Continuing Education Activity
Poststreptococcal glomerulonephritis (PSGN) results from a bacterial infection that causes rapid deterioration of the kidney function due to an inflammatory response following streptococcal infection. PSGN most commonly presents in children 1 to 2 weeks after a streptococcal throat infection, or within 6 weeks following a streptococcal skin infection. When symptomatic, PSGN typically presents with features of the nephritic syndrome such as hematuria, oliguria, hypertension, and edema, though it can also present with significant proteinuria. This activity reviews the etiology, pathogenesis, evaluation, and management of PSGN and explains the role of the interprofessional team in evaluating and treating patients with this condition.
Objectives:
Identify the epidemiology, etiology, pathophysiology of poststreptococcal glomerulonephritis.
Review how to evaluate a patient for poststreptococcal glomerulonephritis.
Summarize the treatment and management options available for poststreptococcal glomerulonephritis.
Explain interprofessional team strategies for improving care coordination and communication to improve outcomes for patients affected by poststreptococcal glomerulonephritis.
Introduction
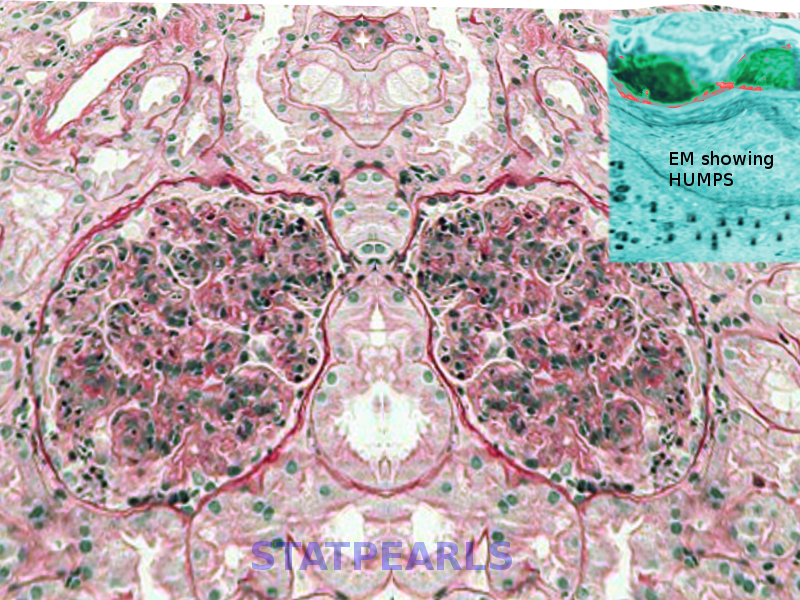
Poststreptococcal glomerulonephritis (PSGN) is characterized by rapid deterioration of kidney functions due to an inflammatory response (type III hypersensitivity reaction) following streptococcal infection (See Image. Poststreptococcal glomerulonephritis). This condition results from specific strains of group A beta-hemolytic streptococci called nephrogenic streptococci. The disease affects the glomeruli and the small blood vessels of the kidneys. PSGN most frequently presents in children 1 to 2 weeks after a sore throat, or 6 weeks after a skin infection (impetigo).[1]
Though the incidence of PSGN has declined in developed countries, the incidence of non-streptococcal organisms is emerging. Nephritis-associated plasmin receptor (NAPlr) and streptococcal pyrogenic exotoxin B (SPeB) are the two common antigens associated with the pathogenesis of PSGN. They not only activate the alternate complement pathway, resulting in hypocomplementemia, but they also have an affinity towards the plasmin and glomerular proteins. The clinical presentation of PIGN can vary from no symptoms to renal failure requiring renal replacement therapy (RRT). [2]
When symptomatic, PSGN typically presents with features of the nephritic syndrome such as hematuria, oliguria, hypertension, and edema. Less commonly presentation can mimic nephrotic syndrome with significant proteinuria.
Etiology
Nephrogenic streptococci infection precedes PSGN, which initially affects skin or the oropharynx. More recently, PSGN is associated with skin infections (impetigo) more frequently than throat infections (pharyngitis).[3][4]
Group A Streptococcus (GAS) has been subtyped depending on the surface M protein and opacity factor, which are known to be nephrogenic and can cause PSGN. Other causes of post-infectious glomerulonephritis include bacterial infections including endocarditis, enterocolitis, pneumonia, and intraventricular shunt infections, viral (hepatitis B and C infections, human immunodeficiency virus, cytomegalovirus, Epstein Barr virus, parvovirus B19), fungal (coccidioidomycosis, histoplasmosis), and parasitic infections (malaria, leishmania, toxoplasmosis, and schistosomiasis).[5]
Poor hygiene, overcrowding, and low socioeconomic status are important risk factors for streptococci outbreaks, and this explains the higher incidence of PSGN in impoverished countries. Genetic factors are expected to predispose to the condition since almost 40% of patients with PSGN gave a positive family history. There is no specific gene found to cause PSGN.[5]
Epidemiology
Over the past three decades, PSGN incidence has significantly dropped in developed countries; such as the United States, UK, Central Europe, and Japan. The reason for this progress is the use of antibiotic prophylaxis and the improvement of hygienic states. In these developed countries, PSGN has become more frequently seen in adult patients who suffer from chronic debilitating diseases.[6]
Higher incidence of PSGN in developing countries- due to increased skin infections (pyoderma). Though the incidence in developed countries has gone down, it is still the most common cause of glomerulonephritis (GN) in children in the united states. [5]
PSGN is also the most common cause of kidney injury in children in the Middle East, Africa, Australia, and worldwide. The annual incidence of new cases of PSGN in developing countries ranges from 8.5 to 28.5 per 100000 individuals.[7] Around 97% of cases reported with PSGN live in underprivileged countries.
Clinically manifestations of PSGN are more common in males than in females with a ratio of 2:1. However; the incidence of subclinical PSGN is almost equal in both sexes. Racial factors were not found to play a role. The disease most frequently affects children between the age of 3 and 12 (with the peak incidence between 5 to 6 years), and seniors greater than 60 years old.
Pathophysiology
The disease is immunological; representing a type III hypersensitivity reaction. The exact mechanism by which PSGN occurs is not fully determined. The body responds to nephrogenic streptococcal infection by forming immune complexes containing the streptococcal antigen with a human antibody.[2] Some theories suggest that these immune complexes become deposited in kidney glomeruli reaching through the circulation. Others claim that the condition results from an “in situ” formation of the antigen-antibody complex within the kidney glomeruli. This “In situ immune complex formation” is either due to a reaction against streptococci antigens deposited in the glomerular basement membrane or, according to other theories, due to an antibody reaction against glomerular components that cross-react with streptococcal antigen due to molecular mimicry.[5]
The presence of immune complexes leads to the activation of the alternate complement pathway causing infiltration of the leukocytes, and proliferation of the mesangial cells in the glomerulus thus impairing the capillary perfusion and glomerular filtration rate (GFR). Reduction in GFR can lead to renal failure (oliguria or anuria), acid-base imbalance, electrolyte abnormalities, volume overload, edema, and hypertension.
Histopathology
- Light microscopy- The glomeruli show hypercellularity (endothelial, mesangial, and inflammatory cells) which are non-specific.
- Electron microscopy- The most characteristic finding is the presence of sub-epithelial humps; which are electron-dense deposits in the subepithelial space near the glomerular basement membrane.[8]
- Immunofluorescence microscopy- Evidence of IgG and C3 deposits in the first 2 to 3 weeks of the disease.
History and Physical
Approximately 50% of children with PSGN are asymptomatic and are discovered accidentally during routine urine analysis. The classic triad of glomerulonephritis includes hematuria, edema, and hypertension. Typically, patients give a history of a recent streptococcal infection such as pharyngitis, tonsillitis, or impetigo. However; some patients develop PSGN without experiencing symptoms of respiratory tract infection or pyoderma, which can be a diagnostic challenge.[9]
The most common presenting symptom is gross hematuria as it occurs in 30 to 50% of cases with acute PSGN; patients often describe their urine as smoky, tea-colored, cola-colored, or rusty. The hematuria can be described as postpharyngitic (hematuria seen after weeks of infection).
Renal involvement is common and is transient with recovery in 1-2 weeks. Less than half of the patients experience oliguria. Depending on the severity of renal involvement, signs, and symptoms suggestive of anuric renal failure or life-threatening acid-base imbalance, electrolyte abnormalities (especially hyperkalemia), and fluid overload would require RRT. About 60-80% of the patients experience high blood pressure which typically resolves in 10 days. [5]
The incidence of edema is seen in about 65-90% of the cases. Puffiness of the eyelids (periorbital edema) is typical for the nephritic syndrome. It is most prominent in the morning and tends to resolve at the end of the day. Generalized edema is also a common feature. Moreover, in severe cases, patients might experience respiratory distress as a result of pulmonary edema. They may experience other non-specific symptoms like anorexia, malaise, nausea, vomiting, etc.
Evaluation
PSGN should be suspected in all children with hypertension and heart failure, even in the absence of hematuria or a history of a preceding sore throat or pyoderma.
Laboratory investigations are the most useful in PSGN assessment.
- Evidence of a preceding streptococcal infection is determined by measuring anti-streptolysin titer (ASO), and anti-nicotinamide-adenine dinucleotidase (anti-NAD) which tend to rise following pharyngitis. Other antibodies such as anti-DNAse B and anti-hyaluronidase (AHase) are usually elevated after both pharyngitis and skin infections. ASO titer is the most frequently used test, while the most sensitive is the streptozyme test; which includes measuring the titers of all the antibodies mentioned above. ASO titers can be falsely low in patients treated with antibiotics for streptococcal infections.
- Serum complement level (C3) is usually low due to its consumption in the inflammatory reaction. Mostly, the decrease in C3 concentration occurs before serum ASO has risen.[5] Complement levels usually return to normal levels in 6-8 weeks.
- Urine analysis: shows macroscopic or microscopic hematuria, RBC casts, mild proteinuria. Only 5% of patients with PSGN have massive proteinuria that indicates nephrotic syndrome. White blood cell casts, hyaline, and cellular casts are usually present in the urine analysis.
- Renal Function Tests: Blood urea nitrogen (BUN) and serum creatinine typically elevate during the acute phase. These values usually return to normal later.
- In patients with heart failure and PSGN, NT-proBNP levels are elevated along with the findings of pulmonary congestion on the chest x-ray.
Renal biopsy is not recommended for diagnosing patients with PSGN and is performed only when other glomerular pathologies are suspected. Renal biopsy is indicated when:
- Progressive decline in the Renal function
- Anuric renal failure
- When there is no latent period between the acute glomerulonephritis and streptococcal infection
- If the complement levels are normal
- When there is no rise in antistreptococcal antibodies
Imaging Studies
- Ultrasonography: Kidneys are enlarged only in a few patients.
- The chest x-ray may show pulmonary congestion in patients with symptoms consistent with volume overload or heart failure.
Treatment / Management
PSGN is a self-limiting condition in most cases, and thus only symptomatic treatment is needed. Supportive treatment aims at controlling the complications of volume overload such as hypertension and edema, which are prominent during the acute phase of the disease.[5]
Pharmacological Therapy
Antimicrobials: Patients with evidence of a streptococcal infection should receive a course of antibiotic therapy, and they may not prevent the development of PSGN.
Diuretics: Loop diuretics (furosemide) are preferred over thiazides (hydrochlorothiazide or chlorthalidone). The efficacy of thiazide diuretics is very minimal when GFR < 30 ml/min.
Antihypertensive medications: Blood pressure can be managed by restricting salt and fluid intake along with diuretics are needed. In cases with uncontrolled blood pressure, the use of calcium channel blockers is recommended. The use of angiotensin-converting enzyme inhibitors (ACEI), angiotensin receptor blockers (ARBs) is recommended in patients with stable GFR and with near-normal potassium levels.
Immunosuppressive therapy: There’s no evidence that immune suppression is useful in patients with PSGN.[10]However, patients with progressive renal failure or the presence of crescents on the renal biopsy may warrant the use of corticosteroids.[11][11][11]
Dialysis
Dialysis is only performed to manage the acid-base balance, electrolyte abnormalities (especially hyperkalemia), and fluid management
General measures
- Salt and water restriction to treat the edema.
- Bed rest and immobilization are recommendations in the first few days of the disease.
- Throat cultures on the patient and family members are important.
- All affected members need to be treated with penicillin or erythromycin.
Differential Diagnosis
- IgA Nephropathy: usually occurs after an upper respiratory tract or gastrointestinal infection, but it differs from PSGN in the shorter latency period it takes to appear after the episode of infection. It can also be described as synpharyngitic hematuria- hematuria and infection coincide.
- Membranoproliferative glomerulonephritis: also presents with a nephritic picture and hypocomplementemia following respiratory tract infection. Complement levels take a longer time to return to normal than in PSGN or persistently low C3 levels.
- Lupus nephritis: sometimes PSGN presents with a picture similar to lupus nephritis. Laboratory testing for antibodies specific to each of the diseases can help in the diagnosis. Positive ANA, ds-DNA, cytopenia, and multi-organ involvement.
- Nephrotic syndrome: 24-hour urine protein excretion is more than 3.5 gram/day along with hypoalbuminemia, edema, hypogammaglobulinemia, and increased risk of thrombosis (due to loss of pro-coagulants).
- Henoch Schonlein purpura (HSP): The typical presentation is palpable purpura, renal failure, gastrointestinal and musculoskeletal manifestations. Have normal complement levels.
- Hemolytic uremic syndrome (HUS): Labs consistent with Hemolysis (schistocytes, LDH, reticulocyte count, indirect bilirubin), bloody diarrhea, thrombocytopenia, stool culture for Escherichia coil O157: H7
- ANCA: Have normal complement levels.
- Goodpasture disease: Involves lung and kidneys. Have anti-glomerular basement antibody and normal complement levels.
Prognosis
PSGN has an excellent prognosis especially in children with complete recovery usually occurring within 6 to 8 weeks. In adults, around 50% of the patients continue to have reduced renal function, hypertension, or persistent proteinuria.[12][13]
Death in adults is often secondary to heart failure and renal dysfunction. Studies show that in the long term some patients may continue to have abnormalities in urine, proteinuria, and hypertension.
Mortality during the acute phase of glomerulonephritis has been estimated at around 2 and 12 percent. It has been assumed that the renal changes found in the majority of patients who survived the initial acute attack would be qualitatively similar to those noted in the fatal cases, although little direct evidence existed to support this view.[14]
Complications
During the acute phase, congestive heart failure and azotemia are likely complications that could be life-threatening. The delayed complications include chronic kidney disease and nephrotic syndrome.
Consultations
Deterrence and Patient Education
Avoidance of overcrowding and personal hygiene are important measures that patients should undertake to decrease the risk of catching streptococcal infections.
Patients with throat or skin infections should seek medical advice and get the proper antibiotic therapy if they receive confirmation of a bacterial infection.
Enhancing Healthcare Team Outcomes
Managing a case of PSGN requires cooperation between internists, nephrologists, infectious disease consultants, pharmacists, and nursing staff, functioning as an interprofessional team, to provide excellent care for their patients. PSGN patient’s fluid and salt intake, as well as urine output, should be carefully monitored by the team. The pharmacist should coordinate with the clinician to ensure that the patient is on no nephrotoxic medications and emphasize medication compliance if the patient has hypertension. The visiting nurse should encourage all close contacts and family members to undergo throat swabs to rule out an acute infection. The nurse should also weigh the patient to ensure that the edema is not worsening. Besides, renal function and potassium levels need to be closely monitored.
Consulting a nephrologist (or a pediatric nephrologist) must be sought in complicated cases. These patients need monitoring for fluid and electrolyte status at each visit. Close communication between interprofessional team members is vital to ensure good outcomes. [Level 5]
The prognosis in children is excellent but adults tend to have a protracted course with at least 30 to 50% developing renal dysfunction and hypertension.[15][16][Level 5]