Fluoroscopy Discography Assessment, Protocols, and Interpretation
Fluoroscopy Discography Assessment, Protocols, and Interpretation
Introduction
Low back pain (LBP) has been described as a global health concern with a point prevalence estimated at 7.5% of the global population, or around 577.0 million people in 2017. It has been the leading cause of years lived with disability (YLDs) at least from 1990 to 2017.[1] Chronic LBP is the second leading cause of adult disability in the United States, and its prevalence increases with age.[2]
While the ancient Greeks and Egyptians suspected a relationship between disease in the lumbar spine and leg symptoms, the modern understanding of lumbar disk herniation did not arise until the mid-1700s, and the first lumbar discectomy was performed by Mixter and Barr in 1932.[3] Discography was first described in 1948 with the early technique performed via a transdural approach. The ensuing decades have seen considerable progress from manual subjective discography to manual and automated injection manometers.[4]
Modern imaging studies, especially magnetic resonance imaging (MRI), are likely to show degeneration of multiple levels that may or may not be of any clinical significance to the presenting back and leg pain symptoms. The loss of proteoglycans from the disc gradually increases with age, especially in males, so that around 10% of 50-year-old discs and 60% of 70-year-old discs have severely degenerated. This leaves a fundamental question of what symptomatic pathology is and what is simply age-related degenerative changes of the spine.[5][6] Provocative discography is a diagnostic modality that potentially has a unique role in answering this question. It should be noted that there are two distinct forms of disc degeneration: "Endplate-driven" disc degeneration involves endplate defects and inwards collapse of the annulus showing inflammatory endplate changes and Schmorl's nodes, and "annulus-driven" disc degeneration involves a radial fissure and/or a disc prolapse, which is well described in the Modified Dallas Classification System.[7]
It has even been shown that the presence of a high-intensity zone on MRI is only a suggestive and screening indication for the diagnosis of discogenic LBP and cannot replace the gold standard of discography.[8] Pressure-controlled manometric discography using certain criteria may be the only way to distinguish asymptomatic discs among morphologically abnormal discs with Grade 3 annular tears in patients with clinical LBP, but manometry is not a mandatory requirement for discography.[9]
In addition to the disc itself, many structures can be responsible for varying degrees of axial spine pain with and without radicular features, and it may be challenging to discern which structures are involved in the clinical LBP syndrome. In addition to primary discogenic pain, which is heterogeneous in and of itself, facet arthritis, medial branch nerve entrapment, endplate edema, Schmorl's nodes, myofascial pain, spinal enthesitis, and sacroiliac joint dysfunction, to name a few, can be responsible for similar patient presentations. Provocative discography still has a role in particular cases. A "sham" injection may also have a role in teasing out non-physiologic complaints and/or obtaining insight into secondary gain issues. A discography is a diagnostic option that may link a patient’s subjective complaints of spinal pain to symptomatic disc disease when non-invasive imaging, such as MRI, does not indicate clear structural abnormalities. Post-discogram CT can also provide reasonable anatomic imaging for surgical decision-making. However, this procedure can be uncomfortable, and medical clearance should be considered in medically complex patients with cardiovascular or other high-risk comorbidities. Consideration should also be given to renal function due to the use of a radiographic contrast agent.
With a number of regenerative medicine options, such as platelet-rich plasma and other "stem cell" treatments, available and coming on the market, provocative discography is seeing an empiric use in pre-injection planning.[10] Additionally, minimally invasive intradiscal treatments, such as endoscopic diskectomy and intradiscal electrothermal procedures, often benefit from pre-procedure discograms, and/or pre-procedure discograms may be required by third-party payors.
There are 2 classifications for the discogram: the original Dallas discogram description and the modified Dallas discogram description.[11]
Original Dallas Classification System based on contrast extravasation and was originally developed in the pre-CT era. It is still noted at the time of discogram and may be used when CT scanning is not available.
This Original Classification System is graded 0-3 as follows:
- 0: no extravasation "cotton ball " appearance of the intact nucleus,
- 1: contrast into the inner annulus,
- 2: contrast into the outer annulus
- 3: contrast beyond the outer annulus, commonly running into the anterior epidural space
The Modified Dallas Classification system is based on contrast extravasation seen on coronal CT imaging through the disc itself.
There are six possible categories in the Modified Dallas Discogram Classification that describe the severity of the radial annular tear.
- Grade 0 is a normal disc—no contrast material leaks from the nucleus.
- Grade 1 tear will leak contrast material into the inner 1/3 of the annulus.
- Grade 2 tear will leak contrast through the inner 1/3 and into the middle 1/3 of the disc.
- Grade 3 tear will leak contrast through the inner and middle annulus. The contrast spills into the outer 1/3 of the annulus.
- Grade 4 tear includes a grade 3 tear, and the contrast is also seen spreading concentrically around the disc. The concentric spread must be greater than 30 degrees. A full-thickness radial tear and concentric annular tear merge together.
- Grade 5 tear ('evil' grade) includes a grade 3 or grade 4 radial tear that has completely ruptured the outer layers of the disc and is leaking contract material out of the disc. This type of tear is felt to be associated with "chemical radiculopathy," with the low pH of the nuclear material theoretically irritating nerve roots directly.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The IVD is made up of the nucleus pulposus in the center and surrounded by the annulus fibrosis and cartilaginous endplates.[12] The cartilaginous endplate is a thin layer of hyaline cartilage that firmly attaches the disc circumferentially to the vertebrae above and below and plays a role in the diffusion of nutrients into the disk.[13] The outer margin of the IVD is innervated along with the posterior longitudinal ligament by fibers of the sinuvertebral nerve.
A healthy IVD is poorly innervated and is supplied only by sensory and sympathetic perivascular nerve fibers, which are usually found in the periphery of the annulus fibrosus.[14] This innervation pattern is relevant in discography, noting that Grade 0-3 Dallas Classification may potentially be painless, whereas some Grade 3 and all Grade 4 or 5 should be painful.
The vertebral body itself has scarce innervation, which is largely found to be perivascular.[15] Vertebral endplates in pathologic "endplate-driven" degeneration are more richly innervated than intervertebral disc pathologies in terms of immunoreactive nerve fibers and immunoreactive cells.[16]
With age, the height of the disk may be reduced, and the endplates may become irregular with Modic endplate changes as part of endplate-driven degeneration.[17] The role of provocative discography in endplate-driven degeneration is unclear at this time. The combination of loss of IVD height and loss of endplate definition, alone or in conjunction with facet hypertrophy, means that not every disk may be amenable to provocative discography.
Indications
- A high index of suspicion for primary discogenic pain is severe enough to consider surgical intervention and/or pain management techniques directed at the disc. Possible interventions include endoscopic discectomy, electrothermal therapy, or posterior annular zone radiofrequency ablation.
- When pain is not responding to conservative modalities, has persisted for at least 3 months, and is occurring with no evidence of contraindications such as severe spinal stenosis, infection, or psychogenic pain.
- To distinguish between painful pseudoarthrosis or a symptomatic disc in a posteriorly fused segment.
- To assess disc before spinal fusion.[18]
While provocative discography is mostly considered when surgical intervention is considered as an option, it may also have diagnostic value in pain syndromes that may overlap with potential visceral origins, such as atypical abdominal or pelvic pain.
Contraindications
Absolute contraindications specific to lumbar discography:
- Previously fused intervertebral body at that level
- Cord or cauda equina/conus medularis compression at the level of the intended diskography
- Active systemic infection or infection/cellulitis of the skin overlying or deep to the skin entry site
- Known or suspected infectious discitis
- Posterolateral/transverse fusion to the point that disk entry is not possible
Contraindications to similar interventional pain management procedures:
- Uncontrolled bleeding disorder or anticoagulation therapy
- Pregnancy
- Allergy to iodine contrast (gadolinium can be used in such cases)
- Severe renal insufficiency
- Medical instability from a cardiovascular standpoint, i.e., unstable angina, uncontrolled hypertension such that any degree of discomfort may precipitate acute cardiovascular events such as arrhythmia or ischemia
- The outcome/result of the diagnostic procedure will have no bearing on clinical course/treatment.
- The specific need for discography to be done with manometer readings and manometer unavailable
Contraindications to any other procedure or healthcare:
- Patient unable or unwilling to consent
- Patient not competent to consent and no medical power of attorney available
- Uncontrolled/untreated psychiatric conditions
Equipment
Provocative Diskogram Equipment List
- Fluoroscopic C-arm x-ray device, mobile or fixed unit with an adequately trained radiology technician
- Lead aprons for all persons in the room
- At least one circulating medical assistant capable of basic assistance
- Several 18-gauge, 1 or 1.5-inch needles
- 25 or 27-gauge 1.5 or longer needle for local anesthesia infiltration for skin and deeper tissue
- 22-gauge, 5 or 7-inch needle for disk entry
- Local anesthetic (lidocaine or bupivacaine)
- Injectable antibiotics, usually second-generation cephalosporin, e.g., cefazolin. Alternative if the patient is allergic.
- Myelogram grade contrast agent. Can use gadolinium if the patient is allergic to iodine contrast.
- Pregnancy testing, if applicable
- Sterile gloves and drapes
- Short IV-extension tubing
- Chlorhexidine gluconate or another equivalent sterile antiseptic solution
- Sterile drape
- Sterile gauze
- If manometry is needed: manometer and attachments commonly come in the sterile one-piece boxed kit, depending on the manufacturer.
- If performing difficult L5/S1 entry: 18-gauge 5-inch spinal needle and 22-gauge 7-inch spinal needle, or 25-gauge 6-inch needle and a 20-gauge 3.5-inch introducer needle.
If performing light intravenous sedation:
- Standard monitoring with EKG, SpO2, NIBP
- Drugs for sedation (e.g. short-acting benzodiazepine such as midazolam)
- Designated trained personnel to monitor and record sedation
- Adequate resuscitative equipment, usually a "code-cart" with the reversing agent(s) to be able to manage and/or reverse sedation and/or manage any potential complications of the sedation itself
If obtaining post-discogram CT:
- CT scanner
- Arrangements and transportation to CT scanner
Personnel
- The physician performing the discogram.
- Radiology technician to manage the C-arm (and CT if post-discogram CT is utilized).
- At least one circulating medical assistant.
- Transporter/escort if the patient needs to be transferred to CT for post-discogram imaging.
- If performing IV sedation:
- Designated trained observer to monitor and record vital signs. If this person is actively administering the medications at the designated time and by physician order, they will need to be a nurse of anesthesia provider based on the state's rules and regulations and the institutional policy of the site of service.
- Personnel adequate for resuscitation when and if needed in response to medication reaction, respiratory or cardiac arrest.
Preparation
Risks, benefits, and potential alternatives, including the elective and diagnostic nature of the procedure, need to be reviewed with the patient. Ideally, this should have been discussed prior to the day of the procedure in an office setting without the stress of the impending procedure. The patient should have adequate opportunity and time to ask questions, and the proceduralist should explain the procedure with images and/or spine models.
If the patient is a female of child-bearing age, a negative pregnancy test or waiver should be obtained.
The clinician should review anti-coagulation and/or antiplatelet therapy and review PT or INR, if applicable. The clinician should review cardiac and/or other medical clearance if indicated.
IV access is obtained for light sedation and/or IV antibiotic administration. Non-invasive monitoring is obtained: EKG, NIBP, SpO2, and baseline vitals are obtained and found to be acceptable for the procedure. The patient is placed in a prone position on the fluoroscopy table. The lumbar region is marked with a skin marker.
A standard "time-out" is called. The correct patient, location, and procedure are verified. If a post-discogram CT is being performed, the location and time en route of transport to CT are confirmed before skin prep.
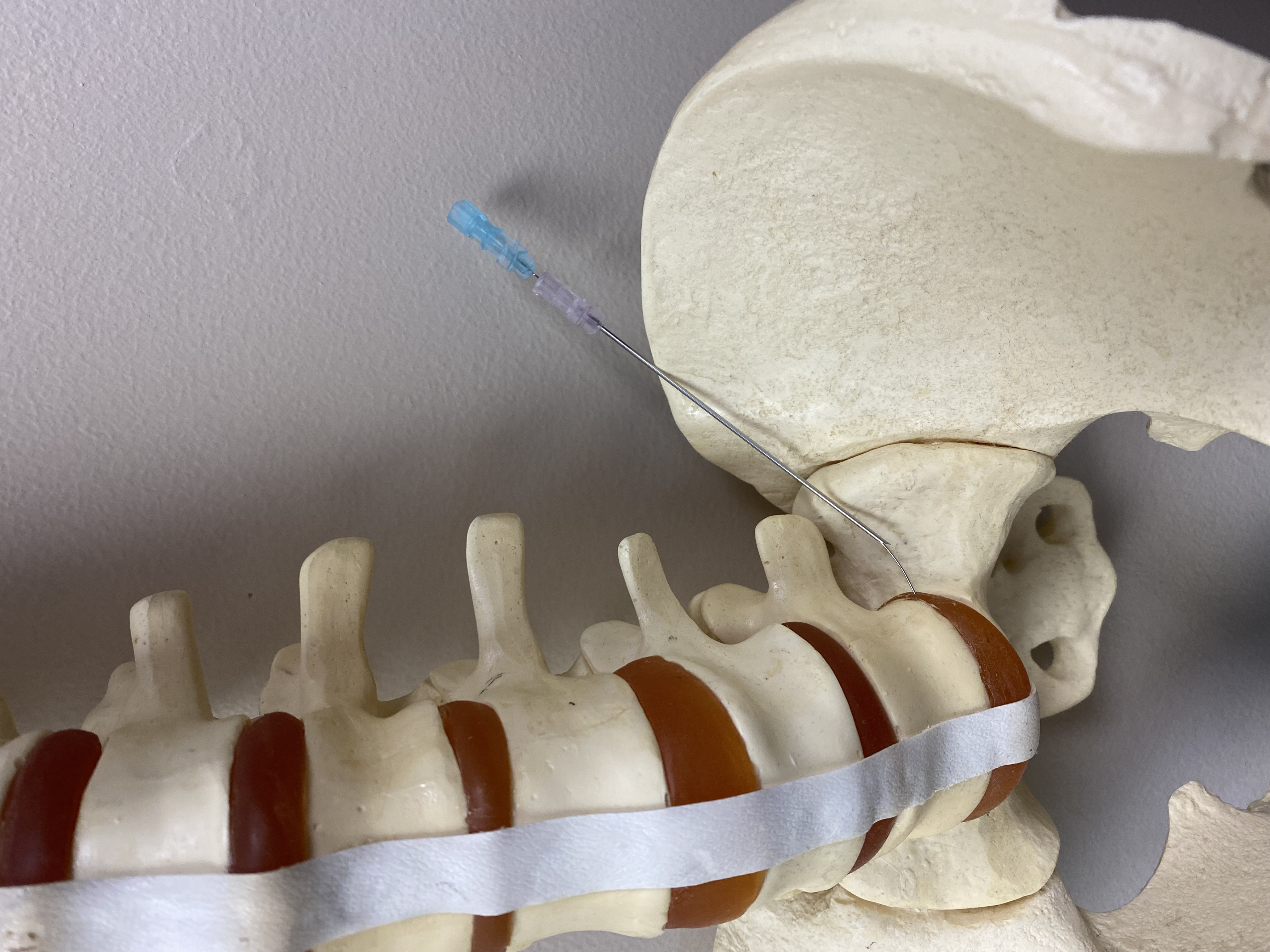
The L5/S1 is the most difficult location, especially in males, due to the higher iliac crest and narrower sacrum. It is not uncommon to take initial images before skin prep and potentially side-bend the patient away from the entry side and even cross the leg over the other. It may be necessary to bend the knee 90 degrees and cross it over the back of the contralateral knee. If such maneuvers are to be employed, it is best to know this before sterile prepping and draping.
Before sterile prepping, the patient position is verified so that the C-arm has adequate space to angle lateral and oblique without hitting or having radiopaque parts of the table get in the way of the beam.
The antibiotic, if used, is usually reconstituted into 10 ml of 0.9% normal saline (e.g., cefazolin 1 g in 10 ml gives a solution of 100 mg/ml). Commonly, 9 ml are given to the patient IV, and the other 1ml (100 mg) is placed into 10 ml of contrast agent with all springes are labeled. It should be noted that there is currently no consensus regarding the use of prophylactic antibiotics for the prevention of discitis.[19]
Procedure room personnel should don lead aprons. The proceduralist should don sterile gloves.
If manometry is being used, the transducer, contrast syringe, and extension tubing are all one piece in a kit, depending on the manufacturer.
A short IV-extension tubing is attached to the syringe labeled contrast, and it is primed with contrast removing all air in the tubing.
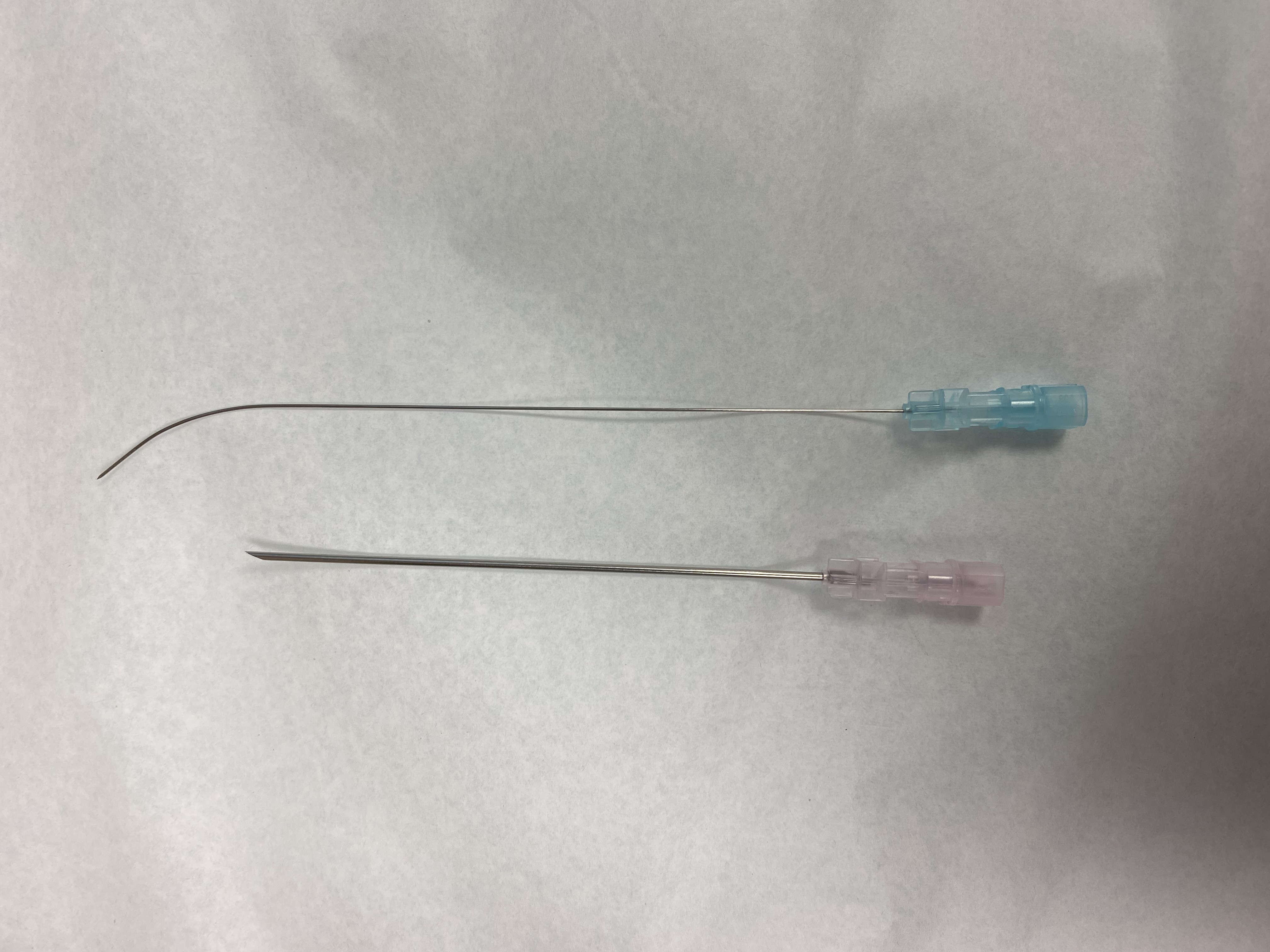
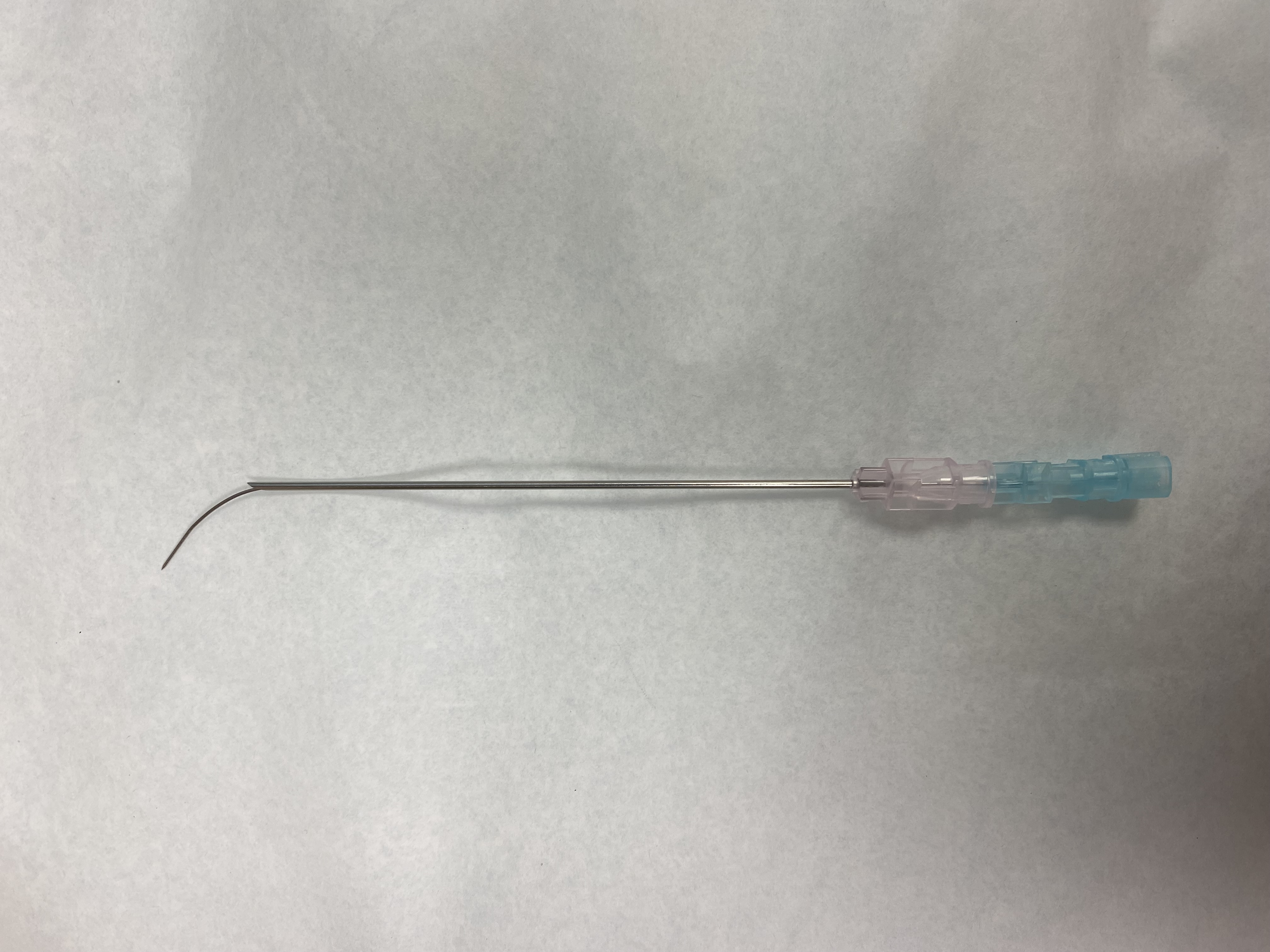
Optional: 22-gauge, 7-inch needle used for disc entry can be given a distal curved bend in the plane of the bevel. It is then inserted through the 3.5 or 5 inches larger bore needle just up to the tip so that the 7-inch needle can be pushed through the distal end of the shorter larger needle to deploy medially towards the disk once the shorter needle is in place. (see image)
Technique or Treatment
With preparation complete and the patient prone position. A standard “time-out” is performed. The skin mark on the lumbar spine is identified. Not every disc can be entered bilaterally. The side on which the physician stands is a matter of right- or left-handedness, personal choice, room set-up, and equipment set-up flexibility.
The patient is prepped with Chloraprep and draped in the usual sterile fashion using a fenestrated drape. A radiopaque marker is placed about mid-region on the lumbar spine as a point of reference. A single anteroposterior (AP) view is commonly performed. The first level intended to be injected is noted. Next, the C-arm is tilted towards or away from the head to line up the endplates of the intended vertebral level. The radiopaque marker is often moved to be more in line with the entry point if the initial estimate is off point. The C-arm is then angled towards the side of the skin entry. An image is obtained to align the anterior edge of the superior articular process with the mid-portion of the disc. Depending on lateral disk collapse, rotation of the vertebral body, and/or scoliosis, the C-arm angles may need to be adjusted. It may be necessary to switch back and forth between AP, lateral, and oblique views for the best estimate of this entry point.
Care should be taken not to enter too far lateral, such as in cases where the vertebra is rotated anterior on that side. In such cases, contralateral disk entry should be considered. Skin anesthesia is accomplished with a local anesthetic, usually lidocaine without epinephrine. An 18-gauge 1 or 1.5-inch needle is initially inserted through the skin in the track towards the center of the disk, and then the 22-gauge 5 or 7 inches needles with or without a bent-tip are inserted through the 18-gauge needle in a "needle-over-needle" technique. Additional lidocaine is administered for infiltration as needed. When the needle is at the outer annulus of the disk on AP and lateral views, the patient is informed that they will feel some discomfort. The needle should have a "rubbery feel" as it comes up against and enters the annulus. The needle is then advanced in the center of the nucleus.
At this point, the C-arm is usually rotated to a lateral view, magnification visualizing the anterior and posterior aspect of the disk and spinal canal is obtained. The stylet is removed from the needle while not advancing or retracting the needle. The cap on the end of the short IV extension of the contrast syringe is removed and attached to the needle that is in the disc. The physician is now ready for the provocative portion of the discogram. Multiple "sham" injections are usually performed. The syringe is held and sometimes even tapped while asking the patient if they feel anything. If a pain response is elicited at this stage, it should be noted as a sham response. Otherwise, pain provocation at this stage should not occur.
If using manometry, the manometer should read zero pressure and zero volume at this point.
Verbal communication is essential. The patient should be made aware that they are going to feel pressure and potentially pain. There is a subjective, almost artistic component to this phase. Every physician will have their own way of interpreting and asking what happens next, but some suggestions/examples are as follows:
- "OK, here is the part we discussed. Tell me when you feel something." At this point, a tapping or other gentle movement for a sham injection is performed. Then, slow pressure and observation of the disc on the lateral view, usually with magnification, is performed.
- "OK, I know that hurts, and I'm sorry about that, but is it the same pain or different?" The patient response or answers are noted.
- "Is that the same pain that you have when it hurts? Is that the same pain that brought you in to see us in the first place?" The patient response or answers are noted
Under real-time fluoroscopy, the contrast is administered, and initial flow into the disc is noted. If using a manometer, the opening pressure and volume are noted. Pressure and gradually increased, and pain location and intensity are noted. The terms concordant and discordant are often used. The volume at which pain may change from concordant to discordant is noted if such a change occurs. While a manual discogram has no pressure transducer, volumes can still be reasonably noted at different times of the procedure. Likewise, manometer volumes and pressures are noted as well. Basic Dallas classification I-IV should be possible to discern on the lateral view, especially later on diagnostic quality lateral plain films.
It is important to finish one level before moving on to the next and not confuse data from one disc with another. Many clinicians inject a small amount (e.g., 0.5 ml) of bupivacaine into the most painful discs for post-procedure palliation. As with any spinal injection, caution should be exercised to avoid inadvertent vascular uptake.
Upon completion of the series, the final AP and lateral view are taken, covering all discs. The sterile skin prep solution is cleaned off the patient. A dry sterile dressing is applied after hemostasis is obtained with direct pressure. The IV is discontinued only after the patient is off the table and stable in the post-procedure suite.
The concept is the same if using a biplane unit or two C-arms set up at 90 angles. An oblique view may not be available based on the equipment, and the AP and lateral views may need to be taken together. The clinician would need to conceptualize the three-dimensional image this creates. This is a separate skill that the proceduralist should be familiar with before attempting.
Complications
While complications of discography are rare, there are the risks of:
- Discitis
- Meningitis
- Nerve root injury
- Superficial infection
- Skin irritation from prep solution
- Medication reaction
- Sequelae of the cardiovascular stress of the procedure
- Renal injury from contrast (late effect)
- Vascular injury
- Bleeding
- Increased pain
- Disc herniations
While the patient needs to be able to interact with the proceduralist, light sedation is commonly provided. However, it carries its own risks and complications of medication reaction and oversedation with respiratory and/or cardiac complications.
Clinical Significance
When performed by a skilled physician, provocative discography is a safe, if not uncomfortable, adjunctive diagnostic procedure that may be of use in the evaluation and workup of axial spine pain with and without radiculopathy. A post discogram CT scanning may provide reasonable alternative imaging in MRI-incompatible patients and, in some cases, is the gold standard over MRI in diagnosis posterior annular tears.[20]
It is imperative to note that discography is diagnostic, not therapeutic. The role of provocative discography role is unclear in "endplate-driven" degeneration. Unnecessary surgery, especially unnecessary fusion fixation of vertebral segments, may potentially be avoided.
Enhancing Healthcare Team Outcomes
With the worldwide burden of LBP clearly documented, it is an important medical topic and can be thought of as almost a public health crisis. With LBP being a clinical syndrome with heterogeneity in terms of presentations, etiologies, histories, and exam findings, objective information is always needed. Finding the appropriate vertebral levels involved in a patient's symptoms can allow for better outcomes and determines the appropriate course of treatment, workup, management, evaluation, and decision-making process regarding lumbar spine surgery, particularly fusion.
For improved outcomes, interactions between spine surgeons, neurologists, interventional pain management physicians, as well as physical therapists, and other allied health professionals can and should include data obtained during provocative discography and post-discogram CT scanning. This is important to plan surgeries, minimally invasive procedures, and therapies for the patient. Primary care physicians and physician extenders are crucial in obtaining an initial history and physical exams, emphasizing common "red flag" symptoms and neurological deficits.[21]
In the initial post-procedure period, pain control and monitoring for any post-procedural complications should consist of basic neuro checks and vital signs. Although rare, later monitoring should consist of observation for constitutional signs or symptoms of fevers, chills, and increasing LBP. Restarting anticoagulation and/or antiplatelet therapy under appropriate guidance may be indicated depending on the clinical scenario. Clinical follow-up should include actually reviewing the objective and subjective data obtained from the discograms as part of integrated care.
In general, the need for meticulous planning and discussion with other professionals involved in managing the patient is highly recommended to lower the rate of complications and improve clinical outcomes.
Nursing, Allied Health, and Interprofessional Team Interventions
Nursing, allied health, and other team members need to engage in basic standard-of-care for outpatient post-procedural monitoring and sterile technique during the procedure. This includes basic assistance with set-up and preparation similar to many other outpatient pain management interventional procedures. Antibiotics and light sedation are usually given intravenously, and some of the antibiotics may be mixed with the contrast agent.
Team interventions should include capability and protocols for handling any medical emergency either during or post-procedure.
Post-procedural nursing care, whether it be in a post-procedure area, post-anesthesia care unit, or return to a regular medical floor, is similar to many other pain management procedures such as epidural steroid injection. This should include vital signs, neurological checks for any new focal weakness, adequate pain control, and observation for potential late reactions to medications. A greater number of these patients may be MRI incompatible due to implanted cardiac devices and henceforth have a higher risk of postprocedure acute cardiac events. There should be a comparatively low threshold in such patients to notify the physician of chest pain, shortness of breath, or any other unusual symptoms that could be an anginal equivalent or otherwise signal of clinical decline.
Nursing, Allied Health, and Interprofessional Team Monitoring
Nursing or medical assistant postprocedure monitoring should include basic patient observation, including vital signs and notification of the physician of any deterioration and patient status. Because the patient may have received light sedation with a benzodiazepine or opioid for the procedure, reversal protocols should be implemented, and resuscitation equipment should be readily available in case of an emergency.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
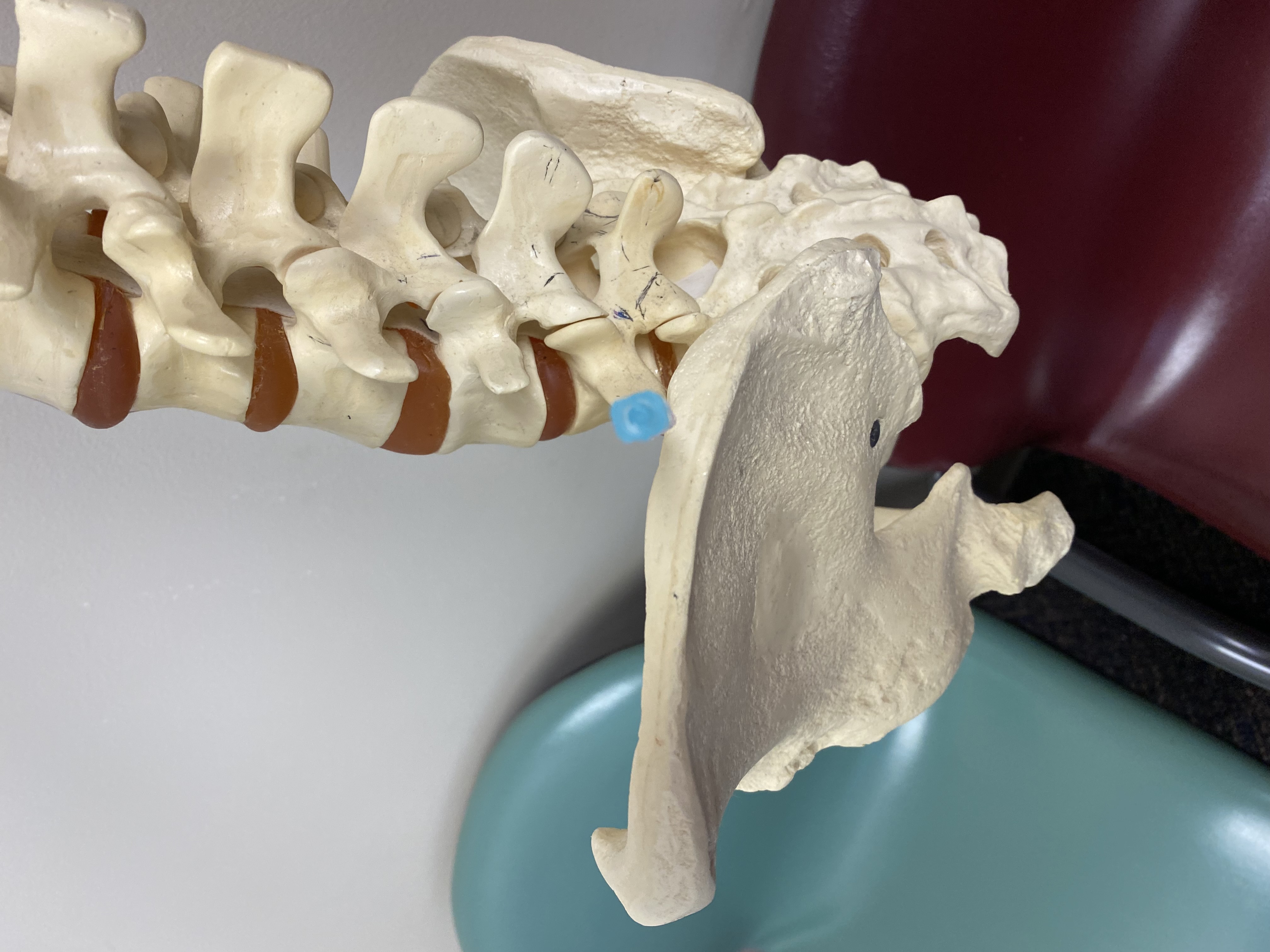
The iliac crest may require the initial entry to be high, above the inferior endplate of the L5 vertebra and/or too far anterior to enter the center of the disc at L5/S1 and, potentially, in cases of a very high sacrum with loss of the height of the disc spaces and vertebral bodies even the L4/5 disc space
Contributed by Michael F. Stretanski
References
Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, Blyth FM, Smith E, Buchbinder R, Hoy D. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Annals of translational medicine. 2020 Mar:8(6):299. doi: 10.21037/atm.2020.02.175. Epub [PubMed PMID: 32355743]
Gooch CL, Pracht E, Borenstein AR. The burden of neurological disease in the United States: A summary report and call to action. Annals of neurology. 2017 Apr:81(4):479-484. doi: 10.1002/ana.24897. Epub [PubMed PMID: 28198092]
Truumees E. A history of lumbar disc herniation from Hippocrates to the 1990s. Clinical orthopaedics and related research. 2015 Jun:473(6):1885-95. doi: 10.1007/s11999-014-3633-7. Epub [PubMed PMID: 24752913]
Derby R, Lee SH, Lee JE, Lee SH. Comparison of pressure-controlled provocation discography using automated versus manual syringe pump manometry in patients with chronic low back pain. Pain medicine (Malden, Mass.). 2011 Jan:12(1):18-26. doi: 10.1111/j.1526-4637.2010.00990.x. Epub 2010 Oct 28 [PubMed PMID: 21040439]
Level 2 (mid-level) evidenceSivakamasundari V, Lufkin T. Bridging the Gap: Understanding Embryonic Intervertebral Disc Development. Cell & developmental biology. 2012 May:1(2):. pii: 103. Epub [PubMed PMID: 23106046]
Level 3 (low-level) evidenceRaj PP. Intervertebral disc: anatomy-physiology-pathophysiology-treatment. Pain practice : the official journal of World Institute of Pain. 2008 Jan-Feb:8(1):18-44. doi: 10.1111/j.1533-2500.2007.00171.x. Epub [PubMed PMID: 18211591]
Adams MA, Dolan P. Intervertebral disc degeneration: evidence for two distinct phenotypes. Journal of anatomy. 2012 Dec:221(6):497-506. doi: 10.1111/j.1469-7580.2012.01551.x. Epub 2012 Aug 12 [PubMed PMID: 22881295]
Wang H, Li Z, Zhang C, Zhang W, Li L, Guo J, Wu W, Hou S. Correlation between high-intensity zone on MRI and discography in patients with low back pain. Medicine. 2017 Jul:96(30):e7222. doi: 10.1097/MD.0000000000007222. Epub [PubMed PMID: 28746177]
Derby R, Kim BJ, Lee SH, Chen Y, Seo KS, Aprill C. Comparison of discographic findings in asymptomatic subject discs and the negative discs of chronic LBP patients: can discography distinguish asymptomatic discs among morphologically abnormal discs? The spine journal : official journal of the North American Spine Society. 2005 Jul-Aug:5(4):389-94 [PubMed PMID: 15996608]
Levi D, Horn S, Tyszko S, Levin J, Hecht-Leavitt C, Walko E. Intradiscal Platelet-Rich Plasma Injection for Chronic Discogenic Low Back Pain: Preliminary Results from a Prospective Trial. Pain medicine (Malden, Mass.). 2016 Jun:17(6):1010-22. doi: 10.1093/pm/pnv053. Epub 2015 Dec 26 [PubMed PMID: 26814283]
Sachs BL, Vanharanta H, Spivey MA, Guyer RD, Videman T, Rashbaum RF, Johnson RG, Hochschuler SH, Mooney V. Dallas discogram description. A new classification of CT/discography in low-back disorders. Spine. 1987 Apr:12(3):287-94 [PubMed PMID: 2954226]
Palepu V, Kodigudla M, Goel VK. Biomechanics of disc degeneration. Advances in orthopedics. 2012:2012():726210. doi: 10.1155/2012/726210. Epub 2012 Jun 17 [PubMed PMID: 22745914]
Level 3 (low-level) evidenceMoore RJ. The vertebral endplate: disc degeneration, disc regeneration. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2006 Aug:15 Suppl 3(Suppl 3):S333-7 [PubMed PMID: 16816945]
García-Cosamalón J, del Valle ME, Calavia MG, García-Suárez O, López-Muñiz A, Otero J, Vega JA. Intervertebral disc, sensory nerves and neurotrophins: who is who in discogenic pain? Journal of anatomy. 2010 Jul:217(1):1-15. doi: 10.1111/j.1469-7580.2010.01227.x. Epub 2010 Apr 26 [PubMed PMID: 20456524]
Buonocore M, Aloisi AM, Barbieri M, Gatti AM, Bonezzi C. Vertebral body innervation: Implications for pain. Journal of cellular physiology. 2010 Mar:222(3):488-91. doi: 10.1002/jcp.21996. Epub [PubMed PMID: 20020509]
Ohtori S, Inoue G, Ito T, Koshi T, Ozawa T, Doya H, Saito T, Moriya H, Takahashi K. Tumor necrosis factor-immunoreactive cells and PGP 9.5-immunoreactive nerve fibers in vertebral endplates of patients with discogenic low back Pain and Modic Type 1 or Type 2 changes on MRI. Spine. 2006 Apr 20:31(9):1026-31 [PubMed PMID: 16641780]
Viswanathan VK, Shetty AP, Rajasekaran S. Modic changes - An evidence-based, narrative review on its patho-physiology, clinical significance and role in chronic low back pain. Journal of clinical orthopaedics and trauma. 2020 Sep-Oct:11(5):761-769. doi: 10.1016/j.jcot.2020.06.025. Epub 2020 Jun 18 [PubMed PMID: 32879563]
Level 3 (low-level) evidenceWalker J 3rd, El Abd O, Isaac Z, Muzin S. Discography in practice: a clinical and historical review. Current reviews in musculoskeletal medicine. 2008 Jun:1(2):69-83. doi: 10.1007/s12178-007-9009-9. Epub [PubMed PMID: 19468876]
Sharma SK, Jones JO, Zeballos PP, Irwin SA, Martin TW. The prevention of discitis during discography. The spine journal : official journal of the North American Spine Society. 2009 Nov:9(11):936-43. doi: 10.1016/j.spinee.2009.06.001. Epub 2009 Jul 29 [PubMed PMID: 19643677]
Lam KS, Carlin D, Mulholland RC. Lumbar disc high-intensity zone: the value and significance of provocative discography in the determination of the discogenic pain source. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2000 Feb:9(1):36-41 [PubMed PMID: 10766075]
Verhagen AP, Downie A, Popal N, Maher C, Koes BW. Red flags presented in current low back pain guidelines: a review. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2016 Sep:25(9):2788-802. doi: 10.1007/s00586-016-4684-0. Epub 2016 Jul 4 [PubMed PMID: 27376890]