Introduction
Endophthalmitis, a dreaded ophthalmic emergency, is defined as the intraocular infection of the coats of the eyeball associated with diffuse vitreous inflammation. It can manifest in significant ocular and systemic complications.[1] The mode of spread can be exogenous or endogenous.[2] Exogenous endophthalmitis can result from trauma, post-surgery, or secondary to keratitis. In contrast, endogenous endophthalmitis, also called metastatic endophthalmitis, results from hematogenous spread of microorganisms secondary to underlying systemic pathology like diabetes, immunosuppression, renal pathology, etc. Suspected cases should undergo imaging like ultrasound B scan, aqueous and vitreous tap for culture and sensitivity, vitreous biopsy, or polymerase chain reaction whenever indicated for rapid diagnosis.[3]
Prompt clinical diagnosis, targeted investigation, meticulous management, and regular follow-up is mandated to safeguard vision in these cases. Medical management includes topical and systemic antibiotics or antifungals, intravitreal antibiotics or antifungals, and surgical treatment of choice is pars plana vitrectomy. The collaboration of the treating ophthalmologist or vitreoretinal surgeon, microbiologists, pathologists, and the critical care physician plays a vital role in determining the patient's final systemic and ocular outcome.[4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Endogenous endophthalmitis (EE) has a multifactorial etiology, and causative agents vary from region to region. The causative agents can be fungal or bacterial, with fungal organisms dominating the majority of cases.[4] In studies from Asia, fungal EE accounts for nearly 11.1 to 17.54% of total cases.[5] The most common causative agent for bacterial EE is gram-positive streptococcus and staphylococcus. Gram-negative bacterial EE is more commoner in Asian countries.[6] Among fungal species, Candida albicans account for many cases being the most common yeast, and among the molds, Aspergillus flavus is the commonest.[7]
Klebsiella pneumonia, a gram-negative rod bacterium, is another causative agent reported to cause EE. Klebsiella has been reported in patients with liver abscess, diabetes mellitus, infective endocarditis, and after a routine colonoscopy.[8] Recently, Rudez et al. reported a case of EE secondary to Clostridium septicum.[9] Yue et al. reported EE secondary to an opportunistic pathogen Citrobacter koseri.[10]
In fungal EE, mold infections are more common after chemotherapy and in patients undergoing liver and cardiac transplants, hematological malignancy, or hematopoietic stem cell transplantation (HSCT). Aspergillus pneumonia has been blamed for causing EE in a small subset of patients.[11] Candida EE has been reported in patients on ventilators and neonates.[12]
The most common systemic risk factors for EE are diabetes mellitus, immunosuppression, patients on long term corticosteroids, history of recent hospitalization, ventilator-associated pneumonia, urinary tract infection, malignancy like lymphoma and leukemia, colon adenocarcinoma, dental infection, scleral perforation, vertebral osteomyelitis, liver abscess, asplenia, hypogammaglobulinemia, cardiac or renal transplant, acquired immune deficiency syndrome, chronic alcoholism, intravenous catheters and drug abuse (Bacillus cereus). Mishra et al. reported a case of EE secondary to multifocal staphylococcal brain abscess associated with septic foci.[13][14][15][16][17][18]
Neonatal EE is an alarming entity in children with bacterial infections, candida infection, malnourishment, retinopathy of prematurity, low birth weight, septicemia. The most common bacteria reported are streptococci, S. agalactiae, Pseudomonas, and Klebsiella. Azar et al., in their retrospective analysis, reported 3 cases of pediatric EE out of 26 cases. A small number of EE cases are also reported secondary to occult systemic infections, which are culture negative.[12][19][20] Recently few case series have been reported in patients with COVID-19 possible reason being immunosuppression.[21][22][23]
Epidemiology
The reported incidence of EE is 2 to 8%.[1][4] The first case of EE dates back to 1856, which was secondary to recurrent Klebsiella infection.[24] A major review article in 2003 reported 335 cases of bacterial EE.[25] The infection can occur at any age with equal gender predilection. In a study comprising 27 subjects, the reported mean age of the patients was 63.[26] The ratio of involvement of the right to left eye is 2 to 1. The right eye is more commonly involved due to more proximal and direct blood flow from the right carotid artery. Approximately 25% of cases have a bilateral presentation.[27]
Pathophysiology
Endogenous endophthalmitis is a blood-borne metastatic infection from the primary inoculation site secondary to bacterial or a fungal pathology.[27] The microorganism primarily spreads through the posterior segment vessels. The right eye has more predilection due to dominant and direct blood flow from the right carotid artery.
The direct infectious spread has also been reported from the brain to the optic nerve. The primary mechanism of damage in EE is septic emboli that migrate to the posterior segment vessels. This, in turn, acts as a focus for the spread of microorganisms to the neighboring tissues after breaching the blood-retinal barrier. Further, the microorganism proliferates and causes inflammation within these tissues.
The infection then spread from the posterior segment to the anterior segment of the eye. One of the previous studies document no underlying source of infection in approximately 44% of the cases, but still, EE patients should undergo a detailed systemic evaluation to rule out the primary focus of infection.[28][29]
History and Physical
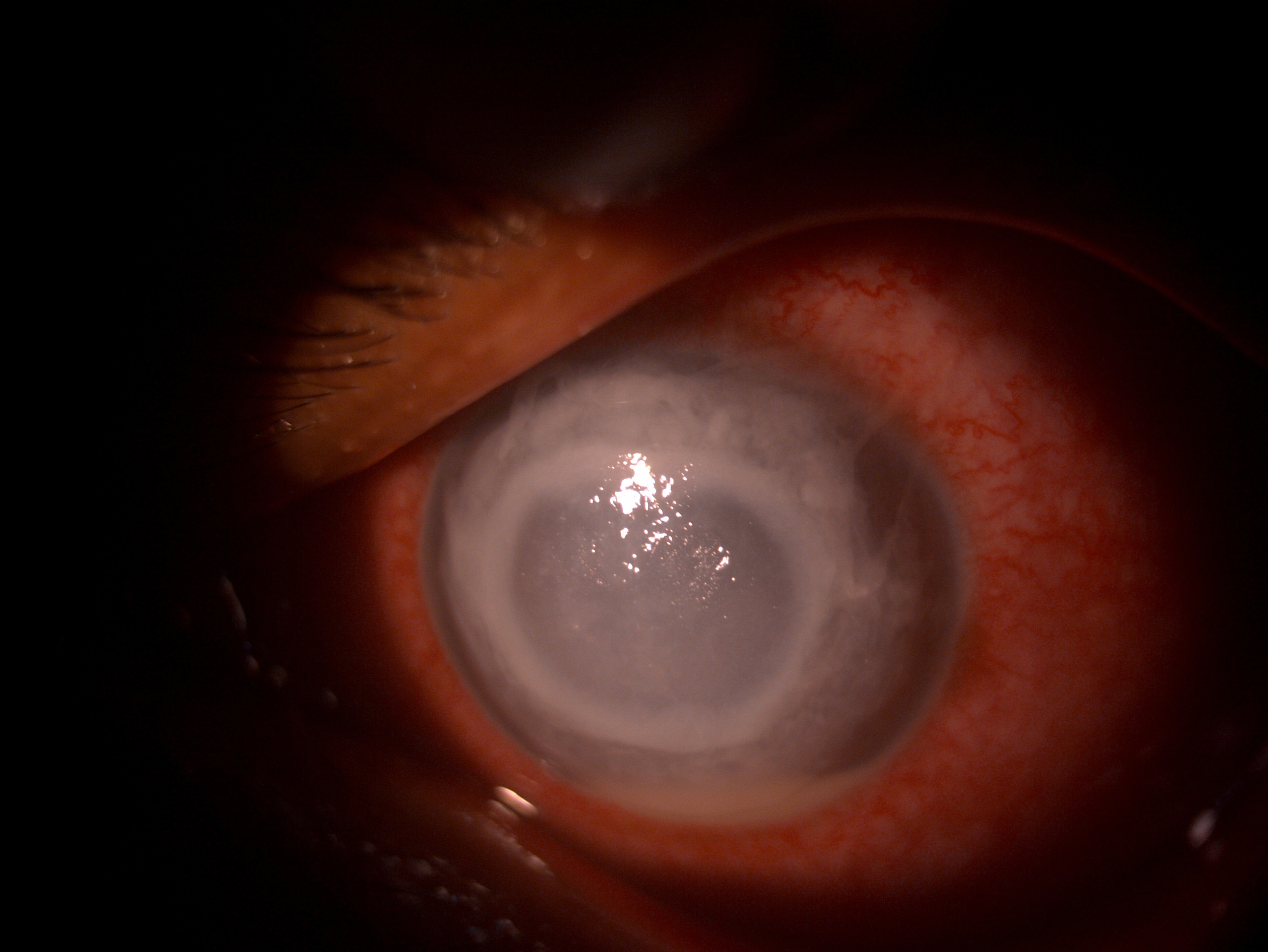
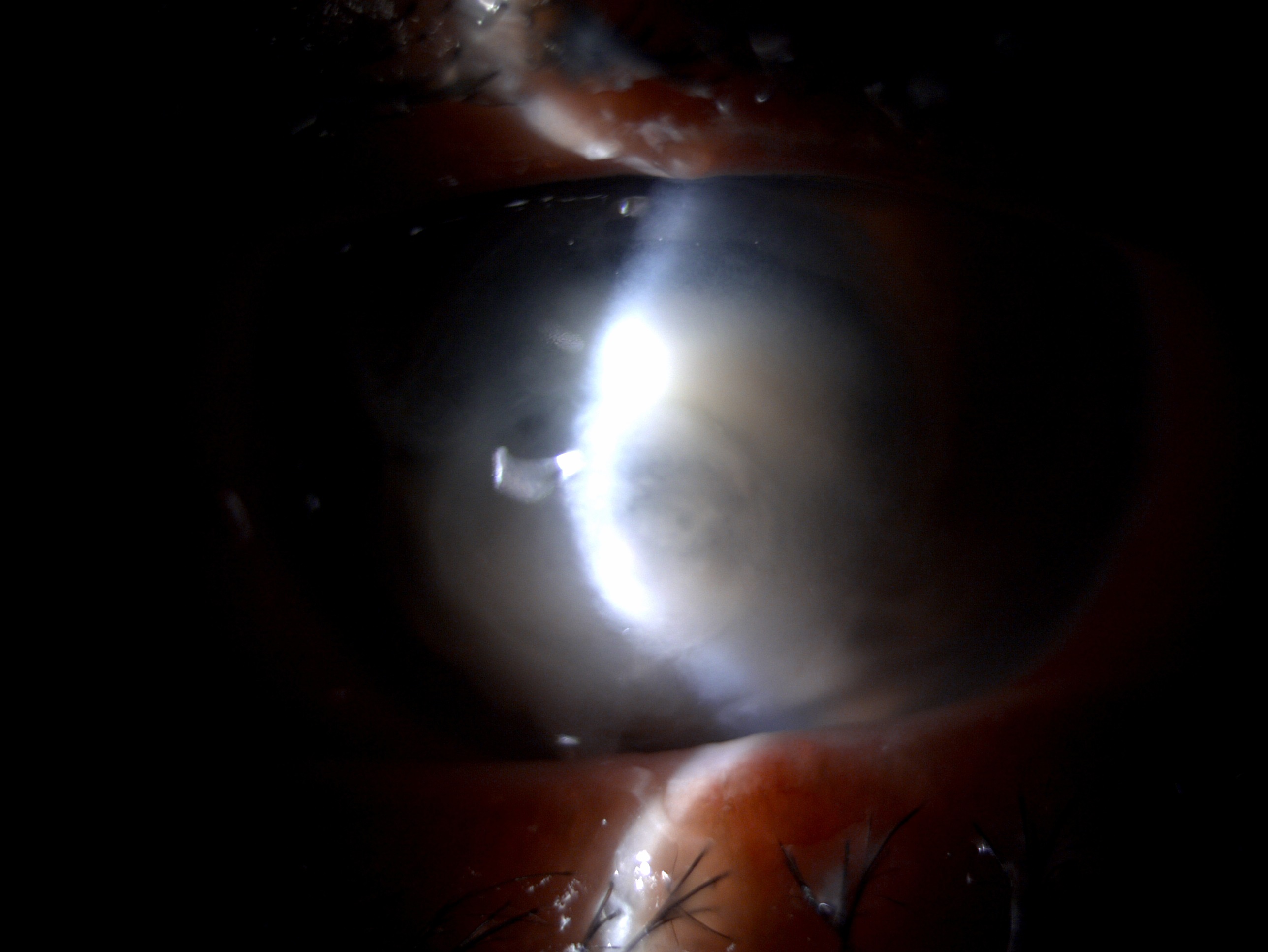
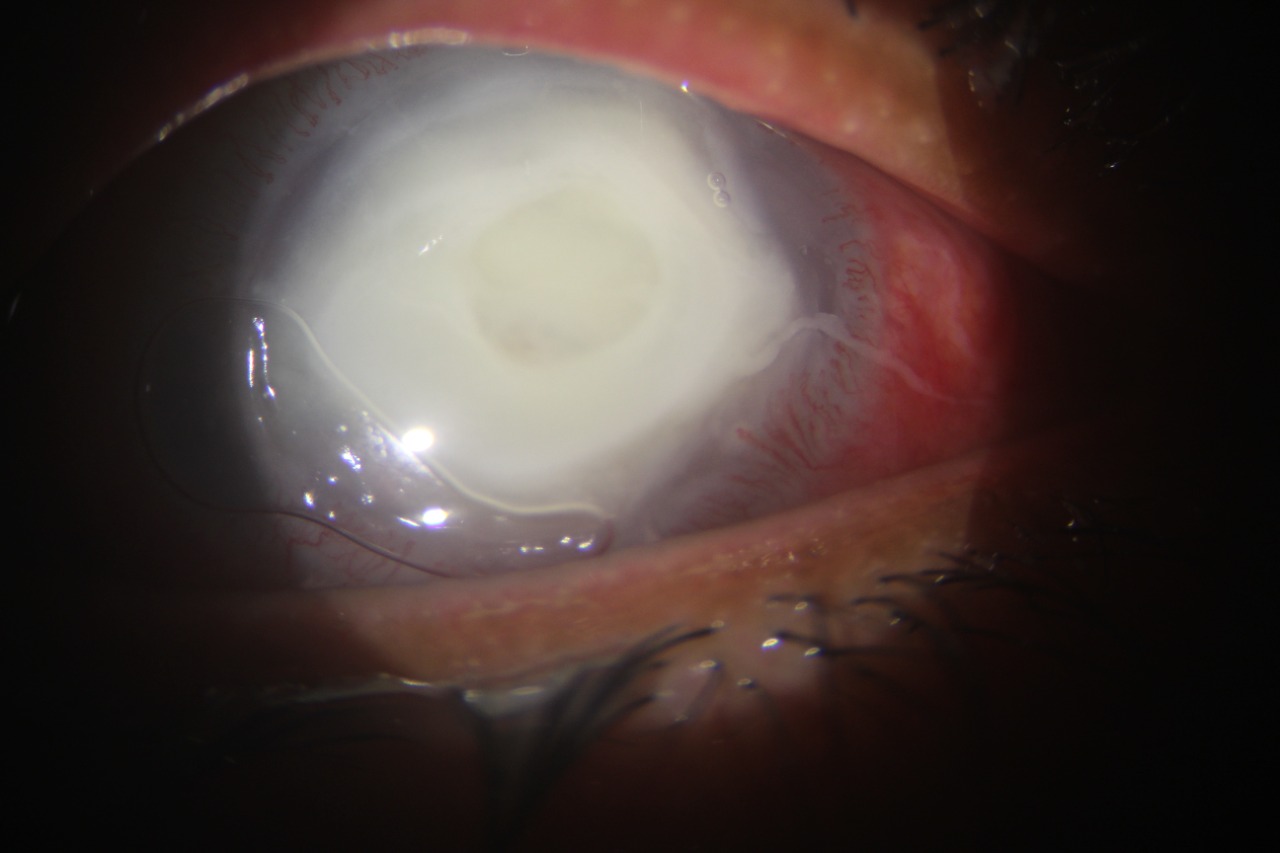
The symptoms of endogenous endophthalmitis vary from pain, redness, irritation, swelling photophobia, defective vision, floaters, and flashes. The clinical signs range from periorbital edema, scleral inflammation, chemosis, conjunctival congestion, corneal infiltrate, endothelial exudates, corneal edema, anterior chamber reaction, hypopyon, fibrinous membrane, iris exudates, iris nodules, sluggish or fixed pupil, relative afferent pupillary defect, posterior synechiae, cataract, absent red reflex, vitreous haze, anterior vitreous cells, vitreous floaters, membranes and exudates.[30][14][31] Bacterial EE is known to cause more anterior chamber inflammation. Bilateral EE is more common with Mycobacterium tuberculosis.
The most important diagnostic feature of EE is vitreous involvement. Aspergillus flavus is known to cause yellow/ white exudates in the vitreous, which vary from focal to diffuse. The hallmark feature of Candida EE is the presence of fluffy cotton wool-like white retinal exudates or colonies along with vitritis.[32] Subretinal and choroidal abscesses have also been reported in cases of endogenous bacterial endophthalmitis. In patients with relatively clear media with less severe vitreous involvement, other findings like subretinal, preretinal, flame-shaped hemorrhage, Roth spots, cotton wool spots, retinal and choroidal detachment can also be documented. MRSA has been associated with a high rate of retinal detachment when the presentation is delayed more than two weeks after the onset of symptoms.[33]
EE can be broadly classified into three categories based on ocular signs and symptoms, as detailed below.[29] Petit et al. earlier has proposed a classification for fungal EE.[34]
|
S. No |
Involvement |
Classification category |
||
|
Probable |
Possible |
Positive |
||
|
1 |
Conjunctiva and Cornea |
Conjunctival congestion, chemosis |
Conjunctival congestion, chemosis |
Conjunctival congestion, chemosis Corneal infiltrates |
|
2 |
Anterior chamber (AC) |
AC reaction, no hypopyon |
Hypopyon ≤ 1.5 mm
|
Hypopyon ≥ 1.5 mm
|
|
3 |
Iris and uveal tissue |
Abscess |
Exudates |
- |
|
4 |
Vitreous |
Vitreous haze absent
|
Vitreous haze is present, but there is an absence of exudates
|
Exudates in vitreous
|
|
5 |
Retina and Choroidal |
- |
Non-necrotizing, focal or discrete chorioretinal lesions, Optic neuritis, Intraretinal hemorrhage
|
Arteriolar septic emboli, necrotizing retinitis, perivascular hemorrhage |
|
6 |
Sclera
|
- |
Scleritis |
- |
|
7 |
Others |
Fever |
White reflex in the new-born |
Panophthalmitis |
Evaluation
Apart from clinical diagnostic, EE is confirmed by imaging and lab investigations. Every case warrants a detailed slit lamp and dilated fundus evaluation. Sometimes the diagnosis is delayed since the clinical picture can have a lot of differentials, and multiple assessments are required before reaching a conclusive diagnosis. The prime importance should be given to systemic evaluation and management.
Imaging Modalities
B Scan Ultrasound
B scan ultrasound is an essential diagnostic modality to pick up vitritis, membranes, exudates in the vitreous cavity, retinal detachment, choroidal detachment, and choroidal abscess. The exudates in the vitreous cavity are present as echoes on the B scan. EE is also known to cause a choroidal abscess, which appears as dome-shaped elevation on B scan similar to choroidal detachment.[35]
Optical Coherence Tomography
Optical coherence tomography (OCT) is an important imaging modality to delineate the retinal and subretinal space. OCT can help localize the exudates within subretinal layers, lesions of the retinal pigment elevation, retinal edema, vitreous cells and exudates, and choroidal involvement.[36]
Anterior Chamber and Vitreous Tap
An anterior chamber aqueous tap of 0.1-0.2 ml can be performed with a 23 G needle. Vitreous tap of 1-2 ml is performed with the help of a 25 G needle. The sample can also be obtained while performing vitrectomy and subjected to culture, sensitivity, and histopathological examination. Lingappan et al. proved that samples obtained with vitrectomy showed a better culture positivity (92%) than vitreous tap (44%). Similarly, Zhang et al. showed that the sample obtained needle biopsy had a lower diagnostic yield than vitrectomy as the vitrectomy samples were closer to the retinal surface.[37]
Polymerase Chain Reaction
The samples obtained through aqueous and vitreous tap can be subjected to a real-time polymerase chain reaction (RT-PCR), with very high sensitivity and specificity. RTPCR has proven high sensitivity and specificity for fungi as per the analysis by Sugita et al. In culture-negative cases of EE; it has proven to be a better diagnostic modality for detecting microorganisms. PCR results are obtained within 90 minutes, with better diagnostic yield than culture results with no risk of contamination. The major limitation of PCR is that an antibiotic susceptibility pattern cannot be obtained through this.[38]
Blood Culture
Blood culture is an important diagnostic modality for the diagnosis of systemic infection. Three consecutive samples can be obtained on three days under aseptic precautions for a better diagnostic yield. Besides blood culture, it is vital to obtain urine culture to identify occult microorganisms. According to a few previous studies, blood culture has shown a higher culture positivity than the vitreous sample, probably due to the sample volume obtained. Culture at extraocular sites has yielded a 21-100% positivity rate as per previous reports.[17]
Upcoming Modalities
2-Deoxy-2-[18F] Fluoro-Dglucose Positron Emission Tomography/Computed Tomography Scan
Mehta et al. recently documented using 2-Deoxy-2-[18F] fluoro-D-glucose positron emission tomography/computed tomography scan for systemic assessment of patients with presumed fungal EE in patients with COVID-19 infection.[39]
Treatment / Management
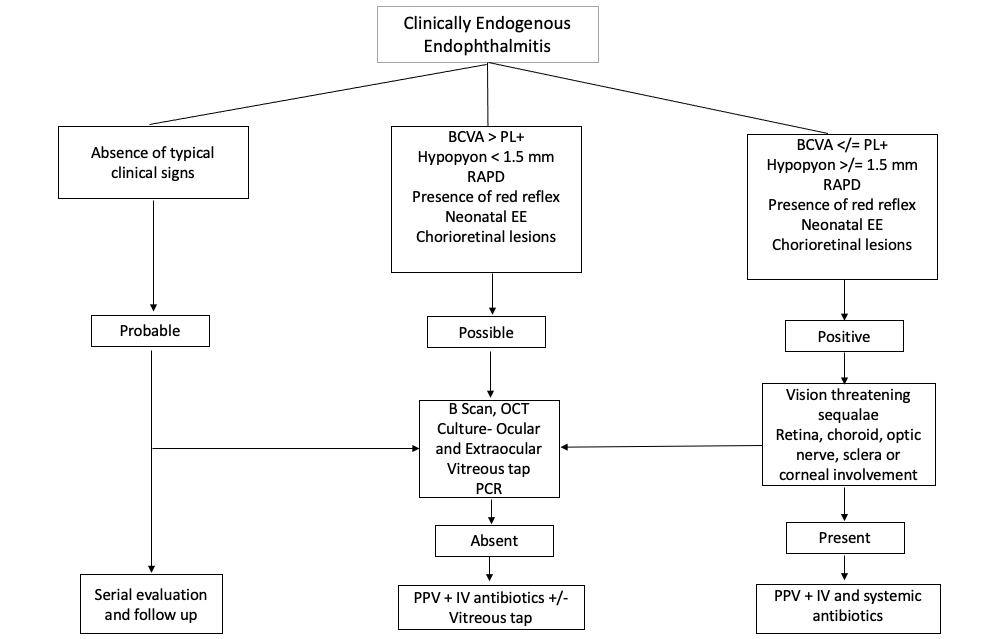
Endogenous endophthalmitis is an emergency, and prompt diagnosis and meticulous management are required to safeguard vision in these cases. The treatment is governed by the stage of the disease, offending microorganism, mode and route of infection, and systemic status of the patient. A flowchart of how to manage endogenous endophthalmitis is depicted below.
Management Protocol for Bacterial Endogenous Endophthalmitis
Systemic Antibacterials
Bacterial EE warrants treatment of systemic infection with antibiotics. Once the blood culture results are available, systemic antibiotics can be initiated. Moreover, severe ocular infection warrants the addition of intravitreal injections. Non-resolving cases with rapidly progressive bacteremia will require pars plana vitrectomy.
Local Therapy
Once infection EE is suspected, a sample for culture and sensitivity should be obtained, and intravitreal antibiotics should be initiated. Early intravitreal antibiotics should be initiated within 24 hours of presentation as they have been reported to have a better and favorable outcome. Before the etiology is established, broad-spectrum intravitreal antibiotics should be administered. Vancomycin 1mg/0.1 ml and cefazolin 2.25 mg/0.1 ml covers gram-positive bacteria, and 2.25 mg/0.1 ml ceftazidime or 0.4 mg/0.1 ml amikacin are the drug of choice for gram-negative bacteria. Vancomycin is the drug of choice for MRSA. However, there have been recent reports of vancomycin resistance staphylococcus aureus (VRSA) also. The drugs commonly used for VRSA are daptomycin 200 ug/0.1 ml and quinupristin/dalfopristin 0.4 mg/0.1 ml. Fluoroquinolones are a broad spectrum with gram-positive and negative coverage.
Once the culture results are available, targeted therapy should be started for rapid recovery. Prompt diagnosis and targeted treatment are essential for a final better outcome. Antibiotics should be used cautiously in pregnant and lactating mothers. Penicillin group of drugs, cephalosporins, and erythromycin can be used safely in these patients. Cartilage abnormalities have been reported secondary to fluoroquinolones; hence they should not be used as the first line in pregnant women.[40][41][11](B2)
Management Protocol for Endogenous Fungal Endophthalmitis
Candida Endogenous Endophthalmitis
The drug of choice for candida EE is intravitreal amphotericin or voriconazole. Amphotericin B (AMB) deoxycholate is given in the dose of 5 to 10 ug/0.1 ml dextrose or sterile saline. The patient should be reassessed after 48 hours, and if needed, the dose can be repeated. AMB has been reported to cause nephrotoxicity, hypotension, and arrhythmia. Hence the patient should be closely monitored for these side effects. Intravitreal voriconazole is administered in a dose of 100-200 ug/0.1 ml sterile saline.[42][43](B3)
The other alternative recommended by the infectious disease society of America (IDSA) is fluconazole. The recommended dose is 400-800 mg per day. Hamada et al. recommended fluconazole as the first-line therapy because of its better side effect profile than AMB. In severe cases with non-resolving vitritis, pars plana vitrectomy is the treatment of choice. The treatment duration depends on the clinical picture, but a minimum of 6 weeks is recommended.[44][45](A1)
Endogenous Endophthalmitis Secondary to Aspergillus, Paecilomyces, and Fusarium
The drugs implicated are voriconazole, AMB, and fluconazole. Voriconazole has proven high efficacy of approximately 100% in these cases. Pars plana vitrectomy with lensectomy or intraocular lens removal should be performed in non-resolving cases. In bedridden patients, those who are severely immunocompromised or unable to tolerate surgery, systemic antifungal therapy should be initiated.[46][47][48](B2)
Pars Plana Vitrectomy
Pars plana vitrectomy (PPV) is the treatment of choice for non-resolving vision-threatening bacterial and fungal EE cases. PPV serves both diagnostic and therapeutic purposes. Pre-surgery or intraoperatively intravitreal drugs can be administered to reduce the microorganism load. Vitrectomy helps to reduce the microorganism load in the posterior segment and assists in rapid recovery. Vitrectomy is based on the vitreoretinal surgeon's discretion.
Early vitrectomy has been reported to cause a reduced incidence of retinal detachment and has a better globe salvage rate. The incidence of enucleation and evisceration is also reduced. Sato et al. suggested early vitrectomy in Candida EE cases. Zhang et al. found better visual outcomes in patients who were subjected to early vitrectomy. Yoon et al. suggested early PPV in Klebsiella endophthalmitis, which may result in better visual effects.[49]
Corticosteroids
The role of intravitreal and systemic steroid use in EE is controversial, and there are no set guidelines for the same. Bacterial endotoxins and profound inflammation is known to cause retinal pigment epithelial damage and necrosis. Steroids combat inflammation, alleviate leucocyte migration, reduce cytokine storm and stabilize the blood-retinal barrier. Jackson et al. showed that patients with EE treated with steroids resulted in a better visual outcome. In contrast, Shuwan et al. showed no significant benefit with the use of steroids. Lindstedt et al., in their multicentric randomized trial, showed that intravitreal dexamethasone had no added benefit. Hence, in a nutshell, steroids should be used with caution in EE patients.[50][51](A1)
Differential Diagnosis
Infectious
- Cytomegalovirus
- Herpes simplex virus
- Varicella-zoster virus
- Epstein bar virus
- Disseminated toxoplasmosis
- Disseminated viral retinitis
- Tuberculosis
- Lyme's
- Pythium[52][53][54]
Non-infectious
- Vogt-Koyanagi-Harada syndrome
- Sarcoidosis
- Behcet syndrome[55]
- Idiopathic
- Toxic anterior segment syndrome
- Sympathetic ophthalmia[56]
- Juvenile idiopathic arthritis
- Posterior scleritis
Postoperative endophthalmitis (after any surface or intraocular surgery)
Masquerade
- Leukemia
- Lymphoma
- Retinoblastoma
- Choroidal melanoma
- Tumour necrosis with inflammation
Intraocular foreign body
White dot syndromes
- Punctate inner choroidopathy
- Serpiginous choroidopathy
- Multifocal choroiditis and panuveitis
- Subretinal fibrosis and uveitis
- Multiple evanescent white dot syndrome
- Acute posterior multifocal placoid pigment epitheliopathy
- Birdshot chorioretinopathy
Asteroid Hyalosis
Disseminated Intravascular Coagulation
Thrombotic Thrombocytopenic Purpura
Prognosis
The prognosis of endogenous endophthalmitis depends on the presentation time, clinical manifestation, the extent of vitreous involvement, and virulence of the offending microorganism. It's a complex entity to diagnose, and due to various comorbidities, it is often picked up late. However, studies have proven that yeasts have the best prognosis, followed by bacteria followed by molds which have the worst prognosis.
Patients who present late and in whom diagnosis and treatment are delayed often land up with complete vision loss, and the prognosis is poor in these cases. The patients requiring vitreous tap are at risk for retinal detachment, and the prognosis is guarded in these cases. Zenith et al., in their analysis, showed that bacterial EE had a poor outcome and prognosis compared to fungal EE and these cases usually require enucleation and evisceration.[17] Yonekawa et al., in their study, proven that prompt diagnosis and treatment was associated with 64% of patients having visual outcomes better than counting finger (CF) in bacterial EE.[41]
Similarly, Itoh et al. showed that early and aggressive vitrectomy within two weeks of diagnosis results in good final outcomes, and the prognosis is good in these cases.[57] Among the offending microorganisms, it has been reported that MRSA EE patients have a poor prognosis and high mortality. However, few studies have proven variable association between the two. Connell et al., in their analysis, showed that the majority of patients with Klebsiella EE required vitrectomy.[58] Ang et al. found that hypopyon in Klebsiella EE can be a prognostic predictor.[40]
Complications
Postoperative and Rehabilitation Care
All patients with EE should be admitted to the hospital, and close monitoring of systemic and ocular parameters is mandated in these cases. Patients requiring intravitreal injections should be evaluated daily for improvement in clinical picture and need for further injections. In case of worsening EE, the surgeon's discretion makes a decision for pars plana vitrectomy. Post vitrectomy, the patient should be started on topical steroids prednisolone 1% or dexamethasone 0.1% in tapering doses 8/7/6/5/4/3/2/1 every week, 5% homatropine two times per day, topical 0.5% timolol two times per day, and oral antibiotics and anti-inflammatory. The patient should be followed up closely to assess the clinical picture and rule out any complications.[63]
Consultations
Endogenous endophthalmitis is a severe sight-threatening emergency, and all patients with suspected EE must be referred and evaluated by a vitreoretinal surgeon. The vitreoretinal surgeon has a vital role to play in the diagnosis and management of these cases.
Deterrence and Patient Education
The patients must be explained the serious nature of the pathology and warning signs and symptoms like pain, redness, swelling, sudden reduction in visual acuity, and photophobia. The patients must be explained that the condition will require hospital admission and intensive treatment in topical and oral drugs, intravitreal injection, and the need for surgery. The patient should be explained regarding visual prognosis and to have realistic expectations.[17]
Enhancing Healthcare Team Outcomes
Endogenous endophthalmitis is usually seen in patients with diabetes mellitus, immunosuppression, and other systemic pathologies. Nursing staff must keep a check on blood sugar, temperature, and other vital parameters. The treating physician must be highly suspicious of EE if the patient reports pain, redness, and sudden vision loss. Patients will all these symptoms must be referred to a vitreoretinal (VR) surgeon for meticulous management. The VR surgeon also plays a vital role in counseling and explaining the prognosis of the pathology to the patient. Nursing staff also plays a crucial role in counseling and regularly administering drugs to the patients in collaboration with the pharmacist. The patient's final visual and systemic outcome depends on the multidisciplinary approach by the physician, pharmacist, nursing staff, and the vitreoretinal surgeons.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
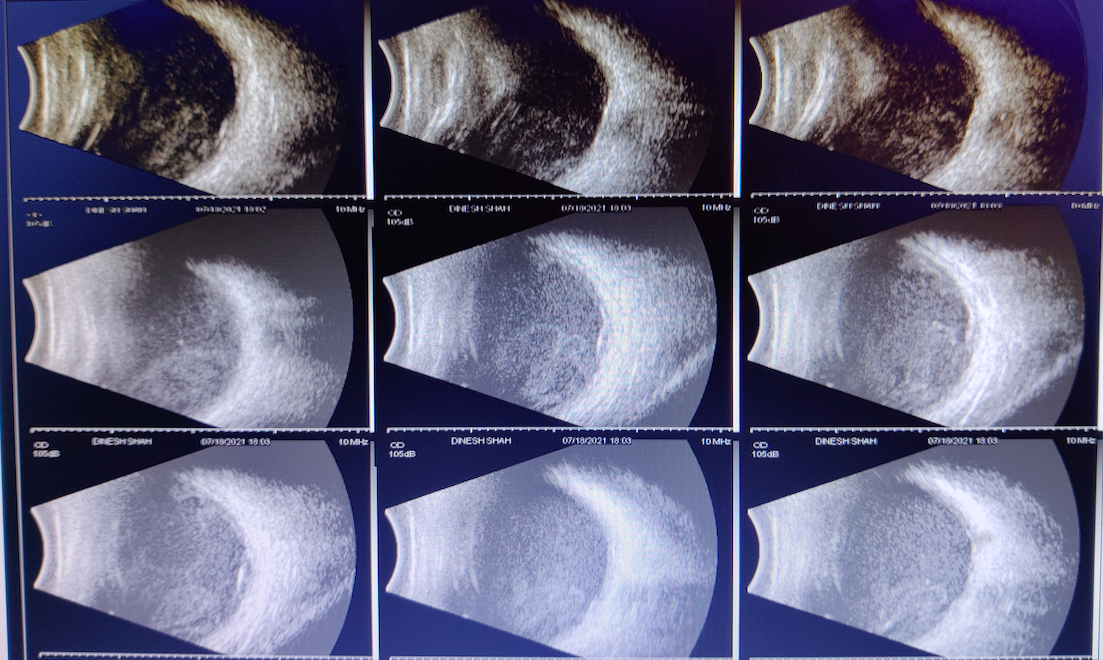
Digital B Scan images of the patient with endogenous endophthalmitis depicting IOL reverberation, multiple dot, and membranous vitreous echoes of variable reflectivity, There is no evidence of retinal detachment, choroidal detachment or retinochoroidal thickening
Contributed by Dr. Bharat Gurnani, MBBS, DNB, FCRS, FICO, MRCS Ed, MNAMS
References
Novosad BD,Callegan MC, Severe bacterial endophthalmitis: towards improving clinical outcomes. Expert review of ophthalmology. 2010 Oct; [PubMed PMID: 21572565]
Level 2 (mid-level) evidenceLynn WA,Lightman S, The eye in systemic infection. Lancet (London, England). 2004 Oct 16-22; [PubMed PMID: 15488221]
Kernt M,Kampik A, Endophthalmitis: Pathogenesis, clinical presentation, management, and perspectives. Clinical ophthalmology (Auckland, N.Z.). 2010 Mar 24; [PubMed PMID: 20390032]
Level 3 (low-level) evidenceSchiedler V,Scott IU,Flynn HW Jr,Davis JL,Benz MS,Miller D, Culture-proven endogenous endophthalmitis: clinical features and visual acuity outcomes. American journal of ophthalmology. 2004 Apr; [PubMed PMID: 15059712]
Level 2 (mid-level) evidenceSharma S,Padhi TR,Basu S,Kar S,Roy A,Das T, Endophthalmitis patients seen in a tertiary eye care centre in Odisha: a clinico-microbiological analysis. The Indian journal of medical research. 2014 Jan; [PubMed PMID: 24604043]
Jackson TL,Paraskevopoulos T,Georgalas I, Systematic review of 342 cases of endogenous bacterial endophthalmitis. Survey of ophthalmology. 2014 Nov-Dec; [PubMed PMID: 25113611]
Level 1 (high-level) evidenceSridhar J,Flynn HW Jr,Kuriyan AE,Miller D,Albini T, Endogenous fungal endophthalmitis: risk factors, clinical features, and treatment outcomes in mold and yeast infections. Journal of ophthalmic inflammation and infection. 2013 Sep 20; [PubMed PMID: 24053550]
Hu CC,Ho JD,Lou HY,Keller JJ,Lin HC, A one-year follow-up study on the incidence and risk of endophthalmitis after pyogenic liver abscess. Ophthalmology. 2012 Nov; [PubMed PMID: 22817832]
Level 2 (mid-level) evidenceRudež LK,Petrović I,Bulić K,Mandić JJ, A rare case of devastating Clostridium septicum endogenous endophthalmitis. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2021 Nov 1; [PubMed PMID: 34724111]
Level 3 (low-level) evidenceYue Q,Zhang Q,Wang Y,He X,Ding K,Wang X,Xi H,Wang L,Zhang Y,Wu C, Complete genome sequencing and comparative analysis of Citrobacter koseri CKNJ, a strain isolated from patient with endogenous endophthalmitis. Japanese journal of infectious diseases. 2021 Aug 31; [PubMed PMID: 34470967]
Level 2 (mid-level) evidenceSahu C,Kumar K,Sinha MK,Venkata A,Majji AB,Jalali S, Review of endogenous endophthalmitis during pregnancy including case series. International ophthalmology. 2013 Oct; [PubMed PMID: 23263732]
Level 3 (low-level) evidenceMoshfeghi AA,Charalel RA,Hernandez-Boussard T,Morton JM,Moshfeghi DM, Declining incidence of neonatal endophthalmitis in the United States. American journal of ophthalmology. 2011 Jan; [PubMed PMID: 20970776]
Level 2 (mid-level) evidenceDurand ML, Endophthalmitis. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2013 Mar; [PubMed PMID: 23438028]
Lamaris GA,Esmaeli B,Chamilos G,Desai A,Chemaly RF,Raad II,Safdar A,Lewis RE,Kontoyiannis DP, Fungal endophthalmitis in a tertiary care cancer center: a review of 23 cases. European journal of clinical microbiology [PubMed PMID: 18183439]
Level 2 (mid-level) evidenceKeyashian K,Malani PN, Endophthalmitis associated with intravenous drug use. Southern medical journal. 2007 Dec; [PubMed PMID: 18090965]
Level 3 (low-level) evidenceCheng HH,Ding Y,Wu M,Tang CC,Zhang RJ,Lin XF,Xu JT, Endogenous aspergillus endophthalmitis after kidney transplantation. International journal of ophthalmology. 2011; [PubMed PMID: 22553722]
Wu ZH,Chan RP,Luk FO,Liu DT,Chan CK,Lam DS,Lai TY, Review of Clinical Features, Microbiological Spectrum, and Treatment Outcomes of Endogenous Endophthalmitis over an 8-Year Period. Journal of ophthalmology. 2012; [PubMed PMID: 23533699]
de Lima LM,Cecchetti SA,Cecchetti DF,Arroyo D,Romão EA,Dantas M,Neto MM, Endophthalmitis: a rare but devastating metastatic bacterial complication of hemodialysis catheter-related sepsis. Renal failure. 2012; [PubMed PMID: 22017567]
Level 3 (low-level) evidenceNoyola DE,Bohra L,Paysse EA,Fernandez M,Coats DK, Association of candidemia and retinopathy of prematurity in very low birthweight infants. Ophthalmology. 2002 Jan; [PubMed PMID: 11772584]
Level 2 (mid-level) evidenceBasu S,Kumar A,Kapoor K,Bagri NK,Chandra A, Neonatal endogenous endophthalmitis: a report of six cases. Pediatrics. 2013 Apr; [PubMed PMID: 23478867]
Level 3 (low-level) evidenceBilgic A,Sudhalkar A,Gonzalez-Cortes JH,March de Ribot F,Yogi R,Kodjikian L,Mathis T, ENDOGENOUS ENDOPHTHALMITIS IN THE SETTING OF COVID-19 INFECTION: A Case Series. Retina (Philadelphia, Pa.). 2021 Aug 1; [PubMed PMID: 33734193]
Level 2 (mid-level) evidenceAgarwal M,Sachdeva M,Pal S,Shah H,Kumar R M,Banker A, Endogenous Endophthalmitis A Complication of COVID-19 Pandemic: A Case Series. Ocular immunology and inflammation. 2021 May 19; [PubMed PMID: 34255587]
Level 2 (mid-level) evidenceGurnani B,Kaur K, Impact of the COVID-19 pandemic on clinical ophthalmology. The Indian journal of medical research. 2021 Jan [PubMed PMID: 33473015]
Tsai AS,Lee SY,Jap AH, An unusual case of recurrent endogenous Klebsiella endophthalmitis. Eye (London, England). 2010 Oct; [PubMed PMID: 20559330]
Level 3 (low-level) evidenceJackson TL,Eykyn SJ,Graham EM,Stanford MR, Endogenous bacterial endophthalmitis: a 17-year prospective series and review of 267 reported cases. Survey of ophthalmology. 2003 Jul-Aug; [PubMed PMID: 12850229]
Level 3 (low-level) evidenceBinder MI,Chua J,Kaiser PK,Procop GW,Isada CM, Endogenous endophthalmitis: an 18-year review of culture-positive cases at a tertiary care center. Medicine. 2003 Mar; [PubMed PMID: 12640186]
Level 2 (mid-level) evidenceGreenwald MJ,Wohl LG,Sell CH, Metastatic bacterial endophthalmitis: a contemporary reappraisal. Survey of ophthalmology. 1986 Sep-Oct; [PubMed PMID: 3541265]
Level 3 (low-level) evidenceSamiy N,D'Amico DJ, Endogenous fungal endophthalmitis. International ophthalmology clinics. 1996 Summer; [PubMed PMID: 8989607]
Level 3 (low-level) evidenceChee SP,Jap A, Endogenous endophthalmitis. Current opinion in ophthalmology. 2001 Dec; [PubMed PMID: 11734687]
Level 3 (low-level) evidenceLingappan A,Wykoff CC,Albini TA,Miller D,Pathengay A,Davis JL,Flynn HW Jr, Endogenous fungal endophthalmitis: causative organisms, management strategies, and visual acuity outcomes. American journal of ophthalmology. 2012 Jan; [PubMed PMID: 21917234]
Level 2 (mid-level) evidenceAgarwal M,Biswas J,Mathur U,Sijwali MS,Singh AK, Aspergillus iris granuloma in a young male: a case report with review of literature. Indian journal of ophthalmology. 2007 Jan-Feb; [PubMed PMID: 17189896]
Level 3 (low-level) evidenceOude Lashof AM,Rothova A,Sobel JD,Ruhnke M,Pappas PG,Viscoli C,Schlamm HT,Oborska IT,Rex JH,Kullberg BJ, Ocular manifestations of candidemia. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2011 Aug 1; [PubMed PMID: 21765074]
Level 1 (high-level) evidenceKhan A,Okhravi N,Lightman S, The eye in systemic sepsis. Clinical medicine (London, England). 2002 Sep-Oct; [PubMed PMID: 12448593]
Tanaka M,Kobayashi Y,Takebayashi H,Kiyokawa M,Qiu H, Analysis of predisposing clinical and laboratory findings for the development of endogenous fungal endophthalmitis. A retrospective 12-year study of 79 eyes of 46 patients. Retina (Philadelphia, Pa.). 2001; [PubMed PMID: 11421007]
Level 2 (mid-level) evidenceRodrigues IA,Jackson TL, A high-definition view of endogenous fungal endophthalmitis. The Lancet. Infectious diseases. 2014 Apr; [PubMed PMID: 24670628]
Level 3 (low-level) evidenceCho M,Khanifar AA,Chan RV, Spectral-domain optical coherence tomography of endogenous fungal endophthalmitis. Retinal cases [PubMed PMID: 25389883]
Level 3 (low-level) evidencePalexas GN,Green WR,Goldberg MF,Ding Y, Diagnostic pars plana vitrectomy report of a 21-year retrospective study. Transactions of the American Ophthalmological Society. 1995; [PubMed PMID: 8719683]
Level 2 (mid-level) evidenceSowmya P,Madhavan HN, Diagnostic utility of polymerase chain reaction on intraocular specimens to establish the etiology of infectious endophthalmitis. European journal of ophthalmology. 2009 Sep-Oct; [PubMed PMID: 19787602]
Mehta S,Nagvekar V,Gupta G, Utility of 2-Deoxy-2-[18F]fluoro-Dglucose positron emission tomography/computed tomography scan in the systemic evaluation of patients with post-COVID-19 endogenous presumed fungal endophthalmitis. Indian journal of ophthalmology. 2021 Oct; [PubMed PMID: 34571657]
Ang M,Jap A,Chee SP, Prognostic factors and outcomes in endogenous Klebsiella pneumoniae endophthalmitis. American journal of ophthalmology. 2011 Feb; [PubMed PMID: 21168820]
Level 2 (mid-level) evidenceYonekawa Y,Chan RV,Reddy AK,Pieroni CG,Lee TC,Lee S, Early intravitreal treatment of endogenous bacterial endophthalmitis. Clinical [PubMed PMID: 22050564]
Level 2 (mid-level) evidenceBarza M, Treatment options for candidal endophthalmitis [editoria; comment]. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 1998 Nov; [PubMed PMID: 9827258]
Level 3 (low-level) evidenceMartínez-Vázquez C,Fernández-Ulloa J,Bordón J,Sopeña B,de la Fuente J,Ocampo A,Rubianes M, Candida albicans endophthalmitis in brown heroin addicts: response to early vitrectomy preceded and followed by antifungal therapy. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 1998 Nov; [PubMed PMID: 9827257]
Breit SM,Hariprasad SM,Mieler WF,Shah GK,Mills MD,Grand MG, Management of endogenous fungal endophthalmitis with voriconazole and caspofungin. American journal of ophthalmology. 2005 Jan; [PubMed PMID: 15652837]
Level 3 (low-level) evidencePappas PG,Kauffman CA,Andes D,Benjamin DK Jr,Calandra TF,Edwards JE Jr,Filler SG,Fisher JF,Kullberg BJ,Ostrosky-Zeichner L,Reboli AC,Rex JH,Walsh TJ,Sobel JD,Infectious Diseases Society of America., Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2009 Mar 1; [PubMed PMID: 19191635]
Level 1 (high-level) evidenceSen P,Gopal L,Sen PR, Intravitreal voriconazole for drug-resistant fungal endophthalmitis: case series. Retina (Philadelphia, Pa.). 2006 Oct; [PubMed PMID: 17031296]
Level 2 (mid-level) evidenceMarangon FB,Miller D,Giaconi JA,Alfonso EC, In vitro investigation of voriconazole susceptibility for keratitis and endophthalmitis fungal pathogens. American journal of ophthalmology. 2004 May; [PubMed PMID: 15126145]
Jørgensen JS,Prause JU,Kiilgaard JF, Bilateral endogenous Fusarium solani endophthalmitis in a liver-transplanted patient: a case report. Journal of medical case reports. 2014 Mar 24; [PubMed PMID: 24661421]
Level 3 (low-level) evidenceSmith SR,Kroll AJ,Lou PL,Ryan EA, Endogenous bacterial and fungal endophthalmitis. International ophthalmology clinics. 2007 Spring; [PubMed PMID: 17450017]
Lindstedt EW,Bennebroek CA,van der Werf DJ,Veckeneer M,Norel AO,Nielsen CC,Wubbels RJ,van Dissel JT,van Meurs JC, A prospective multicenter randomized placebo-controlled trial of dexamethasone as an adjuvant in the treatment of postoperative bacterial endophthalmitis: interim safety analysis of the study drug and analysis of overall treatment results. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2014 Oct; [PubMed PMID: 25107542]
Level 1 (high-level) evidenceLee S,Um T,Joe SG,Hwang JU,Kim JG,Yoon YH,Lee JY, Changes in the clinical features and prognostic factors of endogenous endophthalmitis: fifteen years of clinical experience in Korea. Retina (Philadelphia, Pa.). 2012 May; [PubMed PMID: 22105504]
Level 2 (mid-level) evidenceGurnani B,Kaur K, Pythium Keratitis StatPearls. 2021 Jan; [PubMed PMID: 34424645]
Gurnani B,Christy J,Narayana S,Rajkumar P,Kaur K,Gubert J, Retrospective multifactorial analysis of {i}Pythium keratitis{/i} and review of literature. Indian journal of ophthalmology. 2021 May; [PubMed PMID: 33913840]
Level 2 (mid-level) evidenceGurnani B,Narayana S,Christy J,Rajkumar P,Kaur K,Gubert J, Successful management of pediatric pythium insidiosum keratitis with cyanoacrylate glue, linezolid, and azithromycin: Rare case report. European journal of ophthalmology. 2021 Mar 28; [PubMed PMID: 33779337]
Level 3 (low-level) evidenceBalamurugan S,Das D,Hasanreisoglu M,Toy BC,Akhter M,Anuradha VK,Anthony E,Gurnani B,Kaur K, Interleukins and cytokine biomarkers in uveitis. Indian journal of ophthalmology. 2020 Sep; [PubMed PMID: 32823391]
Paulbuddhe V,Addya S,Gurnani B,Singh D,Tripathy K,Chawla R, Sympathetic Ophthalmia: Where Do We Currently Stand on Treatment Strategies? Clinical ophthalmology (Auckland, N.Z.). 2021; [PubMed PMID: 34707340]
Itoh M,Ikewaki J,Kimoto K,Itoh Y,Shinoda K,Nakatsuka K, Two Cases of Endogenous Endophthalmitis Caused by Gram-Positive Bacteria with Good Visual Outcome. Case reports in ophthalmology. 2010 Sep 21; [PubMed PMID: 21103197]
Level 3 (low-level) evidenceConnell PP,O'Neill EC,Fabinyi D,Islam FM,Buttery R,McCombe M,Essex RW,Roufail E,Clark B,Chiu D,Campbell W,Allen P, Endogenous endophthalmitis: 10-year experience at a tertiary referral centre. Eye (London, England). 2011 Jan; [PubMed PMID: 20966972]
Christy J,Jain N,Gurnani B,Kaur K, Twinkling Eye -A Rare Presentation in Neovascular Glaucoma. Journal of glaucoma. 2019 May 23; [PubMed PMID: 31135586]
Gurnani B,Kaur K,Gireesh P, Rare Coexistence of Bilateral Congenital Sutural and Cortical Blue Dot Cataracts. Journal of pediatric ophthalmology and strabismus. 2020 Jan 1; [PubMed PMID: 31972045]
Balamurugan S,Gurnani B,Kaur K,Gireesh P,Narayana S, Traumatic intralenticular abscess-What is so different? The Indian journal of radiology [PubMed PMID: 32476758]
Gurnani B,Kaur K,Sekaran S, First case of coloboma, lens neovascularization, traumatic cataract, and retinal detachment in a young Asian female. Clinical case reports. 2021 Sep; [PubMed PMID: 34484773]
Level 3 (low-level) evidenceLim HW,Shin JW,Cho HY,Kim HK,Kang SW,Song SJ,Yu HG,Oh JR,Kim JS,Moon SW,Chae JB,Park TK,Song Y, Endogenous endophthalmitis in the Korean population: a six-year retrospective study. Retina (Philadelphia, Pa.). 2014 Mar; [PubMed PMID: 24056527]
Level 2 (mid-level) evidence