testing based solely on variations in gene loci currently cannot accurately predict obesity using genes alone.[5]
The single nucleotide polymorphisms (SNPs) in the fat mass and obesity-associated (FTO) gene (located on Chr. 16) are found to contribute to the development of diabetes indirectly.[20] In another specific condition, genomic imprinting can produce de novo deletions in paternally derived 15q11-q13, a condition known as Prader-Willi syndrome (PWS). In addition to a characteristic physical appearance, PWS patients suffer from hyperphagia leading to chronic energy intake/expenditure.[22]
Another gene commonly implicated in monogenic childhood obesity is the MC4R, which encodes the melanocortin-4 receptor. The MC4R gene is associated with hyperinsulinemia and increased weight gain in infancy.[23] Leptin, leptin receptor deficiencies, and proopiomelanocortin deficiency are the other genetic causes of obesity. Monogenetic obesity is often severe, manifests at a young age, and is frequently accompanied by other symptoms.
Socioeconomic and Environmental Factors
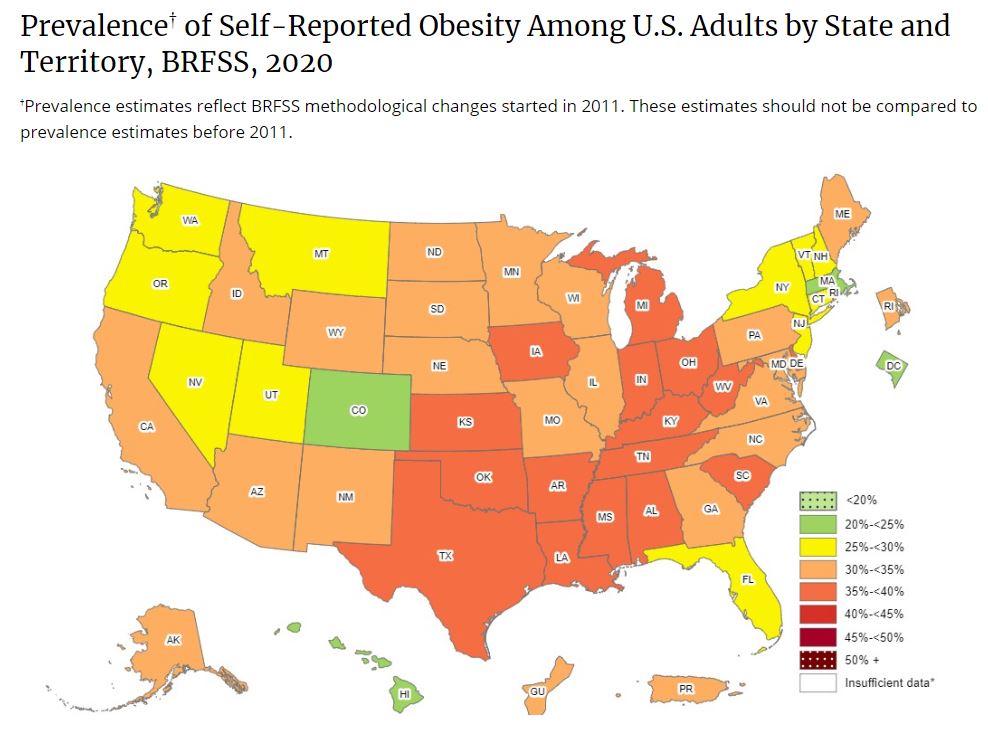
Epidemiological data has analyzed various geographical factors that may contribute to obesity. Social/cultural factors profoundly influence patients' dietary habits and behaviors. As a result, patients can often have an unhealthy understanding of a proper dietary regimen.
Obesity prevalence is lowest among individuals with the highest income and education, irrespective of race and ethnicity. In urban locations throughout the United States, a diet built entirely on fast-and-prepackaged foods is not uncommon. Much of the discrepancy can be due to the patient's lack of awareness of what foods contribute to chronic obesity.[24][25]
In addition, healthy food options are often cost-prohibitive in urban locations. Due to recent global events, the cost of groceries has sky-rocketed, worsening this disparity in healthy food availability. Low-to-middle income families will turn to cheaper calorie-dense and nutrient-poor options to make ends meet during difficult financial times. In combination with increased stress, socioeconomic factors will play a pivotal role in likely worsening the obesity pandemic across the globe. The worsening of obesity will exacerbate the high rate of chronic, obesity-related conditions, increasing the burden on our already stressed healthcare system.
Advertising that promotes obesity-inducing foods targets specific racial and socioeconomic groups differently. An isolated example of this effect was observed with outdoor food and beverage advertisement density in Sacramento, Los Angeles, New Orleans, Philadelphia, Austin, and New York. Geographical areas with low-income African-American and Latino populations were found to have a higher density of unhealthy food and beverage advertisements in those populations at the most significant risk for developing obesity.[26][27][28][29]
Another factor leading to the higher prevalence of obesity is the high cost of healthy food items. Thus the prevalence of obesity differs across US communities, in contrast to blacks, who had the greatest prevalence (50%) of obesity in the United States, and non-Hispanic Asian adults (17%) had the lowest prevalence.[30] This is probably tied to the social determinants of health, such as access to exercise, a wholesome diet, and general health information.
Obesity hypoventilation syndrome (Pickwickian syndrome) results from diminished ventilatory drive and capacity related to obesity. It is defined as the presence of awake alveolar hypoventilation characterized by daytime hypercapnia (arterial PaCO2 greater than 45mmHg). Its prevalence is largely unknown but based on previous studies and is estimated to be between 20 to 30% of obese patients.[31]
Prenatal and Childhood Factors
Childhood and infancy experiences may predispose to adult obesity. High maternal BMI, high gestational weight gain, gestational diabetes, and maternal type II diabetes may all predispose to adult obesity and metabolic disorders in offspring. By modifying gene expression, maternal obesity may influence the brain regions involved in body weight regulation.[32]
These epigenetic modifications, which may be the consequence of an increase in maternal nutrition supply to the developing fetus, promote increased hunger and fat accumulation in children. Children with obesity are five times more likely to be obese in adulthood.[33] This lends credibility to starting obesity-related prevention strategies earlier to reduce obesity prevalence in adulthood. Another area for improvement is by adding healthier school lunch options. A study using non-linear regression models found that children who attended public schools had a higher BMI regardless of socioeconomic status. Furthermore, those children eligible for free or reduced-cost lunch/breakfast had a higher BMI.[34]
Even though additional data is required to determine the impact of limiting the availability of nutrient-poor/high-sugar goods in schools on obesity, some studies have shown a net-positive result.[35][36][37]
Weight and Adulthood Factors
Between the ages of 20 and 65, most adults acquire weight steadily. Therefore, the probability of becoming overweight (BMI 25 kg/m^2) or obese (BMI 30 kg/m2) during one's lifetime is substantial. The energy imbalance responsible for the rise in obesity over the previous 30 years is estimated to be 100 kcal/day, illustrating that even a small daily positive energy balance may lead to clinically considerable weight gain over time. Weight rises until age 65. After that, the average weight loss is 0.65 kg/year.[38][39]
This is partly owing to a loss in muscle mass (sarcopenia), whereas fat mass increases throughout old age, resulting in a reduced correlation between BMI and fat mass.[40] Aging reduces resting and active energy expenditure and may also affect taste and smell, thus reducing food intake.
Dietary Factors
Over the last seventy years, there has been a major shift in the global food environment, with more people having access to processed, high-calorie foods. US Department of Agriculture (USDA) statistics on dietary energy supply shows that the average daily calorie consumption has risen from 2398 kcal/day/person in the 1970s to 2895 kcal/day/person in the 2000s. This increase in caloric consumption alone can explain the rise in obesity rates seen over this period.
Additionally, the USDA statistics show that Americans consume less fruit, vegetables, and dairy than is advised while consuming more fat, sugar, meats, and grains. The Western Diet is a colloquial term used to describe a diet high in processed foods, such as refined sugars and red meats, which may be excessively salty and sugary. This diet has been adopted primarily in America but has recently begun spreading into parts of Europe and Asia. In general, this diet type is associated with chronic inflammatory states, which are precursors to several chronic diseases such as diabetes, atherosclerosis, and chronic kidney disease.[41]
Eaton et al. described a 'discordance hypothesis' which postulates that the western diet is the primary driver of increasing BMIs due to a mismatch between calories consumed and calories burned.[42]
Hunter-gatherers in our primitive human species would expend a tremendous amount of calories hunting, transporting, and preparing food. However, in our society now, very little energy is expended procuring high-calorie foods, which contributes to our natural tendency to store adipose tissue.
Physical Activity Factors
Physical activity accounts for the greatest variation in total energy expenditure. Reduced regular physical activity and increased sedentary behavior have been linked to an increased risk of obesity.[43] The Amish community, with a low obesity rate, walks 14,000 to 18,000 steps per day, while the average American takes about 5,000 to 6,000 steps per day.[44]
Furthermore, occupational and physical activity has decreased in the United States during the last half-century. Half of the American workforce was fairly active in 1960, but by 2010, over 70 percent were either sedentary or reported little physical activity. This resulted in a decrease in work-related energy expenditure of 140 kcal/day for men and 120 kcal/day for females, which further explains the increasing prevalence of obesity. Adults with physical or mental disabilities are more likely to be obese; those with reduced lower-extremity mobility are at the greatest risk.
Sleep Factors
Epidemiological studies demonstrate substantial and persistent relationships between reduced nocturnal sleep duration, nightshift employment with the development of obesity, and other metabolic disorders.[45][46]
There has been an increase in nightshift employees who spend more time sedentary and less time physically active, resulting in decreased energy expenditure and an increase in the likelihood of obesity. Insufficient sleep also causes the activation of brain regions involved with food reward increasing food consumption, particularly high-fat meals. Thus, adequate sleep and sleep pattern are crucial for lowering adiposity as well as a number of other metabolic ailments.
Medical Factors
Hypothyroidism: Hypothyroidism causes weight gain by reducing basal metabolic rate, thus leading to increased adiposity; however, the weight gain is usually modest and improves with treatment.
Cushing syndrome: The increased levels of glucocorticoids in Cushing disease stimulate 11-beta-hydroxysteroid dehydrogenase type 1 in visceral fat and increase its lipogenic capability leading to adiposity. It is characterized by progressive central adiposity involving the trunk and abdomen, fat accumulation on the face and neck, and muscle wasting in the extremities. Cushing syndrome may result from the excess intake of steroids over a long period (iatrogenic/overdose).
Diabetes is often managed by the use of intensive insulin therapy and home glucose monitoring. Tight control of blood glucose is considered critical in preventing the vascular complications of the condition. However, insulin therapy itself is associated with weight gain.[47][48] It has been suggested that metformin may result in weight loss in patients with type2 diabetes. However, evidence is still lacking to establish this association.[49]
Hypothalamic obesity: Hypothalamic obesity is uncommon and may result from damage (tumor, irradiation, surgery, or elevated intracranial pressure) to the ventromedial or paraventricular area of the hypothalamus or the amygdala, which regulates metabolic information about nutrient storage and food availability. Damage to the ventromedial hypothalamus results in hyperphagia and decreased energy expenditure, leading to obesity. It might be associated with additional symptoms such as headache, nausea, or blurring of vision.[50]
Clinical Significance
Chronic obesity reverberates across many different areas of western society. Since 1970, there has been a nearly doubling incidence of obesity in the United States, reflecting more than two-thirds of Americans now being overweight. In 2008, the estimated cost of obesity was approximately 147 billion dollars annually, representing almost 10% of total healthcare-related spending.[51]
In 2021, that number substantially increased to approximately 260.6 billion dollars.[52] We now know that truncal (abdominal) obesity and increased adipose stores are primary risk factors for developing atherosclerosis, which increases morbidity and mortality from cardiovascular complications. An international classification of obesity exists, with an associated likelihood of morbidity.[53]
Classification of Overweight and Obesity Based on Body Mass Index[53]
|
Class |
Body Mass Index (kg/m2) |
Probability of associated comorbidities |
|
Normal Range |
18.5–24.99 |
Average |
|
Preobese |
25.00-29.99 |
Above-average |
|
Class I Obesity |
30.0–34.99 |
Moderate |
|
Class II Obesity |
35.0-39.99 |
High |
|
Class III Obesity |
>40 |
Very high |
Truncal obesity contributes to insulin resistance, the primary pathophysiological mechanism for developing type 2 diabetes mellitus. Over a century of research led to discovering a cluster of clinical features, coined in 1988 as metabolic syndrome, or dysmetabolic syndrome X, by Dr. Gerald M. Reaven. These features included elevated blood pressure, blood sugar, serum triglycerides, and low-density lipoprotein.[54]
Although being obese is not necessarily a direct causative factor in developing metabolic syndrome, weight loss can be the most beneficial lifestyle modification a person can make to reduce the risk of complications from metabolic syndrome.[55] The clinical classification of metabolic syndrome is debated, and five-known professional organizations have put out several evidence-based criteria to aid clinicians in arriving at this diagnosis. However, all five organizations have included truncal obesity as a potential risk factor.[56][57]
Patients with obesity have elevated cytokines such as tumor necrosis factor-alpha (TNF-alpha) and interleukin 1beta (IL-1beta), contributing to metabolic syndrome.[58][7] Chronic obesity is also a risk factor for the development of nonalcoholic fatty liver disease (NAFLD), leading to an increased risk of all-cause mortality.[56][59]
Understanding the multifactorial implications of obesity is paramount to accurately diagnosing and treating the condition. In evaluating a patient who demonstrates features of obesity, the first step is to determine whether the cause is predominately lifestyle or if the result of a secondary condition such as medication use.
One should determine if the patient is taking a medication known to cause obesity. Certain atypical antipsychotics like olanzapine, quetiapine, and risperidone have been shown to cause a net weight gain, with the most substantial weight gain observed with olanzapine. Anticonvulsant and mood stabilizer gabapentin is associated with a 2.2 kg (approximately 5 lb) weight gain within two months.
Also, exercise caution with hypoglycemic agents, particularly in the sulfonylurea class, due to known weight gain associated with tolbutamide (2.8 kg/6 lbs) and glimepiride (2.1 kg/5 lbs). Thiazolidinedione-type hypoglycemic agents have also shown a statistically significant weight gain, particularly pioglitazone (2.6 kg/5.5 lbs).[60]
According to Centers for Disease Control and Prevention (CDC) data, from 2015-2018, approximately 13.2% of adults were on some form of antidepressant medication, with women being the predominant gender receiving prescriptions within this class (17.7%).[61]
However, prescribers should be aware of the antidepressants amitryptiline and mirtazapine, which are associated with a 1.8 kg (4 lbs) and 1.5 kg (3.5 lbs) weight gain, respectively. Glucocorticoids are commonly prescribed in clinical practice for their potent anti-inflammatory effects, which can be useful for treating a broad range of acute and chronic conditions. Unfortunately, glucocorticoids' mechanism of action typically leads to an approximate 4 to 8% rise in weight gain.[62][60]
Enhancing Healthcare Team Outcomes
From a clinical perspective, understanding obesity has gone through a paradigm shift. Previously, clinicians would broadly interpret this disease process as a behavioral issue. The problem with this theory, it creates misplaced blame where the patient may feel inappropriately judged or stigmatized.
Now that we know obesity is a multifactorial disease process, we can build on our knowledge to empower patients to understand obesity through collaboration to explore options for reversing the disease course. It often necessitates a multidisciplinary approach focusing on gradual, sensible lifestyle modifications rather than abrupt weight loss or excessively short-term goals.
Physicians, dietitians, physical therapists, social workers, psychologists, and nurses must collaborate to manage this chronic illness and provide individualized patient care through their unique skills. The doctor is generally a patient's primary source of health information, and their guidance may promote patient motivation.
Routine doctor appointments often fail to address patients' concerns about weight, diet, and physical activity, which might alter the patient's perspective about these conditions. A brief 3-minute lifestyle interview may offer doctors an understanding of patients' eating habits, weight-loss motivation, and mental and physical difficulties.[63]
By stressing diet and obesity-related lifestyle variables, the doctor may urge patients to follow medical advice and consider obesity a serious but manageable health condition. Larger food portions are the main contributor to increased energy intake and obesity; thus, nutritionists may educate patients on the proper portion size, information about the calories and glycemic index in different food items, the unique calorie needs per physical effort, and misconceptions surrounding various fad diets through easy strategies and also to prevent feeling hungry, which may lead to binge eating.
Comprehensive weight reduction counseling must also include methods for both eating less and eating healthier. Patients who consume more low-fat, whole foods (such as fruits, vegetables, legumes, and whole grains) are more likely to consume more nutrients overall. The water content of fresh vegetables is very high, increasing weight and volume to maximize fullness without adding calories.
Diet and exercise together are the most effective obesity treatments. Physical therapists (PT) may urge patients to include non-exercise activity thermogenesis (NEAT), such as standing while using the phone and using stairs instead of elevators, as it can account for a 2,000 kcal difference per day in active vs. inactive adults.[64]
Walking can be a simple exercise, and PT can lead patients toward incremental, manageable objectives, such as adding one minute to a 10-minute walk, ascending one more flight of stairs, or adding 100 steps at a time to a day's total. The physical therapist's role is even more important for patients with musculoskeletal disorders; the therapist may instruct them in exercises that do not need great physical effort and can be as simple as rolling their legs while seated. Knee issues are most prevalent in obese patients; hence, therapists are of the utmost significance to increase physical activity among this patient group.
Numerous mental illnesses may cause weight gain and obesity because eating may be a coping mechanism for depression, despair, stress, and anxiety. Studies have shown that depression, in particular, can lead to unhealthy weight gain due to poor dietary and lifestyle choices, such as choosing to stay inactive out of a lack of motivation or consuming sweet or salty foods to feel good. Psychiatric problems and obesity may form a vicious cycle, with depression/anxiety leading to weight gain and vice versa.
Psychologists may play a crucial role in detecting and treating these underlying issues, and weight reduction can increase confidence and self-esteem substantially. A social worker may aid with allocating resources such as weight loss medications assistance, food stamps, enhancing mobility by supplying walkers and wheelchairs, and locating low-cost gym membership locations such as the YMCA and safe shelters. The nurse is the essential patient contact, may educate patients and follow up weekly in person or by phone to check patient's compliance, making her a crucial element of the multidisciplinary team.
Nursing, Allied Health, and Interprofessional Team Interventions
The roles of nursing, allied health, and interprofessional teams in healthcare in identifying obesity are vital to patient-centered care. As highlighted above, the strategies for reversing obesity in patients require routine follow-up and consistent evaluation by healthcare professionals. Once the plan is implemented and approved by the patient's clinician, support staff can perform routine follow-ups, monitor A1c every 3-months, lipid panel every 6-months, and assess patients' barriers to weight loss. Support staff can communicate the results to the physician to modify the plan to ensure the patient remains on track.
Patients suffering from chronic obesity can often have an unhealthy relationship with food. Cognitive-behavioral therapy (CBT) can be a valuable tool for helping patients reconcile feelings that may lead to overeating. Various technological applications exist to assist patients with direct access to a therapist.
The use of applications to measure daily body-weight and count calories is largely effective due to its ability to draw the users' attention to lifestyle-related details which influence weight gain and loss. For most, cataloging daily caloric intake can be burdensome and arduous, so it is crucial to consistently follow up with patients during their weight-loss journey.
Follow-up is the quintessential element of ensuring adherence to a weight-loss plan. Therefore, it is crucial to set expectations that this will require consistent virtual or in-person meetings to ensure continued compliance when beginning the weight loss journey. If the patient is unwilling to agree to follow-up, the patient will likely fail and revert to previous poor lifestyle choices.
Nursing, Allied Health, and Interprofessional Team Monitoring
Telehealth can be a valuable strategy for managing new patients to a lifestyle modification regimen. Quick face-to-face meetings with weight reporting can be a helpful tool for patients to benchmark their progress and find new motivation.
Media
(Click Image to Enlarge)
References
Flegal KM. The effects of changes in smoking prevalence on obesity prevalence in the United States. American journal of public health. 2007 Aug:97(8):1510-4 [PubMed PMID: 17600266]
Level 2 (mid-level) evidenceSchwartz MW, Seeley RJ, Zeltser LM, Drewnowski A, Ravussin E, Redman LM, Leibel RL. Obesity Pathogenesis: An Endocrine Society Scientific Statement. Endocrine reviews. 2017 Aug 1:38(4):267-296. doi: 10.1210/er.2017-00111. Epub [PubMed PMID: 28898979]
Cawley J, Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. Journal of health economics. 2012 Jan:31(1):219-30. doi: 10.1016/j.jhealeco.2011.10.003. Epub 2011 Oct 20 [PubMed PMID: 22094013]
Grundy SM, Multifactorial causation of obesity: implications for prevention. The American journal of clinical nutrition. 1998 Mar; [PubMed PMID: 9497171]
Loos RJ. The genetics of adiposity. Current opinion in genetics & development. 2018 Jun:50():86-95. doi: 10.1016/j.gde.2018.02.009. Epub 2018 Mar 9 [PubMed PMID: 29529423]
Level 3 (low-level) evidenceSwinburn B, Sacks G, Ravussin E. Increased food energy supply is more than sufficient to explain the US epidemic of obesity. The American journal of clinical nutrition. 2009 Dec:90(6):1453-6. doi: 10.3945/ajcn.2009.28595. Epub 2009 Oct 14 [PubMed PMID: 19828708]
Hardin BI, Keyes D. Enterohormonal and Microbiota Pathophysiology Of Obesity. StatPearls. 2023 Jan:(): [PubMed PMID: 35201732]
Maruvada P,Leone V,Kaplan LM,Chang EB, The Human Microbiome and Obesity: Moving beyond Associations. Cell host [PubMed PMID: 29120742]
Gore AC, Chappell VA, Fenton SE, Flaws JA, Nadal A, Prins GS, Toppari J, Zoeller RT. EDC-2: The Endocrine Society's Second Scientific Statement on Endocrine-Disrupting Chemicals. Endocrine reviews. 2015 Dec:36(6):E1-E150. doi: 10.1210/er.2015-1010. Epub 2015 Nov 6 [PubMed PMID: 26544531]
Kahn R, Buse J, Ferrannini E, Stern M, American Diabetes Association, European Association for the Study of Diabetes. The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes care. 2005 Sep:28(9):2289-304 [PubMed PMID: 16123508]
Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2015 Apr:16(4):319-26. doi: 10.1111/obr.12266. Epub 2015 Mar 5 [PubMed PMID: 25752756]
Level 2 (mid-level) evidenceEknoyan G, A history of obesity, or how what was good became ugly and then bad. Advances in chronic kidney disease. 2006 Oct; [PubMed PMID: 17045228]
Level 3 (low-level) evidenceLean M, Lara J, Hill JO. ABC of obesity. Strategies for preventing obesity. BMJ (Clinical research ed.). 2006 Nov 4:333(7575):959-62 [PubMed PMID: 17082548]
Zafra MA, Molina F, Puerto A. The neural/cephalic phase reflexes in the physiology of nutrition. Neuroscience and biobehavioral reviews. 2006:30(7):1032-44 [PubMed PMID: 16678262]
Patricia JJ, Dhamoon AS. Physiology, Digestion. StatPearls. 2023 Jan:(): [PubMed PMID: 31334962]
Forssell H. Gastric mucosal defence mechanisms: a brief review. Scandinavian journal of gastroenterology. Supplement. 1988:155():23-8 [PubMed PMID: 3072665]
Goodman BE. Insights into digestion and absorption of major nutrients in humans. Advances in physiology education. 2010 Jun:34(2):44-53. doi: 10.1152/advan.00094.2009. Epub [PubMed PMID: 20522896]
Level 3 (low-level) evidenceMelkonian EA, Asuka E, Schury MP. Physiology, Gluconeogenesis. StatPearls. 2023 Jan:(): [PubMed PMID: 31082163]
Klok MD, Jakobsdottir S, Drent ML. The role of leptin and ghrelin in the regulation of food intake and body weight in humans: a review. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2007 Jan:8(1):21-34 [PubMed PMID: 17212793]
Frayling TM, Timpson NJ, Weedon MN, Zeggini E, Freathy RM, Lindgren CM, Perry JR, Elliott KS, Lango H, Rayner NW, Shields B, Harries LW, Barrett JC, Ellard S, Groves CJ, Knight B, Patch AM, Ness AR, Ebrahim S, Lawlor DA, Ring SM, Ben-Shlomo Y, Jarvelin MR, Sovio U, Bennett AJ, Melzer D, Ferrucci L, Loos RJ, Barroso I, Wareham NJ, Karpe F, Owen KR, Cardon LR, Walker M, Hitman GA, Palmer CN, Doney AS, Morris AD, Smith GD, Hattersley AT, McCarthy MI. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science (New York, N.Y.). 2007 May 11:316(5826):889-94 [PubMed PMID: 17434869]
Level 2 (mid-level) evidenceWhitaker KL, Jarvis MJ, Beeken RJ, Boniface D, Wardle J. Comparing maternal and paternal intergenerational transmission of obesity risk in a large population-based sample. The American journal of clinical nutrition. 2010 Jun:91(6):1560-7. doi: 10.3945/ajcn.2009.28838. Epub 2010 Apr 7 [PubMed PMID: 20375189]
Level 2 (mid-level) evidenceButler MG. Prader-Willi Syndrome: Obesity due to Genomic Imprinting. Current genomics. 2011 May:12(3):204-15. doi: 10.2174/138920211795677877. Epub [PubMed PMID: 22043168]
Doulla M, McIntyre AD, Hegele RA, Gallego PH. A novel MC4R mutation associated with childhood-onset obesity: A case report. Paediatrics & child health. 2014 Dec:19(10):515-8 [PubMed PMID: 25587224]
Level 3 (low-level) evidenceOgden CL, Fakhouri TH, Carroll MD, Hales CM, Fryar CD, Li X, Freedman DS. Prevalence of Obesity Among Adults, by Household Income and Education - United States, 2011-2014. MMWR. Morbidity and mortality weekly report. 2017 Dec 22:66(50):1369-1373. doi: 10.15585/mmwr.mm6650a1. Epub 2017 Dec 22 [PubMed PMID: 29267260]
Caprio S, Daniels SR, Drewnowski A, Kaufman FR, Palinkas LA, Rosenbloom AL, Schwimmer JB. Influence of race, ethnicity, and culture on childhood obesity: implications for prevention and treatment: a consensus statement of Shaping America's Health and the Obesity Society. Diabetes care. 2008 Nov:31(11):2211-21. doi: 10.2337/dc08-9024. Epub [PubMed PMID: 18955718]
Level 3 (low-level) evidenceCassady DL, Liaw K, Miller LM. Disparities in Obesity-Related Outdoor Advertising by Neighborhood Income and Race. Journal of urban health : bulletin of the New York Academy of Medicine. 2015 Oct:92(5):835-42. doi: 10.1007/s11524-015-9980-1. Epub [PubMed PMID: 26337182]
Lesser LI, Zimmerman FJ, Cohen DA. Outdoor advertising, obesity, and soda consumption: a cross-sectional study. BMC public health. 2013 Jan 10:13():20. doi: 10.1186/1471-2458-13-20. Epub 2013 Jan 10 [PubMed PMID: 23305548]
Level 2 (mid-level) evidenceKwate NO, Lee TH. Ghettoizing outdoor advertising: disadvantage and ad panel density in black neighborhoods. Journal of urban health : bulletin of the New York Academy of Medicine. 2007 Jan:84(1):21-31 [PubMed PMID: 17146710]
Lowery BC, Sloane DC. The prevalence of harmful content on outdoor advertising in Los Angeles: land use, community characteristics, and the spatial inequality of a public health nuisance. American journal of public health. 2014 Apr:104(4):658-64. doi: 10.2105/AJPH.2013.301694. Epub 2014 Feb 13 [PubMed PMID: 24524512]
Level 2 (mid-level) evidenceHales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017-2018. NCHS data brief. 2020 Feb:(360):1-8 [PubMed PMID: 32487284]
Ghimire P, Sankari A, Kaul P. Pickwickian Syndrome. StatPearls. 2023 Jan:(): [PubMed PMID: 31194373]
Şanlı E, Kabaran S. Maternal Obesity, Maternal Overnutrition and Fetal Programming: Effects of Epigenetic Mechanisms on the Development of Metabolic Disorders. Current genomics. 2019 Sep:20(6):419-427. doi: 10.2174/1389202920666191030092225. Epub [PubMed PMID: 32476999]
Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2016 Feb:17(2):95-107. doi: 10.1111/obr.12334. Epub 2015 Dec 23 [PubMed PMID: 26696565]
Level 1 (high-level) evidenceLi J, Hooker NH. Childhood obesity and schools: evidence from the national survey of children's health. The Journal of school health. 2010 Feb:80(2):96-103. doi: 10.1111/j.1746-1561.2009.00471.x. Epub [PubMed PMID: 20236408]
Level 3 (low-level) evidenceTaber DR, Chriqui JF, Perna FM, Powell LM, Chaloupka FJ. Weight status among adolescents in States that govern competitive food nutrition content. Pediatrics. 2012 Sep:130(3):437-44. doi: 10.1542/peds.2011-3353. Epub 2012 Aug 13 [PubMed PMID: 22891223]
Fox MK, Gordon A, Nogales R, Wilson A. Availability and consumption of competitive foods in US public schools. Journal of the American Dietetic Association. 2009 Feb:109(2 Suppl):S57-66. doi: 10.1016/j.jada.2008.10.063. Epub [PubMed PMID: 19166673]
Level 2 (mid-level) evidenceSmith R, Kelly B, Yeatman H, Boyland E. Food Marketing Influences Children's Attitudes, Preferences and Consumption: A Systematic Critical Review. Nutrients. 2019 Apr 18:11(4):. doi: 10.3390/nu11040875. Epub 2019 Apr 18 [PubMed PMID: 31003489]
Level 1 (high-level) evidenceHill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science (New York, N.Y.). 2003 Feb 7:299(5608):853-5 [PubMed PMID: 12574618]
Yang YC, Walsh CE, Johnson MP, Belsky DW, Reason M, Curran P, Aiello AE, Chanti-Ketterl M, Harris KM. Life-course trajectories of body mass index from adolescence to old age: Racial and educational disparities. Proceedings of the National Academy of Sciences of the United States of America. 2021 Apr 27:118(17):. doi: 10.1073/pnas.2020167118. Epub [PubMed PMID: 33875595]
Batsis JA, Villareal DT. Sarcopenic obesity in older adults: aetiology, epidemiology and treatment strategies. Nature reviews. Endocrinology. 2018 Sep:14(9):513-537. doi: 10.1038/s41574-018-0062-9. Epub [PubMed PMID: 30065268]
Okręglicka K. Health effects of changes in the structure of dietary macronutrients intake in western societies. Roczniki Panstwowego Zakladu Higieny. 2015:66(2):97-105 [PubMed PMID: 26024397]
Eaton SB, Eaton SB 3rd, Konner MJ, Shostak M. An evolutionary perspective enhances understanding of human nutritional requirements. The Journal of nutrition. 1996 Jun:126(6):1732-40 [PubMed PMID: 8648449]
Level 3 (low-level) evidencePiercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, George SM, Olson RD. The Physical Activity Guidelines for Americans. JAMA. 2018 Nov 20:320(19):2020-2028. doi: 10.1001/jama.2018.14854. Epub [PubMed PMID: 30418471]
Roberts WC. The Amish, body weight, and exercise. The American journal of cardiology. 2004 Nov 1:94(9):1221 [PubMed PMID: 15518631]
McHill AW, Wright KP Jr. Role of sleep and circadian disruption on energy expenditure and in metabolic predisposition to human obesity and metabolic disease. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2017 Feb:18 Suppl 1():15-24. doi: 10.1111/obr.12503. Epub [PubMed PMID: 28164449]
Tse LA, Wang C, Rangarajan S, Liu Z, Teo K, Yusufali A, Avezum Á, Wielgosz A, Rosengren A, Kruger IM, Chifamba J, Calik KBT, Yeates K, Zatonska K, AlHabib KF, Yusoff K, Kaur M, Ismail N, Seron P, Lopez-Jaramillo P, Poirier P, Gupta R, Khatib R, Kelishadi R, Lear SA, Choudhury T, Mohan V, Li W, Yusuf S. Timing and Length of Nocturnal Sleep and Daytime Napping and Associations With Obesity Types in High-, Middle-, and Low-Income Countries. JAMA network open. 2021 Jun 1:4(6):e2113775. doi: 10.1001/jamanetworkopen.2021.13775. Epub 2021 Jun 1 [PubMed PMID: 34190997]
Heller S. Weight gain during insulin therapy in patients with type 2 diabetes mellitus. Diabetes research and clinical practice. 2004 Sep:65 Suppl 1():S23-7 [PubMed PMID: 15315867]
Purnell JQ, Zinman B, Brunzell JD, DCCT/EDIC Research Group. The effect of excess weight gain with intensive diabetes mellitus treatment on cardiovascular disease risk factors and atherosclerosis in type 1 diabetes mellitus: results from the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study (DCCT/EDIC) study. Circulation. 2013 Jan 15:127(2):180-7. doi: 10.1161/CIRCULATIONAHA.111.077487. Epub 2012 Dec 4 [PubMed PMID: 23212717]
Level 1 (high-level) evidenceApolzan JW, Venditti EM, Edelstein SL, Knowler WC, Dabelea D, Boyko EJ, Pi-Sunyer X, Kalyani RR, Franks PW, Srikanthan P, Gadde KM, Diabetes Prevention Program Research Group. Long-Term Weight Loss With Metformin or Lifestyle Intervention in the Diabetes Prevention Program Outcomes Study. Annals of internal medicine. 2019 May 21:170(10):682-690. doi: 10.7326/M18-1605. Epub 2019 Apr 23 [PubMed PMID: 31009939]
Holmer H, Pozarek G, Wirfält E, Popovic V, Ekman B, Björk J, Erfurth EM. Reduced energy expenditure and impaired feeding-related signals but not high energy intake reinforces hypothalamic obesity in adults with childhood onset craniopharyngioma. The Journal of clinical endocrinology and metabolism. 2010 Dec:95(12):5395-402. doi: 10.1210/jc.2010-0993. Epub 2010 Sep 8 [PubMed PMID: 20826582]
Hammond RA, Levine R. The economic impact of obesity in the United States. Diabetes, metabolic syndrome and obesity : targets and therapy. 2010 Aug 30:3():285-95. doi: 10.2147/DMSOTT.S7384. Epub 2010 Aug 30 [PubMed PMID: 21437097]
Cawley J, Biener A, Meyerhoefer C, Ding Y, Zvenyach T, Smolarz BG, Ramasamy A. Direct medical costs of obesity in the United States and the most populous states. Journal of managed care & specialty pharmacy. 2021 Mar:27(3):354-366. doi: 10.18553/jmcp.2021.20410. Epub 2021 Jan 20 [PubMed PMID: 33470881]
. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organization technical report series. 2000:894():i-xii, 1-253 [PubMed PMID: 11234459]
Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988 Dec:37(12):1595-607 [PubMed PMID: 3056758]
James PT, Rigby N, Leach R, International Obesity Task Force. The obesity epidemic, metabolic syndrome and future prevention strategies. European journal of cardiovascular prevention and rehabilitation : official journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology. 2004 Feb:11(1):3-8 [PubMed PMID: 15167200]
Quah YV Jr, Poh BK, Ismail MN. Metabolic Syndrome Based on IDF Criteria in a Sample of Normal Weight and Obese School Children. Malaysian journal of nutrition. 2010 Aug:16(2):207-17 [PubMed PMID: 22691926]
Parikh RM, Mohan V. Changing definitions of metabolic syndrome. Indian journal of endocrinology and metabolism. 2012 Jan:16(1):7-12. doi: 10.4103/2230-8210.91175. Epub [PubMed PMID: 22276247]
Sanz Y, Moya-Pérez A. Microbiota, inflammation and obesity. Advances in experimental medicine and biology. 2014:817():291-317. doi: 10.1007/978-1-4939-0897-4_14. Epub [PubMed PMID: 24997040]
Level 3 (low-level) evidencePolyzos SA, Kountouras J, Mantzoros CS. Obesity and nonalcoholic fatty liver disease: From pathophysiology to therapeutics. Metabolism: clinical and experimental. 2019 Mar:92():82-97. doi: 10.1016/j.metabol.2018.11.014. Epub 2018 Nov 29 [PubMed PMID: 30502373]
Domecq JP, Prutsky G, Leppin A, Sonbol MB, Altayar O, Undavalli C, Wang Z, Elraiyah T, Brito JP, Mauck KF, Lababidi MH, Prokop LJ, Asi N, Wei J, Fidahussein S, Montori VM, Murad MH. Clinical review: Drugs commonly associated with weight change: a systematic review and meta-analysis. The Journal of clinical endocrinology and metabolism. 2015 Feb:100(2):363-70. doi: 10.1210/jc.2014-3421. Epub 2015 Jan 15 [PubMed PMID: 25590213]
Level 1 (high-level) evidenceBrody DJ, Gu Q. Antidepressant Use Among Adults: United States, 2015-2018. NCHS data brief. 2020 Sep:(377):1-8 [PubMed PMID: 33054926]
Akalestou E, Genser L, Rutter GA. Glucocorticoid Metabolism in Obesity and Following Weight Loss. Frontiers in endocrinology. 2020:11():59. doi: 10.3389/fendo.2020.00059. Epub 2020 Feb 20 [PubMed PMID: 32153504]
Eckel RH, Preventive cardiology by lifestyle intervention: opportunity and/or challenge? Presidential address at the 2005 American Heart Association Scientific Sessions. Circulation. 2006 Jun 6; [PubMed PMID: 16754814]
Levine JA. Nonexercise activity thermogenesis--liberating the life-force. Journal of internal medicine. 2007 Sep:262(3):273-87 [PubMed PMID: 17697152]