Introduction
Corneal endotheliitis is defined as corneal endothelium-specific inflammation, which Khodadoust and Attarzadeh first described in 1982, characterized by corneal edema, keratic precipitates (KP), mild anterior chamber (AC) inflammation, and endothelial dysfunction. Based on the presentation of KP and pattern of the overlying stromal and epithelial edema, corneal endotheliitis can be classified into four types: linear, sectoral, disciform, and diffuse.[1]
Viruses including herpes simplex virus (HSV), varicella-zoster virus (VZV), or human herpesvirus 7 (HHV-7) have been reported in association with corneal endotheliitis. In 2006, Koizumi reported the first case of corneal endotheliitis caused by CMV.[2][3][4] CMV endotheliitis can present with linear or coin-shaped KP with or without cornea edema in immunocompetent individuals.[5][6] It may be accompanied by anterior uveitis and increased intraocular pressure (IOP).
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Human CMV, a ubiquitous lymphotropic herpes virus, has been increasingly recognized as one of the most common viruses causing corneal endotheliitis.[7][8] After Koizumi reported the first case of corneal endotheliitis in whom CMV DNA was detected in the aqueous humor, more evidence of CMV origin in corneal endotheliitis of CMV origin was provided by PCR.[9][10]
A higher CMV viral load in aqueous has been correlated with increased corneal endothelial cell loss and IOP elevation.[11][12] Studies have shown an association between CMV endotheliitis and previous corneal transplantation.[13][14]
Epidemiology
CMV seroprevalence is associated with ethnicity, age, and socioeconomic status, with rates varying from 50% in the United States and as high as 100% in countries in Africa, Asia, and South America.[15] Despite high worldwide seroprevalence, CMV endotheliitis has mainly been reported from Asian countries.[16]
The Japan Corneal Endotheliitis Study, the largest case series with 106 cases, reports that CMV endotheliitis is most common in middle-aged and older men (mean age of 66.9 years, 80.2% of men).[17]
Pathophysiology
The pathophysiology of CMV endotheliitis has yet to be fully elucidated. Suzuki and Ohashi have hypothesized that corneal endotheliitis is likely an anterior chamber-associated immune deviation (ACAID)-related disease. Latent CMV infection in the trabecular meshwork and the ciliary body becomes intermittently reactivated, and a small amount of virus may be released into the anterior chamber. Repeated releasing of the virus promotes ACAID against viral antigens. With the suppression of cell-mediated immunity, the virus can proliferate in the corneal endothelium. This theory is supported by a study of inducing ACAID against HSV in a rabbit model of herpetic corneal endotheliitis.[18]
History and Physical
Typically, CMV endotheliitis occurs in immunocompetent patients. The most common symptoms described by patients include photophobia and visual disturbances, usually in one eye. According to Japan Endotheliitis Study, almost half the patients had a previous history of anterior uveitis, Posner-Schlossman syndrome, or secondary glaucoma/ ocular hypertension. Also, more than half of patients had a prior history of corneal transplantation, glaucoma surgery, or cataract surgery.
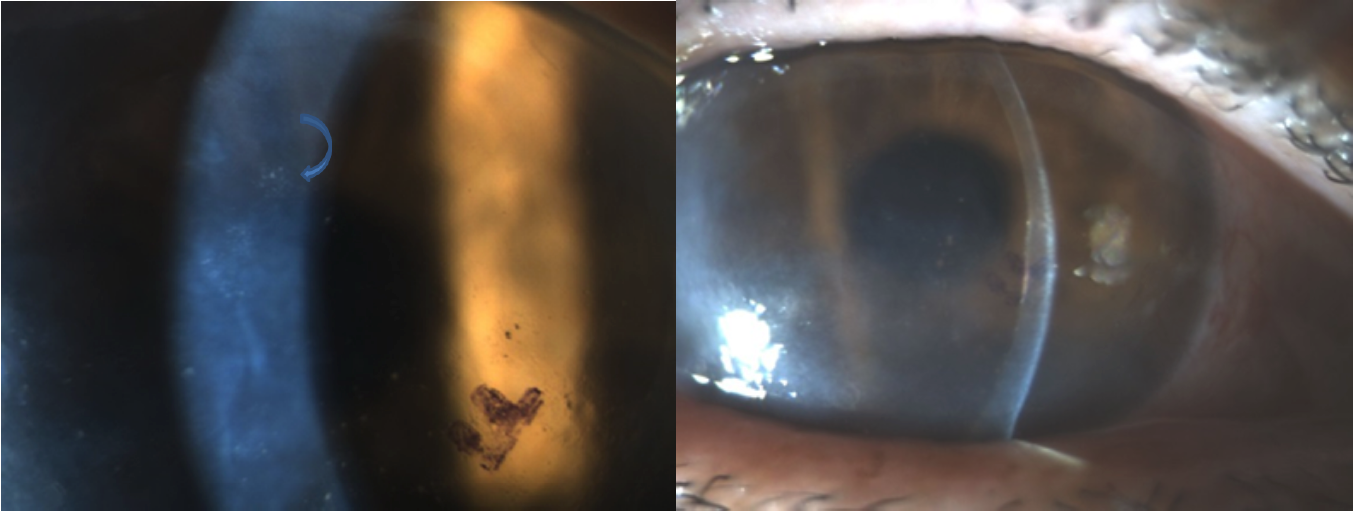
Physical findings include the presence of KP with overlying corneal edema, mild AC inflammation, ocular hypertension, limbal injection, peripheral anterior synechia, or pigmentation changes in the trabecular meshwork. Disc-shaped or Coin-shaped KPs are most common, observed in 70.6% of eyes in the Japan Endotheliitis study; the linear pattern was noted in 8.3% of eyes.[17]
Evaluation
Generally, corneal endotheliitis is a clinical diagnosis. Corneal endotheliitis with coin-shaped KPs and overlying corneal edema has a high positive predictive value (90.9%) for CMV endotheliitis.[19] Aqueous fluid can be tested for CMV DNA via qualitative or quantitative polymerase chain reaction (PCR). PCR is widely available and can provide a definitive diagnosis of CMV endotheliitis. PCR Multiplex testing for CMV, HSV, and VZV can be useful in guiding treatment.[20] Repeated aqueous tap may be considered should there be a high clinical suspicion with a negative PCR result.[21] Studies have shown a significant correlation between viral load and IOP elevation, recurrent inflammation, the presence of coin-shaped lesions, and corneal endothelial cell loss.[12]
Based on Japan Endotheliitis Study, typical CMV endotheliitis is diagnosed with corneal endotheliitis with a coin-shaped lesion or linear KPs similar to the rejection line, along with (+) CMV DNA but (-) HSV DNA and (-) VZV DNA; while atypical CMV endotheliitis is defined as corneal endotheliitis with localized corneal edema with KPs associated with two of the following signs including recurrent/chronic anterior uveitis, or ocular hypertension/ secondary glaucoma, or corneal endothelial cell loss, in the setting of (+) CMV DNA but (-) HSV DNA and (-) VZV DNA.[17]
CMV antibodies can also be measured by enzyme-linked immunoassay (ELISA). The Goldmann-Witmer coefficient (GWc), which is calculated as a titer of antibody in aqueous/titer of antibody in serum, multiplied by total serum globulins/total aqueous globulins, can be used to identify a causative agent.[22] It is suggestive of intraocular antibody production when the value exceeds three. A combination of these tests may have a clinical role since PCR test may only be positive during the active stage, and antibody testing can be positive at any point.[21]
In addition, non-invasive imaging tests, including anterior segment optical coherence tomography (ASOCT) and in vivo confocal microscopy (IVCM), can assist in diagnosis and monitoring disease progression. By using ASOCT, Kobayashi et al. demonstrated a saw-tooth appearance of protruding structures and high reflectivity of the posterior cornea in CMV endotheliitis, which decreased throughout the course of antiviral treatment. Hashida et al. demonstrated different patterns depending on the causative virus in ASOCT.[23][24]
A coin-shaped lesion in CMV endotheliitis presents with a quadrilateral and elliptical pattern, compared to HSV endotheliitis having small protrusion with low reflectivity and VZV endotheliitis with larger pigmented KP. Owl's eye morphological features detected with in-vivo confocal microscopy, which is considered to be pathognomonic for CMV endotheliitis, may be helpful as an adjunct. However, there is a report of Owl's eye morphology in HSV Keratitis and longstanding corneal grafts.[25][26][27]
Treatment / Management
The treatment of CMV endotheliitis should aim at both its infectious and inflammatory components. Anti-CMV treatment includes intravenous ganciclovir or oral valganciclovir, topical ganciclovir, or a combination of systemic and topical antiviral therapy. Ganciclovir and valganciclovir inhibit CMV's DNA polymerase and halt viral DNA replication. However, acyclovir and valacyclovir, which corneal specialists commonly use against HSV and HZV, are not effective in suppressing CMV, which does not utilize a viral thymidine kinase.[16] (B3)
Anti-inflammatory treatment with topical corticosteroids is usually combined with an anti-CMV regimen and should not be used alone. In the Japan Endotheliitis study, 104 of 109 eyes received either systemic anti-CMV (ganciclovir or valganciclovir), topical ganciclovir, or both.[28][29] Combined systemic and topical treatment was more effective in decreasing corneal edema and KPs, but there is no significant difference compared to systemic or topical treatment alone. Wong et al. summarized 12 case series and case reports in the management of CMV endotheliitis from January 2000 to January 2020.[30][31](B3)
There were 1 case report and 3 case series with a total of 32 eyes reporting good outcomes in the majority of patients receiving topical ganciclovir and topical prednisolone. Cases successfully treated with intravitreal ganciclovir injection have also been reported.[32][33](B3)
There is no consensus on an Anti-CMV regimen in managing CMV endotheliitis. The most commonly used regimen based on literature are:
- Systemic anti-CMV regimen: The first line is oral valganciclovir. The induction dose is 900 mg twice daily for 21 days with subsequent maintenance of 900 daily. Intravenous ganciclovir 5 mg/Kg twice daily for 21 days with subsequent maintenance of 5 mg/kg daily can be used if the patient failed oral valganciclovir.
- Topical ganciclovir 0.15% every 2 hours to 6 times a day, then taper to 3 to 4 times a day. Topical ganciclovir alone can be considered for mild CMV endotheliitis.[7]
- Stop maintenance of systemic treatment three months after clinical resolution but continue long-term topical ganciclovir for prophylaxis.
Management of CMV endotheliitis in the setting of corneal transplantation:
Following corneal transplantation, highly suspected CMV endotheliitis warrants prompt diagnosis with PCR analysis and anti-CMV treatment, usually oral valganciclovir with or without topical ganciclovir. Systemic or topical corticosteroids should be reduced as much as deemed safe in a given transplant. Treatment with therapeutic doses of oral valganciclovir is usually extended to 6 weeks to 3 months, followed by long-term maintenance with topical ganciclovir 0.15%.[34][35] More studies are required to evaluate optimal treatment regimens and the duration of maintenance therapy.(B3)
Topical ganciclovir or combined with a short-term oral valganciclovir for prophylaxis after keratoplasty in patients with a history of CMV infection has been reported, including a treatment failure that ended up doing better with the addition of systemic treatment.[36][37][38][39]
In the study by Koizumi et al., who evaluated the therapeutic efficacy of topical ganciclovir 0.15%, they detected ganciclovir in all aqueous humor samples. They concluded that a therapeutic level of ganciclovir concentration in the cornea was reached. Further studies are needed to determine whether topical ganciclovir alone is sufficient for prophylaxis. Still, it is an attractive treatment option considering the significant adverse effects, including pancytopenia and myelosuppression associated with systemic treatment.[40]
Aqueous tapping before or during the time of corneal transplantation to detect CMV could be beneficial for patients with a history of CMV infection or unclear reasons for endothelial failure, particularly in regions with high seroprevalence.
Differential Diagnosis
Endothelial dysfunction is caused by other herpes viruses, including HSV, VZV, mumps, Epstein Barr virus (EBV). HSV endotheliitis may present with linear or diffuse small to medium-sized pigmented KPs, VZV-related endotheliitis has diffuse medium to large-sized mutton-fat KPs, and EBV may have diffuse corneal edema and multiple fine KPs.[8] In general, PCR analysis for HSV, VZV, and CMV should be performed to make the diagnosis.
Inflammatory glaucomatous conditions including hypertensive anterior uveitis, Fuch Uveitis syndrome, Posner-Schlossman syndrome, previously presumed to be idiopathic, have been strongly linked to viral etiologies, including CMV infection.[41][42]
Corneal graft rejection in corneal transplantation patients: Differentiating CMV endotheliitis from corneal graft rejection remains challenging, especially with negative PCR analysis. Treatment for graft rejection may also reactivate latent CMV, exacerbate CMV endotheliitis, and worsen graft failure. Raised IOP, KPs, graft rejection not responding to steroid or unexplained sudden endothelial cell loss is more suggestive of CMV endotheliitis instead of allograft rejections.[34]
Prognosis
CMV endotheliitis has a relatively favorable prognosis if detected and treated early and effectively. However, recurrent episodes can occur, with progressively worse outcomes. Topical ganciclovir appears to help prevent a recurrence, but more studies are needed to evaluate optimal prophylaxis regimens.
Complications
CMV endotheliitis can cause irreversible endothelial dysfunction, vision loss, and secondary glaucoma. In the Japan Endotheliitis study, 60.6% of the eyes retained corneal clarity without additional corneal transplantation. Complications associated with systemic treatment such as pancytopenia and myelosuppression should be monitored periodically. Systematic treatment should be discontinued if pancytopenia or myelosuppression occurs.[17]
Deterrence and Patient Education
Patients should be educated that CMV endotheliitis can relapse. It is important to be compliant with treatment and self-monitor for symptoms such as blurry vision, red-eye, or photophobia. Delayed treatment and recurrent episodes can cause progressively worse outcomes. Patients should also be educated on the side effects of the anti-CMV regimen.
Enhancing Healthcare Team Outcomes
Management of CMV endotheliitis involves systemic anti-CMV treatment. It should involve an interprofessional healthcare team that includes infectious disease specialists and primary care clinicians, nurses, and pharmacists to optimize treatment and monitor adverse effects.
Media
References
Alfawaz A, Cytomegalovirus-related corneal endotheliitis: A review article. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2013 Jan; [PubMed PMID: 23964187]
Koizumi N,Yamasaki K,Kawasaki S,Sotozono C,Inatomi T,Mochida C,Kinoshita S, Cytomegalovirus in aqueous humor from an eye with corneal endotheliitis. American journal of ophthalmology. 2006 Mar; [PubMed PMID: 16490509]
Level 3 (low-level) evidenceBaltatzis S,Romero-Rangel T,Foster CS, Sectorial keratitis and uveitis: differential diagnosis. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2003 Jan; [PubMed PMID: 12545285]
Level 3 (low-level) evidenceOhashi Y,Yamamoto S,Nishida K,Okamoto S,Kinoshita S,Hayashi K,Manabe R, Demonstration of herpes simplex virus DNA in idiopathic corneal endotheliopathy. American journal of ophthalmology. 1991 Oct 15; [PubMed PMID: 1656756]
Level 3 (low-level) evidenceKhodabande A, Varicella endotheliitis: a case report. European journal of ophthalmology. 2009 Nov-Dec; [PubMed PMID: 19882562]
Level 3 (low-level) evidenceInoue T,Kandori M,Takamatsu F,Hori Y,Maeda N, Corneal endotheliitis with quantitative polymerase chain reaction positive for human herpesvirus 7. Archives of ophthalmology (Chicago, Ill. : 1960). 2010 Apr; [PubMed PMID: 20385952]
Level 3 (low-level) evidenceWong AHY,Kua WN,Young AL,Wan KH, Management of cytomegalovirus corneal endotheliitis. Eye and vision (London, England). 2021 Jan 14; [PubMed PMID: 33441165]
Moshirfar M,Murri MS,Shah TJ,Skanchy DF,Tuckfield JQ,Ronquillo YC,Birdsong OC,Hofstedt D,Hoopes PC, A Review of Corneal Endotheliitis and Endotheliopathy: Differential Diagnosis, Evaluation, and Treatment. Ophthalmology and therapy. 2019 Jun; [PubMed PMID: 30859513]
Chee SP,Bacsal K,Jap A,Se-Thoe SY,Cheng CL,Tan BH, Corneal endotheliitis associated with evidence of cytomegalovirus infection. Ophthalmology. 2007 Apr; [PubMed PMID: 17207531]
Level 2 (mid-level) evidenceKandori M,Inoue T,Takamatsu F,Kojima Y,Hori Y,Maeda N,Tano Y, Prevalence and features of keratitis with quantitative polymerase chain reaction positive for cytomegalovirus. Ophthalmology. 2010 Feb; [PubMed PMID: 19969369]
Level 2 (mid-level) evidenceMiyanaga M,Sugita S,Shimizu N,Morio T,Miyata K,Maruyama K,Kinoshita S,Mochizuki M, A significant association of viral loads with corneal endothelial cell damage in cytomegalovirus anterior uveitis. The British journal of ophthalmology. 2010 Mar; [PubMed PMID: 19734135]
Kandori M,Miyazaki D,Yakura K,Komatsu N,Touge C,Ishikura R,Inoue Y, Relationship between the number of cytomegalovirus in anterior chamber and severity of anterior segment inflammation. Japanese journal of ophthalmology. 2013 Nov; [PubMed PMID: 23928983]
Level 2 (mid-level) evidenceSuzuki T,Hara Y,Uno T,Ohashi Y, DNA of cytomegalovirus detected by PCR in aqueous of patient with corneal endotheliitis after penetrating keratoplasty. Cornea. 2007 Apr; [PubMed PMID: 17413969]
Level 3 (low-level) evidenceAnshu A,Chee SP,Mehta JS,Tan DT, Cytomegalovirus endotheliitis in Descemet's stripping endothelial keratoplasty. Ophthalmology. 2009 Apr; [PubMed PMID: 19195708]
Level 3 (low-level) evidenceAdland E,Klenerman P,Goulder P,Matthews PC, Ongoing burden of disease and mortality from HIV/CMV coinfection in Africa in the antiretroviral therapy era. Frontiers in microbiology. 2015; [PubMed PMID: 26441939]
Joye A,Gonzales JA, Ocular manifestations of cytomegalovirus in immunocompetent hosts. Current opinion in ophthalmology. 2018 Nov; [PubMed PMID: 30281031]
Level 3 (low-level) evidenceKoizumi N,Inatomi T,Suzuki T,Shiraishi A,Ohashi Y,Kandori M,Miyazaki D,Inoue Y,Soma T,Nishida K,Takase H,Sugita S,Mochizuki M,Kinoshita S,Japan Corneal Endotheliitis Study Group., Clinical features and management of cytomegalovirus corneal endotheliitis: analysis of 106 cases from the Japan corneal endotheliitis study. The British journal of ophthalmology. 2015 Jan; [PubMed PMID: 25075122]
Level 3 (low-level) evidenceZheng X,Yamaguchi M,Goto T,Okamoto S,Ohashi Y, Experimental corneal endotheliitis in rabbit. Investigative ophthalmology [PubMed PMID: 10670465]
Level 3 (low-level) evidenceHwang YS,Shen CR,Chang SH,Lai CC,Liu CL,Chen KJ,Lin KK,Chen TL,Hsiao CH, The validity of clinical feature profiles for cytomegaloviral anterior segment infection. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2011 Jan; [PubMed PMID: 20857136]
Level 2 (mid-level) evidenceMartín Ramírez A,Cardeñoso Domingo L,González Guijarro JJ, PCR Multiplex for CMV Detection in Patients with Anterior Uveitis. Ocular immunology and inflammation. 2019; [PubMed PMID: 29474137]
Relvas LJM,Antoun J,de Groot-Mijnes JDF,Motulsky E,Ten Dam-Van Loon NH,Makhoul D,Willermain F,Caspers L, Diagnosis of Cytomegalovirus Anterior Uveitis in Two European Referral Centers. Ocular immunology and inflammation. 2018; [PubMed PMID: 29377783]
De Groot-Mijnes JD,Rothova A,Van Loon AM,Schuller M,Ten Dam-Van Loon NH,De Boer JH,Schuurman R,Weersink AJ, Polymerase chain reaction and Goldmann-Witmer coefficient analysis are complimentary for the diagnosis of infectious uveitis. American journal of ophthalmology. 2006 Feb; [PubMed PMID: 16458686]
Level 3 (low-level) evidenceKobayashi R,Hashida N,Soma T,Koh S,Miki A,Usui S,Maeda N,Nishida K, Clinical Findings of Anterior Segment Spectral Domain Optical Coherence Tomography Images in Cytomegalovirus Corneal Endotheliitis. Cornea. 2017 Apr; [PubMed PMID: 27941387]
Hashida N,Asao K,Maruyama K,Nishida K, Cornea Findings of Spectral Domain Anterior Segment Optical Coherence Tomography in Uveitic Eyes of Various Etiologies. Cornea. 2019 Oct; [PubMed PMID: 31335529]
Hillenaar T,Weenen C,Wubbels RJ,Remeijer L, Endothelial involvement in herpes simplex virus keratitis: an in vivo confocal microscopy study. Ophthalmology. 2009 Nov; [PubMed PMID: 19744733]
Kobayashi A,Yokogawa H,Higashide T,Nitta K,Sugiyama K, Clinical significance of owl eye morphologic features by in vivo laser confocal microscopy in patients with cytomegalovirus corneal endotheliitis. American journal of ophthalmology. 2012 Mar; [PubMed PMID: 22030352]
Level 3 (low-level) evidenceYokogawa H,Kobayashi A,Sugiyama K, Mapping owl's eye cells of patients with cytomegalovirus corneal endotheliitis using in vivo laser confocal microscopy. Japanese journal of ophthalmology. 2013 Jan; [PubMed PMID: 23124832]
Level 3 (low-level) evidencePavan-Langston D,Welch CL,Zegans ME, Ganciclovir gel for cytomegalovirus keratouveitis. Ophthalmology. 2012 Nov; [PubMed PMID: 23122464]
Level 3 (low-level) evidenceFan NW,Chung YC,Liu YC,Liu CJ,Kuo YS,Lin PY, Long-Term Topical Ganciclovir and Corticosteroids Preserve Corneal Endothelial Function in Cytomegalovirus Corneal Endotheliitis. Cornea. 2016 May; [PubMed PMID: 26967107]
Hwang JH,Ha M,Park Y,Chung SH, The Effect of Topical Ganciclovir and Corticosteroid on Cytomegalovirus Corneal Endotheliitis in Korean Patients. Ocular immunology and inflammation. 2019; [PubMed PMID: 29953306]
Koizumi N,Miyazaki D,Inoue T,Ohtani F,Kandori-Inoue M,Inatomi T,Sotozono C,Nakagawa H,Horikiri T,Ueta M,Nakamura T,Inoue Y,Ohashi Y,Kinoshita S, The effect of topical application of 0.15% ganciclovir gel on cytomegalovirus corneal endotheliitis. The British journal of ophthalmology. 2017 Feb; [PubMed PMID: 27142389]
Choi WS,Cho JH,Kim HK,Kim HS,Shin YJ, A case of CMV endotheliitis treated with intravitreal ganciclovir injection. Korean journal of ophthalmology : KJO. 2013 Apr; [PubMed PMID: 23543604]
Level 3 (low-level) evidenceYu T,Peng RM,Xiao GG,Feng LN,Hong J, Clinical Evaluation of Intravitreal Injection of Ganciclovir in Refractory Corneal Endotheliitis. Ocular immunology and inflammation. 2020; [PubMed PMID: 30806530]
Tan TE,Tan DTH, Cytomegalovirus Corneal Endotheliitis After Descemet Membrane Endothelial Keratoplasty. Cornea. 2019 Apr; [PubMed PMID: 30614903]
Dockery PW,Joubert KP,Parker JS,Parker JS, Comment on: [PubMed PMID: 31498245]
Level 3 (low-level) evidenceHasan A,Quintero-Estades JA,Nataneli N, A Woman With Intraocular Inflammation After Descemet Membrane Endothelial Keratoplasty. JAMA ophthalmology. 2020 Sep 1; [PubMed PMID: 32729891]
Kitazawa K,Jongkhajornpong P,Inatomi T,Koizumi N,Kayukawa K,Wakimasu K,Sotozono C,Kinoshita S, Topical ganciclovir treatment post-Descemet's stripping automated endothelial keratoplasty for patients with bullous keratopathy induced by cytomegalovirus. The British journal of ophthalmology. 2018 Sep; [PubMed PMID: 29363530]
Basilious A,Chew HF, Topical Ganciclovir for Prophylaxis of Cytomegalovirus Endotheliitis in Endothelial Keratoplasty. Cornea. 2019 Jan; [PubMed PMID: 30379718]
Chew MC,Tan DT,Chee SP,Li L, Optimising graft survival in endothelial keratoplasty for endothelial failure secondary to cytomegalovirus endotheliitis. Journal of ophthalmic inflammation and infection. 2019 Aug 2; [PubMed PMID: 31375951]
Fellay J,Venetz JP,Aubert JD,Seydoux C,Pascual M,Meylan PR, Treatment of cytomegalovirus infection or disease in solid organ transplant recipients with valganciclovir. Transplantation proceedings. 2005 Mar; [PubMed PMID: 15848585]
Yoo WS,Kim GN,Chung I,Cho MC,Han YS,Kang SS,Yun SP,Seo SW,Kim SJ, Clinical characteristics and prognostic factors in hypertensive anterior uveitis diagnosed with polymerase chain reaction. Scientific reports. 2021 Apr 23; [PubMed PMID: 33893358]
Chee SP,Bacsal K,Jap A,Se-Thoe SY,Cheng CL,Tan BH, Clinical features of cytomegalovirus anterior uveitis in immunocompetent patients. American journal of ophthalmology. 2008 May; [PubMed PMID: 18255045]
Level 2 (mid-level) evidence