Introduction
Apraxia is the inability to perform skilled movements, whether they have been previously learned or can be immediately imitated by observing or carrying out the instructions of another individual.[1][2] Diagnosis involves ruling out weakness, sensory dysfunction, comprehension deficits, or incoordination as potential causes.[1][2][3] Initially, Hugo Karl Liepmann classified apraxia into 3 types—limb-kinetic, ideomotor, and ideational.[4] Liepmann's descriptions laid the groundwork for today's characterizations. However, the concept of apraxia now comprises a broader spectrum of subtypes compared to those originally identified by Liepmann. Broadly, apraxia can be classified based on specific tasks performed or general actions taken.[5] Unfortunately, the subtypes of apraxia are not defined consistently in the literature.[6]
Major forms of apraxia are listed below.
- General
- Ideational: Loss of neural encoding of the concept of a previously known skill
- Ideomotor: Impaired connection between the concept of a skill and its motor output
- Limb-kinetic: Loss of the motor output associated with a given skill
- Conceptual: Loss of ability to use tools
- Task-specific
- Speech
- Specific constructional: Difficulty in drawing, constructing, or copying
The term "ideational apraxia" is sometimes alternatively used to describe the loss of the ability to perform a sequence of movements. In contrast, "conceptual apraxia" refers to the loss of the concept itself.[2][6] However, a thorough discussion of usage differences is beyond the scope of this article.
Praxis, or the ability to carry out skilled actions, involves the activation or inhibition of neural networks in the brain. The type of apraxia manifested can vary depending on the involved neural network.[3] Apraxia can be diagnosed by performing a comprehensive examination on patients, which includes a detailed history, neurological examination, and apraxia-specific testing. However, consensus on the best operational practices for assessing apraxia does not exist.[1]
The management of apraxia involves addressing its underlying causes through physical, occupational, or other task-specific therapies, alongside counseling. Long-term outcomes depend on the type of apraxia and its effect on the patient's activities of daily living. Associated deficits can vary from acalculia, agraphia, and aphasia to confusion, social anxiety, and low self-esteem. Some individuals with apraxia may necessitate long-term assisted nursing care.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Some of the known causes of apraxia include:
- Stroke [7]
- Corticobasal syndrome [8]
- Alzheimer disease [9]
- Huntington disease
- Multiple sclerosis [10]
- Tumors [11]
- Creutzfeldt-Jakob disease [12]
- Schizophrenia
- Traumatic brain injury [13]
The risk of developing a specific form of apraxia depends on the risk of developing its associated etiological disorder.
Epidemiology
Apraxia is prevalent in approximately 50% to 80% of individuals with left hemisphere strokes, 30% to 50% with right hemisphere strokes, 19% to 45% with traumatic brain injuries, 25% with multiple sclerosis, and 90% with dementia.[14][15] However, population-level incidence and prevalence data for apraxia are unfortunately limited.
Pathophysiology
Praxis has various conceptual subdivisions. One example is its subdivision into the use of objects or tools and the performance of gestures, either by imitation or on command.[16] Although the neural networks subserving different types of praxis are nonidentical, specific brain structures, such as the left inferior parietal lobule and frontal motor areas, are involved in praxis and apraxias.[16][17][18][19]
A typical schema for the structures involved in praxis illustrates that praxis networks can be activated through visual, auditory, verbal, or tactile stimuli. The activated sensory modality provides information to neurons in the left parietal lobe, which selectively fires to commence the praxis process.[20][21] Subsequently, there is feedforward to the supplementary and premotor areas, where corresponding maps of coordinated movements are accessed. This information is sent to the primary motor cortex, which initiates the encoded motor programs by activating the musculature through the pyramidal tracts.[2]
Models of praxis and its associated networks are continually evolving. Additional structures are implicated, including the thalami, basal ganglia, prefrontal regions, temporal regions, and connecting white matter. Damage to these structures, which constitute the praxis networks, can result in apraxia, depending on the role of the damaged structure within its network.[2]
History and Physical
Evaluation of apraxia can begin after a comprehensive neurological examination, which excludes sensory, motor, and cognitive dysfunction as potential causes of the observed deficits. Before testing, the patient must first demonstrate an understanding of and ability to execute the tasks used for testing. Although there is no prescribed sequence for testing limbs, both sides should undergo evaluation.[2][22]
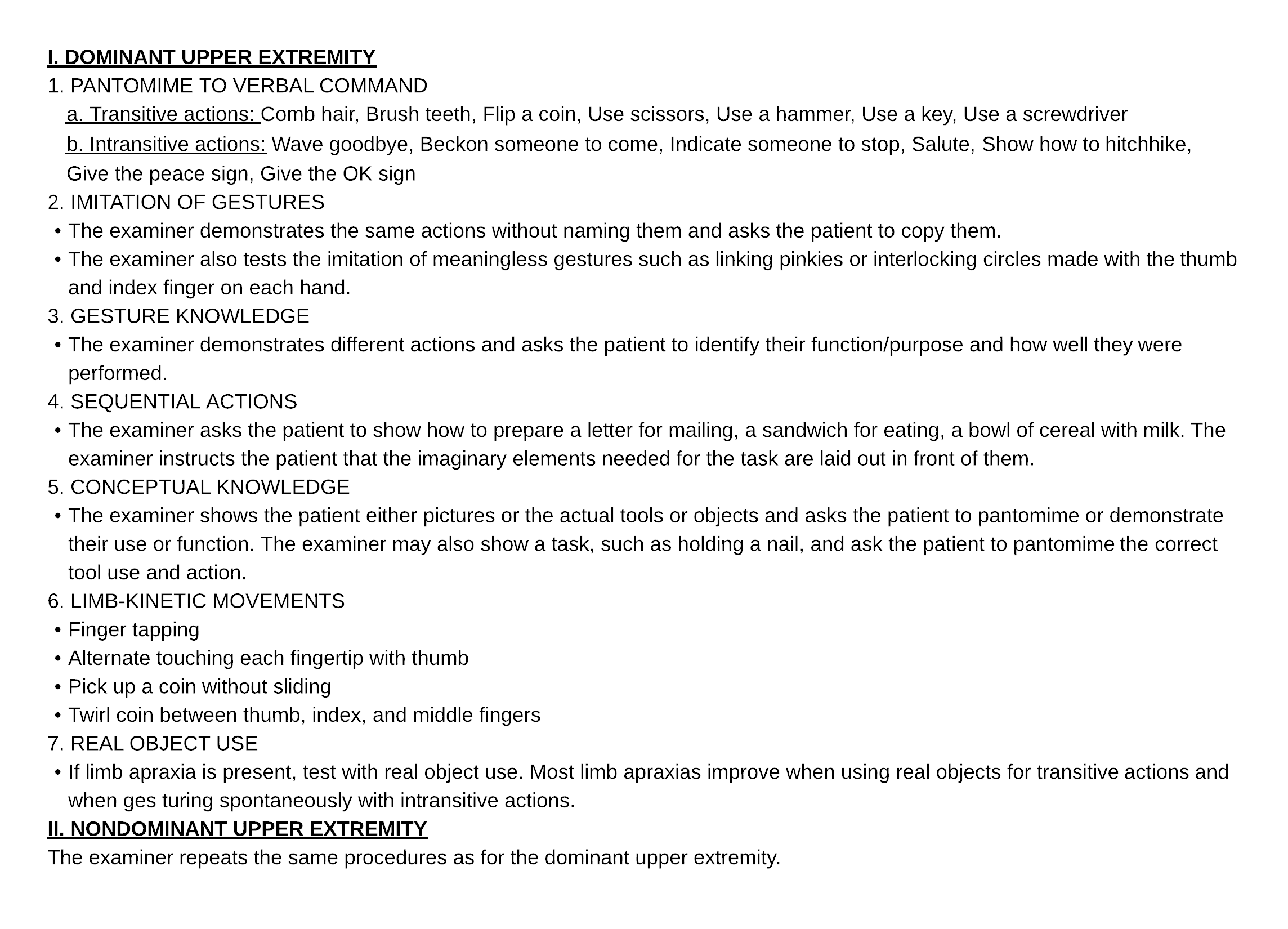
In general, 2 types of actions are assessed—those that are directly imitated and those that are recalled from memory. These actions can be further subdivided into 3 categories—intransitive gestures, transitive gestures, and pantomime of tool use. Intransitive gestures, also known as symbolic gestures, do not depend on using an object, such as saluting or waving goodbye. Transitive gestures involve using an object, such as swinging a hammer or flipping a coin. Pantomime involves mimicking or simulating the use of tools or objects without them being physically present. In addition, meaningless gestures, such as holding the thumb to the underside of the nose, can also be assessed (see Image. Examination of Limb Apraxia).[2][22]
Examples of abnormal findings associated with apraxia subtypes are listed below.[2]
- Ideomotor apraxia: Patients exhibit an inability to pantomime or imitate gestures. Moreover, they experience challenges with spatiotemporal orientation and positioning. Movements involving their fingers, hands, and arms display abnormal trajectories.
- Ideational apraxia: Patients struggle to identify the correct sequence of actions necessary to accomplish a task. Even when provided with a list of required steps, they may encounter difficulties organizing them accurately.
- Limb-kinetic apraxia: Patients exhibit incorrect fine motor actions, particularly with their hands, when attempting to perform a learned task. For instance, they may struggle with rotating a coin using their thumb, index finger, and middle finger.
- Conceptual apraxia: Patients face challenges identifying the appropriate tool for a given task. When presented with a tool, they may struggle to discern its purpose. Additionally, they may experience difficulty in pantomiming the correct utilization of a tool.
Formal testing tools for limb apraxia include the Florida Apraxia Battery–Extended and Revised Sydney (FABERS), the Apraxia Battery for Adults-2, the Short Screening Test for Ideomotor Apraxia (STIMA), the Cologne Apraxia Screening (KAS) or Revised Cologne Apraxia Screening (KAS-R), the Diagnostic Instrument for Limb Apraxia (DILA) or the Diagnostic Instrument for Limb Apraxia-Short Version (DILA-S), and the Test of Upper Limb Apraxia (TULIA).[23][24][25][26][27]
Evaluation
Thorough assessment methods, including detailed history-taking, physical examination, and neuropsychological testing, are used to identify and classify apraxia. Additional testing is used not to describe the apraxia further but to determine its etiology. Apraxia may develop acutely after a neurological insult such as stroke or traumatic brain injury. Alternatively, it may also be insidious, as observed in neurodegenerative disorders. Patients are often unaware of their inability to perform previously learned skills and activities.
Radiological and laboratory evaluation of apraxia can assist in uncovering etiologies associated with apraxia, including cerebrovascular disease, neurodegenerative disorders, traumatic brain injury, tumors, and multiple sclerosis. Imaging modalities such as magnetic resonance imaging (MRI) and positron emission tomography (PET) can identify associated brain lesions.
Treatment / Management
The primary treatment for apraxia involves focused rehabilitation utilizing various therapies such as occupational, speech, and physical, alongside addressing the underlying disorder. Apraxia can significantly impair independent functional capacity, with its presence often indicating the level of caregiver assistance needed post-stroke, while its absence may predict an early return to work.[28](B2)
Currently, a widely accepted treatment strategy for apraxia does not exist. The challenge of creating task-specific therapies with generalizable benefits is illustrated in the work of Buxbaum et al.[29] Rehabilitation is ideally initiated promptly following apraxia diagnosis, particularly in cases stemming from acute lesions.[30][31] Newer technologies, such as transcranial magnetic stimulation, have shown promise in treating apraxia.[32]
Differential Diagnosis
Several disorders related to movement or speech can be mistaken for apraxia, such as aphasia, nonapraxic dysarthria, alien limb phenomenon, akinesia, magnetic grasp, grope reflex, motor preservation, and motor impersistence.
Prognosis
Patients with apraxia can have significant issues with performing learned skills, which can profoundly affect their independence and ability to carry out activities of daily living. Appropriate safety precautions must be implemented with objects and activities in their surroundings that can cause potential injury. In cases where the inability to perform certain learned skills is debilitating, patients may require skilled nursing care. The eventual prognosis varies depending on the patient and the underlying etiological disease.
Complications
Potential sequelae of apraxia include:
- Inability to perform activities of daily living
- Failure to function properly at work
- Injury caused by improper tool use
- Social isolation
- Social anxiety
- Low self-esteem
Deterrence and Patient Education
The most common causes of apraxia include stroke, dementia, and traumatic brain injury. Apraxia is often a sign of a complex underlying neurological condition that poses challenges in its management. Education regarding modifiable risk factors should be prioritized whenever possible. Pharmacological interventions and lifestyle management addressing hypertension, diabetes mellitus, sleep apnea, atrial fibrillation, tobacco use, and alcohol consumption can contribute to better outcomes.
Regardless of the underlying causes, the inability to perform specific tasks due to apraxia can evoke frustration, potentially resulting in loss of capacity, diminished motivation, depression, and further deterioration of function. Educational resources, effective communication with caregivers, and counseling of family members can be crucial in establishing realistic expectations, understanding care goals, and anticipating the challenges in the recovery journey. Active participation by patients, caregivers, and family members can significantly facilitate the rehabilitation process.
Pearls and Other Issues
Key facts to keep in mind about apraxia include:
- Apraxia is a neurological disorder characterized by the inability to perform learned or purposeful movements.
- Types of apraxia include ideomotor, ideational, limb-kinetic, and conceptual forms.
- Common causes of apraxia include stroke, traumatic brain injury, dementia, neurodegenerative disorders, tumors, and schizophrenia.
- Although occupational, physical, and speech therapy may help improve functional impairments caused by apraxia, addressing the underlying cause is necessary.
- The prognosis depends on the underlying cause and promptness of intervention.
Enhancing Healthcare Team Outcomes
Apraxia poses a challenge for clinicians due to the complexity of its identification and testing. The presence of concurrent neurological and psychological factors can obscure symptoms. Causes of apraxia range from acute disorders such as stroke and traumatic brain injury to chronic conditions such as neurodegenerative illness or schizophrenia. Furthermore, it can be mistaken for neurological conditions such as aphasia, abulia, and limb akinesia.
The lack of broad consensus concerning screening and diagnosis can frustrate healthcare providers. However, a detailed history, physical examination, and targeted testing can facilitate early identification and management. Despite inconsistencies in subtype definitions, healthcare professionals prioritize a multidisciplinary approach to diagnosing and managing apraxia, emphasizing seamless communication and collaboration within the healthcare team, thereby gaining valuable insights into the complexities of diagnosing and managing the condition.
The involvement of multidisciplinary and interprofessional teams is paramount in managing apraxia to enhance patient outcomes. This team can include the patient, their family members, nurses, occupational therapists, physiotherapists, primary care physicians, radiologists, neurologists, physiatrists, psychiatrists, counselors, social workers, and case workers. Each healthcare team member should maintain open communication channels with the rest of the team and be responsible for maintaining accurate and detailed records of interactions, interventions, and testing. Such an interprofessional approach significantly enhances patient outcomes.
In both inpatient and outpatient settings, a primary care physician or neurologist can assess for apraxia through comprehensive examination and history-taking. Nurses caring for patients can identify deficiencies in limb function, tool usage knowledge, and general demeanor alterations. Family members can aid in identifying patient weaknesses while they undergo rehabilitation. Therapists can assist in improving limb function and help patients acquire new skills for limb and tool usage. Psychological support during the recovery and rehabilitation phases is vital for long-term patient well-being.
Establishing a supportive environment at home and work for the patient's condition can facilitate their recovery process. The long-term outcome depends on the etiology and duration of the illness. However, prompt identification and management of the condition by an interprofessional healthcare team can lead to an improved prognosis.
Media
References
Baumard J, Le Gall D. The challenge of apraxia: Toward an operational definition? Cortex; a journal devoted to the study of the nervous system and behavior. 2021 Aug:141():66-80. doi: 10.1016/j.cortex.2021.04.001. Epub 2021 Apr 23 [PubMed PMID: 34033988]
Heilman KM. Upper Limb Apraxia. Continuum (Minneapolis, Minn.). 2021 Dec 1:27(6):1602-1623. doi: 10.1212/CON.0000000000001014. Epub [PubMed PMID: 34881728]
Zadikoff C, Lang AE. Apraxia in movement disorders. Brain : a journal of neurology. 2005 Jul:128(Pt 7):1480-97 [PubMed PMID: 15930045]
Pearce JM. Hugo Karl Liepmann and apraxia. Clinical medicine (London, England). 2009 Oct:9(5):466-70 [PubMed PMID: 19886110]
Heilman KM. Apraxia. Continuum (Minneapolis, Minn.). 2010 Aug:16(4 Behavioral Neurology):86-98. doi: 10.1212/01.CON.0000368262.53662.08. Epub [PubMed PMID: 22810515]
Cassidy A. The clinical assessment of apraxia. Practical neurology. 2016 Aug:16(4):317-22. doi: 10.1136/practneurol-2015-001354. Epub 2016 Mar 16 [PubMed PMID: 26984951]
Donkervoort M, Dekker J, van den Ende E, Stehmann-Saris JC, Deelman BG. Prevalence of apraxia among patients with a first left hemisphere stroke in rehabilitation centres and nursing homes. Clinical rehabilitation. 2000 Apr:14(2):130-6 [PubMed PMID: 10763789]
McClain M, Foundas A. Apraxia. Current neurology and neuroscience reports. 2004 Nov:4(6):471-6 [PubMed PMID: 15509449]
Stamenova V, Roy EA, Black SE. A model-based approach to limb apraxia in Alzheimer's disease. Journal of neuropsychology. 2014 Sep:8(2):246-68. doi: 10.1111/jnp.12023. Epub 2013 Jun 17 [PubMed PMID: 23773829]
Rapaić D, Medenica V, Kozomara R, Ivanović L. Limb apraxia in multiple sclerosis. Vojnosanitetski pregled. 2014 Sep:71(9):821-7 [PubMed PMID: 25282779]
Liouta E, Stranjalis G, Kalyvas AV, Koutsarnakis C, Pantinaki S, Liakos F, Komaitis S, Stavrinou LC. Parietal association deficits in patients harboring parietal lobe gliomas: a prospective study. Journal of neurosurgery. 2018 May 4:130(3):773-779. doi: 10.3171/2017.12.JNS171799. Epub [PubMed PMID: 29726775]
González DA, Soble JR. Corticobasal syndrome due to sporadic Creutzfeldt-Jakob disease: a review and neuropsychological case report. The Clinical neuropsychologist. 2017 Apr:31(3):676-689. doi: 10.1080/13854046.2016.1259434. Epub 2016 Nov 22 [PubMed PMID: 27871202]
Level 3 (low-level) evidenceArmstrong MJ, Litvan I, Lang AE, Bak TH, Bhatia KP, Borroni B, Boxer AL, Dickson DW, Grossman M, Hallett M, Josephs KA, Kertesz A, Lee SE, Miller BL, Reich SG, Riley DE, Tolosa E, Tröster AI, Vidailhet M, Weiner WJ. Criteria for the diagnosis of corticobasal degeneration. Neurology. 2013 Jan 29:80(5):496-503. doi: 10.1212/WNL.0b013e31827f0fd1. Epub [PubMed PMID: 23359374]
Level 2 (mid-level) evidenceBuchmann I, Dangel M, Finkel L, Jung R, Makhkamova I, Binder A, Dettmers C, Herrmann L, Liepert J, Möller JC, Richter G, Vogler T, Wolf C, Randerath J. [Formula: see text] Limb apraxia profiles in different clinical samples. The Clinical neuropsychologist. 2020 Jan:34(1):217-242. doi: 10.1080/13854046.2019.1585575. Epub 2019 Apr 19 [PubMed PMID: 31002018]
Smania N, Girardi F, Domenicali C, Lora E, Aglioti S. The rehabilitation of limb apraxia: a study in left-brain-damaged patients. Archives of physical medicine and rehabilitation. 2000 Apr:81(4):379-88 [PubMed PMID: 10768524]
Level 1 (high-level) evidenceGoldenberg G. Apraxia and the parietal lobes. Neuropsychologia. 2009 May:47(6):1449-59. doi: 10.1016/j.neuropsychologia.2008.07.014. Epub 2008 Jul 25 [PubMed PMID: 18692079]
Lesourd M, Osiurak F, Baumard J, Bartolo A, Vanbellingen T, Reynaud E. Cerebral correlates of imitation of intransitive gestures: An integrative review of neuroimaging data and brain lesion studies. Neuroscience and biobehavioral reviews. 2018 Dec:95():44-60. doi: 10.1016/j.neubiorev.2018.07.019. Epub 2018 Aug 4 [PubMed PMID: 30086324]
Niessen E, Fink GR, Weiss PH. Apraxia, pantomime and the parietal cortex. NeuroImage. Clinical. 2014:5():42-52. doi: 10.1016/j.nicl.2014.05.017. Epub 2014 Jun 5 [PubMed PMID: 24967158]
Reynaud E, Lesourd M, Navarro J, Osiurak F. On the neurocognitive origins of human tool use : A critical review of neuroimaging data. Neuroscience and biobehavioral reviews. 2016 May:64():421-37. doi: 10.1016/j.neubiorev.2016.03.009. Epub 2016 Mar 11 [PubMed PMID: 26976352]
Garcea FE, Mahon BZ. Parcellation of left parietal tool representations by functional connectivity. Neuropsychologia. 2014 Jul:60():131-43. doi: 10.1016/j.neuropsychologia.2014.05.018. Epub 2014 Jun 2 [PubMed PMID: 24892224]
Goldenberg G, Spatt J. The neural basis of tool use. Brain : a journal of neurology. 2009 Jun:132(Pt 6):1645-55. doi: 10.1093/brain/awp080. Epub 2009 Apr 7 [PubMed PMID: 19351777]
Vanbellingen T, Bohlhalter S. Apraxia in neurorehabilitation: Classification, assessment and treatment. NeuroRehabilitation. 2011:28(2):91-8. doi: 10.3233/NRE-2011-0637. Epub [PubMed PMID: 21447909]
Power E, Code C, Croot K, Sheard C, Gonzalez Rothi LJ. Florida Apraxia Battery-Extended and revised Sydney (FABERS): design, description, and a healthy control sample. Journal of clinical and experimental neuropsychology. 2010 Jan:32(1):1-18. doi: 10.1080/13803390902791646. Epub [PubMed PMID: 19358011]
Papadopoulos G, Parissis D, Konstantinopoulou E, Natsis K, Gotzamani-Psarrakou A, Ioannidis P. Preliminary validation of the apraxia battery for adults-second edition (ABA-2) in Greek patients with dementia. Acta neurologica Belgica. 2022 Aug:122(4):997-1003. doi: 10.1007/s13760-021-01783-2. Epub 2021 Sep 1 [PubMed PMID: 34471971]
Level 1 (high-level) evidenceTessari A, Toraldo A, Lunardelli A, Zadini A, Rumiati RI. STIMA: a short screening test for ideo-motor apraxia, selective for action meaning and bodily district. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2015 Jun:36(6):977-84. doi: 10.1007/s10072-015-2203-4. Epub 2015 Apr 7 [PubMed PMID: 25847083]
Wirth K, Held A, Kalbe E, Kessler J, Saliger J, Karbe H, Fink GR, Weiss PH. [A New Diagnostic Tool for Apraxia in Patients with Right-Hemisphere Stroke: The Revised Cologne Apraxia Screening (KAS-R)]. Fortschritte der Neurologie-Psychiatrie. 2016 Oct:84(10):633-639 [PubMed PMID: 27788554]
Vanbellingen T, Kersten B, Van Hemelrijk B, Van de Winckel A, Bertschi M, Müri R, De Weerdt W, Bohlhalter S. Comprehensive assessment of gesture production: a new test of upper limb apraxia (TULIA). European journal of neurology. 2010 Jan:17(1):59-66. doi: 10.1111/j.1468-1331.2009.02741.x. Epub 2009 Jul 9 [PubMed PMID: 19614961]
Saeki S, Ogata H, Okubo T, Takahashi K, Hoshuyama T. Return to work after stroke. A follow-up study. Stroke. 1995 Mar:26(3):399-401 [PubMed PMID: 7886713]
Level 2 (mid-level) evidenceBuxbaum LJ, Haaland KY, Hallett M, Wheaton L, Heilman KM, Rodriguez A, Gonzalez Rothi LJ. Treatment of limb apraxia: moving forward to improved action. American journal of physical medicine & rehabilitation. 2008 Feb:87(2):149-61. doi: 10.1097/PHM.0b013e31815e6727. Epub [PubMed PMID: 18209511]
Baak B, Bock O, Dovern A, Saliger J, Karbe H, Weiss PH. Deficits of reach-to-grasp coordination following stroke: Comparison of instructed and natural movements. Neuropsychologia. 2015 Oct:77():1-9. doi: 10.1016/j.neuropsychologia.2015.07.018. Epub 2015 Jul 17 [PubMed PMID: 26189872]
Mutha PK, Stapp LH, Sainburg RL, Haaland KY. Motor Adaptation Deficits in Ideomotor Apraxia. Journal of the International Neuropsychological Society : JINS. 2017 Feb:23(2):139-149. doi: 10.1017/S135561771600120X. Epub [PubMed PMID: 28205499]
Park JE. Repetitive Transcranial Magnetic Stimulation for Limb-Kinetic Apraxia in Parkinson's Disease. Journal of clinical neurology (Seoul, Korea). 2018 Jan:14(1):110-111. doi: 10.3988/jcn.2018.14.1.110. Epub 2017 Oct 31 [PubMed PMID: 29141285]