Continuing Education Activity
Morvan Syndrome is an uncommon and complex neurological disorder characterized by hyperactivity of the central, autonomic, and peripheral nervous systems. The disorder manifests in the central nervous system through symptoms such as confusion, behavioral changes, myoclonus, and insomnia, with additional occurrences of hallucinosis and encephalopathy. Autonomic hyperactivity includes features like hyperhidrosis, constipation, labile blood pressure, hemodynamic instability, and cardiac arrhythmias. Painful muscle cramps, myokymia, and neuromyotonia demonstrate peripheral nervous system hyperactivity.
Autoantibodies against proteins comprising the voltage-gated potassium channel complex (VGKC), specifically CASPR2 and LGI1, are often associated with Morvan syndrome. With only 60 case reports published in French and even fewer in the English-language medical literature, Morvan syndrome poses diagnostic and treatment challenges to medical professionals. This educational activity for healthcare professionals aims to enhance their competence in managing Morvan syndrome. Clinicians completing the activity can expect improved diagnostic and treatment skills, ultimately leading to heightened proficiency in addressing the unique challenges associated with this rare and complex neurological condition.
Objectives:
Identify the signs and symptoms of Morvan syndrome.
Interpret antibody testing results and plan treatment accordingly.
Select a treatment modality that best suits the clinical presentation of Morvan syndrome.
Collaborate with the interprofessional team to recognize, diagnose, educate, treat, and monitor patients with Morvan syndrome to improve clinical outcomes.
Introduction
Morvan syndrome (MoS) is a rare and complex disorder of nervous system hyperexcitability. Dr. Augustine Marie Morvan, a French physician, first described MoS in April 1890 in La Gazette Hebdomadaire de Medecine et de Chirurgie. Morvan dubbed the syndrome la chorée fibrillaire (fibrillary chorea), but we now know the disorder eponymously as Morvan syndrome.[1][2]
In the central nervous system, hyperexcitability manifests via confusion, behavioral changes, myoclonus, and severe insomnia; hallucinosis and encephalopathy may also occur. Autonomic hyperactivity includes hyperhidrosis, constipation, labile blood pressure, hemodynamic instability, and cardiac arrhythmias. Finally, peripheral nervous system hyperexcitability is typically demonstrated by painful muscle cramps, myokymia (vermicular or continuous rippling movements, often encountered as eyelid twitching), and neuromyotonia (involuntary continuous muscle fiber activity, often seen as fasciculations, doublet and triplet discharges on electromyography).[3] In short, MoS combines peripheral and central nervous system hyperexcitable states; myokymia, neuromyotonia, muscle fasciculations, stiffness, autonomic nervous dysfunction, severe insomnia, and encephalopathy are commonly encountered, though most patients manifest only some of the symptoms that may occur.
Until the mid-1950s, etiologic theories in MoS focused on infectious causes, especially viral infections; for the second half of the 20th–century, etiologic theories focused on heavy metal toxicity. In 1999, the first report identified a new autoantibody member of the neurexin superfamily, an axonal transmembrane protein called anti-contactin-associated protein-like 2 (CASPR2). To date, approximately 60 case reports of CASPR2-associated MoS have been published in the French literature; the English language peer-reviewed medical literature boasts two case series numbering 43 patients in total.[4][5]
MoS is frequently paraneoplastic and is associated with malignant thymomas, in particular.[6] It is essential to distinguish MoS from acquired neuromyotonia and limbic encephalitis. MoS can be fatal in as many as a third of cases, although a recent small case series from the Indian subcontinent reported death as an outcome in only 1 of 8 patients.[7]
A diagnosis of MoS is confirmed when serum antibody titers for CASPR2 and LGI1 are elevated. Therapeutic plasma exchange, often with immunosuppression, is the preferred treatment modality. Outcomes range from complete recovery to death, with the latter occurring in 20% of patients in a 2012 case series reported by Irani et al.[4]
Consensus in the peer-reviewed medical literature supports the efficacy of immunomodulatory treatment, especially plasmapheresis, in MoS.[8][9][4]
Little is known about the epidemiology of MoS, which is often unrecognized and thus unreported. Orphanet (accessed January 2024) reports the disease prevalence of MoS as less than one case per million. Consensus in the medical literature reveals MoS to be a strikingly male-dominated entity, with male-to-female ratios as high as 19:1 in some studies [4] and ranging from 70% to 90% in others.[5]
Etiology
Though it was first described in the late 19th century, advances in the etiologic understanding of MoS have developed only since the late 1990s. MoS is an autoimmune neurological disorder belonging to the spectrum of conditions associated with antibodies to proteins constituting the voltage-gated potassium channel (VGKC) complex. VGKC antibodies contribute to the pathogenesis of MoS, acquired neuromyotonia (Isaac syndrome), limbic encephalitis, and faciobrachial dystonic seizures.[10][4]
In the first half of the 20th century, MoS was believed to occur as a sequela of viral infection.[11][12] Later, theories of association with heavy metal exposure were posited.[13] Recently, MoS occurring after Siddha traditional medicine treatment in India has been reported.[14]
Since the late 1990s, MoS has been recognized for its strong association with Caspr2 autoantibodies. In some cases, antibodies to the leucine-rich glioma inactivated 1 (LgI1) protein (receptor subunits known as epitempin and DCC) and to the netrin-1 receptor have been identified as additional contributors to pathogenesis in MoS and limbic encephalitis.[15] Netrin-1 has been implicated in angiogenesis, inflammation, tissue remodeling, and cancer: antibodies to the netrin-1 receptor are associated with neuromyotonia in MG patients with previous thymomas.[15] Finally, some patients have antibodies directed against the third identified antigenic component of the VGKC complex, contactin-2.[16]
MoS has long been recognized as a paraneoplastic syndrome, most commonly associated with an underlying thymoma; cases of MoS concomitant with myasthenia gravis associated with underlying thymoma have been reported.[4] Cancers of the lung, sigmoid colon, and testicles and hematologic malignancies, such as lymphoma, can also occur. It should be noted, however, that MoS can occur without underlying cancer; in such cases, the response to immunotherapy may be better than in paraneoplastic cases.[17]
One report has shown CASPR2 protein-coding mRNA in the prostate gland, supporting the possibility that the male reproductive system may harbor these antigens besides brain tissue. This finding was consistent with the onset of MoS in a few patients after scrotal drainage, as reported by Irani et al.[18][19]. Isolated case reports have implicated mRNA vaccinations against COVID-19 as causing a case of LGI1 Limbic encephalitis.[20]
Epidemiology
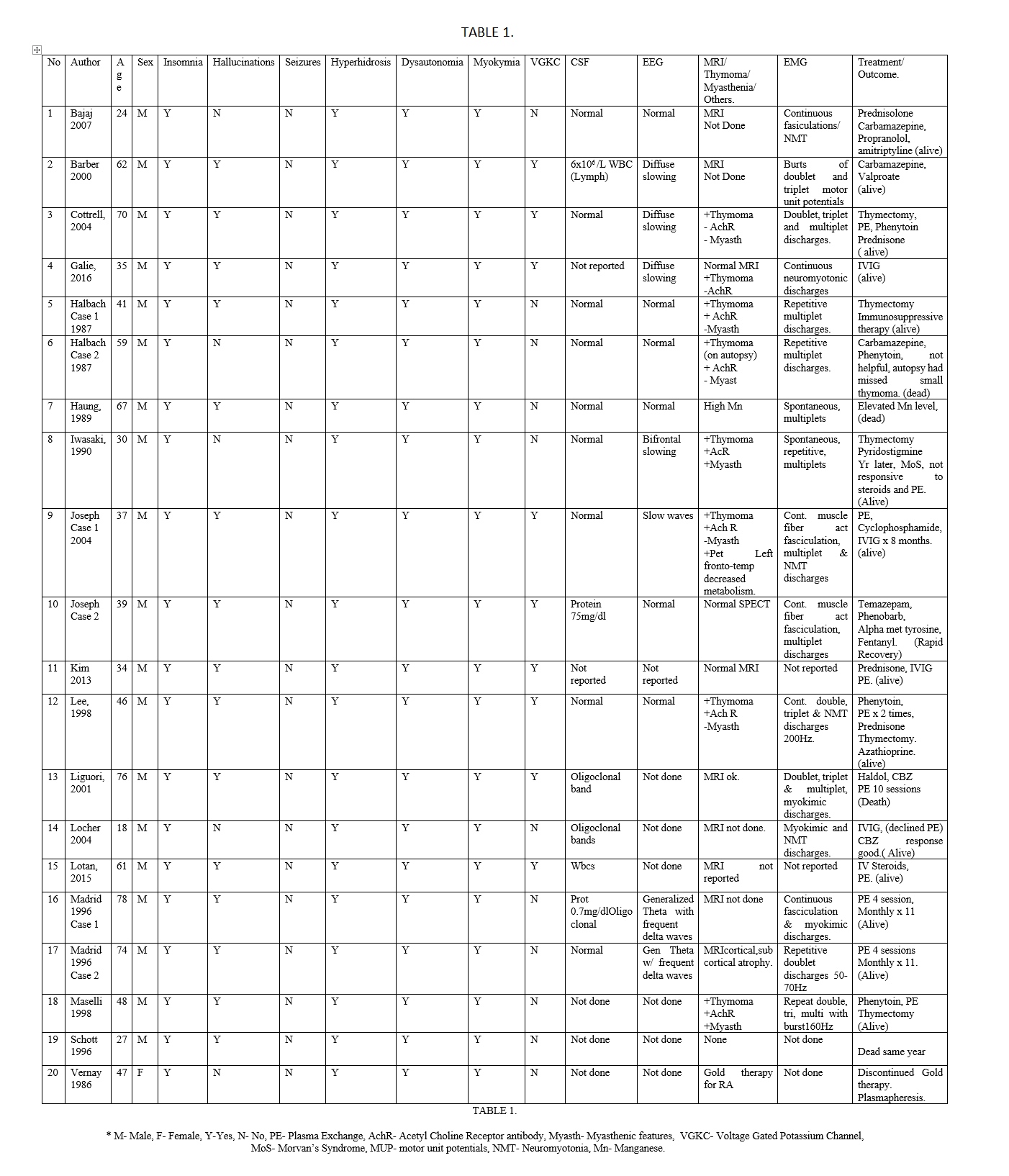
The true epidemiology of MoS is unknown; systematic patient series are few, and, as a result, the condition is likely significantly underrecognized and, therefore, underreported.[21] One case series in 2012 reported information about 29 patients;[22] a 2021 case series reported data from an additional 14 cases.[5]
According to Orphanet (accessed January 2024), MoS is a rare—less than 1 case per million—and life-threatening acquired neurologic disease characterized by neuromyotonia, dysautonomia, and encephalopathy, with severe insomnia.
MoS has an overwhelming male predominance. Murine models in utero exposure to endogenous maternal polyclonal CASPR2 antibodies demonstrated abnormal cortical development in male offspring only.[23] Quite recently, a case report about a woman with multiple positive antibodies, including LGI1, was reported.[24]
As mentioned, MoS is often a paraneoplastic disorder. Paraneoplastic disorders frequently go underdiagnosed and underreported, even though paraneoplastic disease develops in 1 out of 300 patients with cancer; paraneoplastic incidence is estimated to lie between 1.6 and 8.9 cases per million person-years.[6]
In MoS, 75% of cases reportedly demonstrate positivity to Caspr2 antibodies, 60% to LGI1 antibodies, and lower percentages reveal antibodies to netrin-1 or acetylcholine receptors; thymoma is present in 50% to 90% of cases.[21]
Pathophysiology
As previously noted, antibodies against 2 VGKC complex proteins, CASPR2 and LGI1, are now strongly implicated in the pathogenesis of MoS.[25][4] CASPR2 is expressed predominantly in the peripheral nervous system, whereas LGI1 is found in the central and peripheral nervous systems. There is experimental evidence that these antibodies cause neuronal hyperexcitability by suppressing voltage-gated potassium outward currents needed for the repolarization of the motor nerve. Immunostaining of brain tissue shows that these antibodies target subtly different neural substrates likely to underlie the distinctive clinical features seen in Morvan syndrome.
MoS encompasses a wide variety of clinical presentations. LGI1 antibody-mediated autoimmune disorders present mainly with limbic encephalitis, hyponatremia, REM sleep behavioral disorders, and classic faciobrachial dystonic seizures. CASPR2 antibody syndromes are characterized primarily by peripheral nervous system hyperexcitability. MoS can present with any combination of these symptomatologies, depending on the presence of antibodies against CASPR2, LGI1, or both.[19][26][27]
First described in 1999, CASPR2 is a neurexin superfamily transmembrane cell adhesion protein that regulates the recruitment of Kv1.1 and Kv1.2 VGKC subunits at the juxtaparanodal region of myelinated axons, important for proper electrical function.[28][29][21] An animal model recently demonstrated that CASPR2 antibodies can also alter CASPR2 function in the hippocampi, leading to reduced numbers of inhibitory neurons in the hippocampus and suggesting that antibody activity in the brain parenchyma may contribute to hyperexcitability of both the peripheral and central nervous systems.[23][30]
LGI1 is a secreted cell surface protein complex expressed predominantly in the cornu ammonis (CA) 1 and 3 regions of the hippocampus and the dentate gyrus.[31] The leucine-rich repeat subunit is essential for LGI1/LGI1 dimerization, and an epitempin domain (EPTP) mediates the LGI1/ADAM22/23 interaction. The LGI1 protein is crucial for synaptic transmission through its orchestration of interactions with presynaptic Kv1.1 channels and the postsynaptic α-amino-3-hydroxy-5-methyl-4-isoxazole-propionate receptor (AMPA-R).[8][9][10] In one recently reported paper, serum from LGI1 patients with autoimmune encephalitis produced reduced AMPA-R density and caused interruptions in the hippocampal LGI1-ADAM22/23 interaction, collectively leading to modified synaptic transmission.[32]
The various combinations of LGI1 and CASPR2 antibody binding likely contribute to the distinctive and complex phenotypes encountered in MoS. Monoaminergic nuclei in the diencephalon and brain stem are known to be involved in arousal and autonomic homeostasis. A disturbance in this homeostasis can cause insomnia, dysautonomia, and, less frequently, hyponatremia. Dysfunction in the neurons anywhere in the thalamus, hypothalamus, locus coeruleus, and raphe nuclei produces insomnia. The dysautonomia noted in MoS is likely generated within the hypothalamus and raphe nuclei. SIADH-related hyponatremia has been found in patients with LGI1 antibodies: the LGI1 antibody binds to hypothalamic neurons that produce the anti-diuretic hormone, and hyponatremia plausibly arises due to receptor-mediated increased secretion.[33][34]Low plasma sodium is also occasionally associated with CASPR2 antibodies, though the mechanism has yet to be elucidated.
Of note, additional antibodies are occasionally found along with CASPR2 and LGI1 antibodies, including antibodies to the DCC and UNC5a receptors of the anti-Netrin-1 protein (especially in the presence of a thymoma) and antibodies against nonneuronal targets, such as antinuclear or antithyroid antibodies. The role of these additional antibodies in paraneoplastic pathogenesis remains unclear.[21]
As mentioned earlier (See Etiology), some MoS patients have anti-contactin-2 antibodies, rarely found in limbic encephalitis. Contactin-2 is expressed in cardiac conduction tissue, and some reports posit that anti-contactin-2 antibodies may prompt cardiovascular instability in MoS. Some patients display reactivity to antigenic targets inconsistent with LGI1, CASPR2, or contactin-2, leading to the suspicion that additional, not-yet-identified antibody reactivities are present in at least some patients with MoS. This is an area that is ripe for further research.[35]
In paraneoplastic syndromes, 2 broad categories of autoantibodies are implicated. The first group comprises antibodies targeting intracellular nuclear or cytoplasmic antigens, such as anti-Hu, anti-Yo, and anti-Ri antibodies. These antibodies are not directly pathogenic in causing the clinical paraneoplastic syndrome. The second group comprises antibodies targeting cell-surface and synaptic antigens, such as anti-GABAa and anti-NMDA antibody syndromes. These antibodies are pathogenic, causing a B-cell-mediated response at the target antigens.[36] VGKC is a cell-surface or synaptic protein complex that includes CASPR2 and LGI1. The antibodies targeting these proteins are understood to be directly pathogenic through B-cell-mediated pathogenic mechanisms. Treatments targeting the autoantibodies and B-cells are expected to be beneficial.
Regarding insomnia, MoS represents functional interruptions in thalamolimbic circuits regulating the sleep-wake cycle and control of the autonomic system. Thalamic degeneration in MoS may be reversible, distinguishing MoS from fatal familial insomnia, a human prion disease characterized by selective severe atrophy of thalamic mediodorsal and anteroventral nuclei with disconnection of the limbic cortical areas and subcortical regions.[37][3]
Thymectomy and thymoma chemotherapy may trigger the onset of MoS, supporting the possibility that thymic tumors shelter antigenic targets, particularly CASPR2, and somehow become exposed and potentially vulnerable to antibody attack following thymectomy or thymoma chemotherapy.
History and Physical
MoS is characterized by central, autonomic, and peripheral nervous system hyperactivity.[38][1][39]. Historically, findings of neuropsychological dysfunction, autonomic dysfunction, and disordered sleep have been underrepresented in clinical characterizations of MoS, underscoring the need to collect the maximum amount of relevant data when assessing a patient for the possibility of MoS.[5]
CNS features of MoS include encephalopathy, severe insomnia, vivid (usually auditory) hallucinations, delirium, spatial and temporal disorientation, confusion, amnesia, agitation, and hostility. Dysautonomia is primarily characterized by instability, and features include excessive sweating, fever, palmoplantar erythema, pruritus, drooling, severe constipation, excessive lacrimation, arrhythmias, hypertension, weight loss, skin and, rarely, hyponatremia due to the syndrome of inappropriate antidiuretic hormone secretion.[1][40] The peripheral nervous system (PNS) features include peripheral nerve hyperexcitability resulting in continuous muscle fiber activity, neuropathic pain, areflexia (loss of deep tendon reflexes), and a stocking-type sensory loss. Continuous muscle fiber activity is manifested as neuromyotonia, which is clinically seen as myokymia.[41][42][43]
Variable occurrence of the clinical features of MoS is well known and usually depends on the type of antibody detected, whether anti-CASPR2, anti-LGI1, antibodies to both CASPR2 and LGI1, or a combination of other antibodies. Despite the preponderance of peripheral nervous system dysfunction associated with reactivity to CASPR2, MoS patients also frequently present with limbic symptoms at onset, more often seizures than cognitive dysfunction, and most have limbic involvement at some point during their clinical course. Cerebellar ataxia is also common in this population.[44] Serum hyponatremia, delusions, and myoclonus are more common in the presence of LGI1 antibodies.
History-taking in possible MoS should focus on defining the constellation of specific symptoms with which a given individual patient presents clinically. Particularly useful lines of questioning would be those focusing on the topics listed below.
Family history: A hereditary origin of neuromuscular hyperexcitability should always be ruled out, even in non-VGKC-related genes, as evidenced by the recently discovered high frequency of mutations in people of Slavic origin. Peripheral nervous system hyperexcitability has also variably been associated with abnormalities in the KCNA1, KCNQ2, CAV3, and HSPG2 genes.[45]
Comorbid conditions: Practitioners should specifically inquire about concomitant autoimmune diseases, such as myasthenia gravis, thyroiditis, systemic lupus erythematosus, or autoimmune cytopenia.[21] A thorough history of neoplasm, especially cancers of the lung, sigmoid colon, and testicles, along with hematologic malignancies, such as lymphoma, should be obtained.
Signs of peripheral or central nervous system hyperexcitability: Salient signs of nervous system hyperexcitability include history of seizures (especially the typical ictus of faciobrachial dystonic seizures, with brief, posturing movements of the hand and ipsilateral hemiface),[46] stereotypical movements (eg, wringing of the hands), neuropathic pain, stocking-glove sensory dysfunction, falls or ataxia, twitching (myoclonus), and muscle cramps.
Signs of dysautonomia: Dysautonomia may appear in a plethora of ways, including recent constipation, hyperhidrosis, sialorrhea, polydipsia, weight loss, diffuse itching, lacrimation, cardiac arrhythmias, and hypertension.
Behavior and comportment: Delusions or hallucinations, confusion, temporal disorientation, memory or other cognitive problems, agitation, irritability, and hostility may reveal encephalopathy.[3]
Sleep history: Insomnia may be severe and is often characterized by dream enactment behavior, periodic limb movements, and REM sleep without atonia. Insomnia in patients with CASPR2 antibodies is often characterized by agrypnia excitata, a rare syndrome of near-total absence of sleep accompanied by hyperactivation of the central and autonomic nervous systems; agrypnia excitata is found only in MoS, delirium tremens, and the prion disease known as fatal familial insomnia.[46]
Evaluation
The detection of VGKC antibodies in serum is diagnostic of MoS. Although these antibodies are directed against CASPR2 and LGI1 (more commonly both), the CASPR2 antibody is particularly associated with malignant thymoma. Current practice recommendations suggest obtaining serum antibody testing only for CASPR2 and LGI1 instead of more global VGKC antibody testing, as low levels of VGKC abnormalities are commonly found in healthy controls.[47] In MoS, CASPR2 antibodies are found in serum rather than cerebrospinal fluid; antibody titers in MoS tend to be lower than in autoimmune limbic encephalitis patients.[21]
Therefore, the multidimensional clinical presentation possible in MoS necessitates the ability to recognize the syndrome with a high index of clinical suspicion. The investigations that would typically be performed in cases of nervous system hyperexcitability—such as cerebrospinal fluid analysis, magnetic resonance imaging of the brain, electroencephalography (EEG), and positron emission scans—may yield little diagnostic help; these investigations have their greatest utility in ruling out other diagnostic possibilities. Some studies are helpful in seeking associated underlying malignancies. Electromyography (EMG) can confirm myokymia. However, EMG in MoS typically shows fasciculations, multiplets, and after-discharges; myokymia and neuromyotonia are rarely seen in electrodiagnostic studies.[21]
The evaluation, in summary, is a two-step approach. The first step is confirmation by detecting the autoantibodies in the serum or the CSF. The second step is to look for underlying cancer by imaging such as CT chest, abdomen, pelvis, or PET scan.
Diagnostic workup should include a search for possibly associated autoimmune diseases, such as myasthenia gravis (ie, elevated levels of acetylcholine receptor antibodies and abnormal decrement after repetitive nerve stimulation on EMG) or autoimmune cytopenia. When antibody testing is positive for elevated titers of CAPSR2 or LGI1, a workup for occult malignancy is imperative; ruling out malignant thymoma in patients with CASPR2 antibodies is particularly important.[21]
To evaluate dysautonomia “at the bedside,” tests of orthostasis, heart rate changes with deep breathing, and the Valsalva maneuver should be performed.[5]
Polysomnography (PSG) is often thwarted by a patient’s inability to fall asleep and, in some cases, even to cooperate with the study due to behavioral abnormalities and encephalopathy.[5] PSG results in patients with MoS have documented reduced or absent sleep spindles and K complexes (typical features of stage 2 NREM sleep), REM sleep without atonia, and absent or severely reduced slow-wave sleep. In many patients, sleep is so dysfunctional as to satisfy criteria for agrypnia excitata.[48]
Spot EEG is often normal or otherwise unrevealing. However, a 2022 case series exploring the frequency of seizures after the putative achievement of seizure freedom in autoimmune encephalitis due to CASPR2 or LGI1 antibodies has questioned the consensus regarding favorable seizure outcomes in this population. The investigators posited that the incidence of persistent seizures may be as high as 20%. Prolonged video-EEG telemetry is recommended in this patient population and could also be helpful in more straightforward presentations of MoS.[49]
FDG-PET may be revealing in cases of LGI1 autoimmune encephalitis. In cases where the encephalitis is associated with CASPR2 antibodies, FDG-PET findings have yet to be studied conclusively. A preliminary study has reported that medial temporal hypermetabolism and diffuse cortical hypometabolism were found on visual inspection in CASPR2 encephalitis, even without standardized findings (e.g., visual and voxel-based methods). However, standardized PET image analysis, compared to databases of normal studies to clarify the areas with pathological metabolism, is not yet available.[3] FDG-PET can be positive even if structural brain imaging and EEG are negative.[50]
Muscle biopsy may be useful to exclude myopathy or mitochondrial disease in patients with prominent peripheral symptoms.[50]
Treatment / Management
Clinicians have tried several treatment modalities with variable clinical responses, including gold therapy, antiepileptic agents, such as carbamazepine, valproate, phenobarbital, and phenytoin, and procedures such as thymectomy, generally without significant success.
Plasma exchange appears to be the most effective treatment available for MoS; immunosuppression with corticosteroids or other immunosuppressant agents is often also necessary.[1] For reasons that remain unclear, the clinical response to plasma exchange and immunosuppression is variable, possibly due to variability in the mixture of serum factors responsible for causing symptoms. Some authors postulate that immunosuppression is more effective when MoS is associated with other autoimmune conditions, such as myasthenia gravis or autoimmune thyroid disorders. Case reports indicate that symptomatology refractory to plasma exchange may nonetheless respond to agents such as azathioprine, rituximab, and lacosamide.[51][52] Removal of CASPR2 and LGI1 antibodies may also improve agrypnia excitata (even when accompanied by oneiric stupor), though the overall prognosis remains poor in such cases.[37]
A recent Japanese case report underscored the clinicopathological relationship between an unresectable malignant thymoma and MoS, noting that chemotherapy directed against the thymoma both shrank the lesion and improved the symptoms of MoS, suggesting a strong clinical correlation between thymoma and MoS disease activity and raising the tantalizing possibility (not yet investigated) that chemotherapy for thymoma might have utility as a treatment for MoS.[53]
Differential Diagnosis
Documented diagnostic misadventures in MoS have included overinterpretation of positive serum antibodies and mistaking functional, psychiatric, or nonspecific cognitive symptoms for encephalopathy.[54][55]
Limbic encephalitis[40] caused by autoantibodies other than CASPR2 or LGI1 has remarkably similar CNS features to MoS despite subtle differences between these 2 conditions. In limbic encephalitis, amnesia, seizures, and structural abnormalities of the temporal lobe on imaging occur more prominently, but each symptom can also occur in MoS. In limbic encephalitis, neuromyotonia and dysautonomia are generally conspicuous by their absence. Co-occurrence of limbic encephalitis and neuromyotonia is insufficient to warrant a diagnosis of MoS.[56] Additional features that can help distinguish MoS from classical limbic encephalitis are neuropathic lower limb pain, weight loss, male sex, and association with malignant thymomas.
Acquired neuromyotonia, eponymously known as Isaac syndrome,[57] overlaps with MoS in terms of peripheral nerve hyperexcitability, but in Isaac syndrome, overt central or autonomic nervous dysfunction is absent. MoS patients often present with marked weight loss and asthenia features normally absent in Isaacs syndrome.[21] It is important to distinguish peripheral nerve hyperexcitability syndromes from stiff person syndrome, myotonic disorders, and rippling muscle disease.[58][59] Myokymia can be a presenting feature of multiple sclerosis[60] and cervical radiculopathy,[61] and it has occurred as an adverse effect of medications such as gabapentin and acetazolamide.[62][63]
Guillain-Barre syndrome (GBS)[39] is an immune system-mediated ascending neuropathy with muscle weakness, loss of deep tendon reflexes, and sensory deprivation resulting from damage to the peripheral nervous system. A viral infection usually triggers GBS; less commonly, it can present after surgery or vaccination. Diagnosis is generally through clinical exclusion and supported by tests such as nerve conduction studies and CSF analysis. In severe cases, prompt treatment with intravenous immunoglobulins or plasmapheresis and supportive care will lead to functional recovery in the majority.
For comprehensiveness, one ought to include fatal familial insomnia in the differential diagnosis for MoS, as the two conditions overlap in terms of the presence of agrypnia excitata.[64][65] However, FFI is a prion disease, and structural brain abnormalities are usually obvious on MRI imaging, unlike MoS.
Pertinent Studies and Ongoing Trials
Recently, a randomized placebo-controlled clinical trial demonstrated the superiority of intravenous immunoglobulin to placebo in autoimmune epilepsy occurring secondary to positive titers of CASPR2 and LGI1.[66]
Some patients display reactivity to antigenic targets inconsistent with LGI1, CASPR2, or contactin-2, leading to the suspicion that additional, not-yet-identified antibody reactivities are present in at least some patients with MoS. This is an area that is ripe for further research.[35]
Prognosis
The natural history of Morvan syndrome is surprisingly variable, ranging from complete recovery to death. Some cases have been reported to remit spontaneously, and many patients require extensive treatment, mainly in the form of immunotherapy in the form of plasma exchange and long-term immunosuppression. Some cases were fatal; 20% of MoS patients in the 2012 case series by Irani et al died.[4] MoS is a life-threatening condition due to severe dysautonomia and its frequent association with malignant thymoma.[21]
Complications
As noted previously, obtaining PSG is often challenging in MoS, as patients may experience little or no sleep and, in some cases, even be unable to cooperate with the study due to behavioral abnormalities and encephalopathy.[5]
Under anesthesia, spontaneous laryngeal spasms secondary to neuromyotonia and hyperexcitability secondary to potassium channel dysfunction have been reported. To minimize the possibility of laryngospasm, local or regional anesthetic agents are preferred over general anesthesia; muscle-relaxing agents should be avoided to the extent possible.[67]
Consultations
Patients suspected to have Morvan syndrome, due to its extensive neurological symptomatology, would benefit from a neurology consultation in all cases, especially with neurologists specialized in neuroimmunology, neuromuscular disorders, and dysautonomia. Depending on other clinical complications such as cardiac arrhythmias, either cardiology or possibly electrophysiology consultation would be pertinent. The high prevalence of occult malignancies in MoS necessitates the early involvement of oncology. Involving physical, occupational, and speech therapists may help decrease caregiver burden.
Deterrence and Patient Education
Patients should be educated about the rarity of Morvan syndrome, the conditions it mimics or with which it can be confused, and its association with occult malignancies. Patients should also be informed that MoS is often responsive to treatment, and full recovery occurs in some patients.
MoS patients may need considerable support from unpaid caregivers. Extensive physical, occupational, and speech rehabilitation can ameliorate caregiver burden.[55]
Patients should be cautioned about the risk of laryngospasm with general anesthesia and should be instructed to review their MoS with the anesthesiologist before any surgical or other procedure.
Pearls and Other Issues
Identification in the serum of either or both of the auto-antibodies, LGI1 and CASPR2, is the hallmark of the diagnosis of MoS, given the wide variety of clinical manifestations affecting the central and peripheral nervous systems. A high index of suspicion is vital.
Recall that titers of CASPR2 usually exceed those of LGI1. CASPR2 positivity is particularly associated with malignant thymoma, which should be investigated in all cases.
The remarkable clinical improvement often noted after plasma exchange strongly supports the idea that autoantibodies cause this condition. Although the combination of CASPR2 and LGI1 antibodies may explain many aspects of the clinical phenotype, antibody positivity alone offers an insufficient characterization of MoS. It is possible, even likely, that additional antibodies directed against other VGKC-complex proteins will be identified, leading to an improved understanding of the complex presentation with multifocal localization typically seen in MoS.
The index patient in MoS presented with symptoms of irregular small muscle contractions, painful muscle cramps, itching, hyperhidrosis, delirium, hallucinations, and severe sleep disturbances.[3]
Enhancing Healthcare Team Outcomes
Clinical consciousness-raising about the presentation and natural history of MoS is needed to prompt heightened awareness of the condition, facilitating early recognition that could lead to potentially curable immunotherapy.[5]
Providing patient-centered care for individuals with MoS requires a collaborative effort among healthcare professionals, including physicians, advanced practice practitioners, nurses, pharmacists, therapists, and others. First and foremost, healthcare team members must possess the necessary clinical skills and expertise when diagnosing, evaluating, and treating MoS. This includes proficiency in interpreting serum antibody titers, recognizing potential complications, and understanding the nuances of managing this multidimensional disease of overlapping nervous system hyperexcitability. Cardiology and oncology may require consultation depending on the array of symptoms displayed by a given patient with MoS. Moreover, a strategic approach involving individualized care plans tailored to each patient's unique circumstances is vital. To date, no clinical practice guidelines inform the management of MoS, and resources for patient education are largely nonexistent.
Ethical considerations come into play when determining treatment options and respecting patient autonomy in decision-making. Responsibilities within the interprofessional team should be clearly defined, with each member contributing their specialized knowledge and skills to optimize patient care. Effective interprofessional communication fosters a collaborative environment where information is shared, questions are encouraged, and concerns are addressed promptly.
Lastly, care coordination is pivotal in ensuring seamless and efficient patient care. Physicians, advanced practitioners, nurses, pharmacists, and other healthcare professionals must work together to streamline the patient's journey, from diagnosis through treatment and follow-up. This coordination minimizes errors, reduces delays, and enhances patient safety, ultimately leading to improved outcomes and patient-centered care that prioritizes the well-being and satisfaction of those affected by MoS.