Continuing Education Activity
Lower eyelid laxity is part of the normal aging process. Sagging and malposition of the lower eyelid can be frequently seen in the elderly. Understanding the relevant surgical anatomy and how it can be affected by the aging process is crucial for assessing lower eyelid laxity. This helps the surgeons to formulate a reasonable patient-specific management plan to ensure good postoperative results. This activity reviews the relevant surgical anatomy of the lower eyelid, the effect of aging on the lower lid and periorbital region, and highlights the role of the interprofessional team in its management.
Objectives:
- Review the anatomy of the lower eyelid and its relevance when assessing lower eyelid laxity.
- Understand the aging process of the periorbital region and its effect on the lower lid laxity.
- Identify different indications of lower lid laxity assessment.
- Describe how to assess lower eyelid laxity in a systemic approach.
Introduction
The anatomical and physiological integrity of the lower eyelid is important for both functional and aesthetic purposes. It helps in the protection of the cornea and maintenance of the lacrimal drainage system. Surgeons must understand the different techniques that can be used to assess lower eyelid position and laxity. This applies to assessment before cosmetic procedures, e.g., lower blepharoplasty or reconstructive procedure such as facial reanimation after facial nerve palsy. Accurate analysis and diagnosis of the site and the degree of lower eyelid laxity are paramount before any lower eyelid surgical procedure.[1][2][3]
Conditions When Lower Eyelid Laxity Assessment Is Essential
- Before upper and lower blepharoplasty
- After a trauma to the lower eyelid and periorbital region
- When assessing skin cancer in the lower eyelid or lid-cheek junction or adnexal tumors
- Dry eye or epiphora
- Lagophthalmos[4]
- Exposure keratopathy[5]
- Thyroid orbitopathy[6]
- Facial palsy[7]
Anatomy and Physiology
Precise knowledge and understanding of the lower eyelid anatomy are prerequisites for safe and successful cosmetic or reconstructive surgery. However, it has fewer dynamic features. The lower eyelid is divided into two lamellae: anterior and posterior. The anterior lamella is composed of skin and orbicularis oculi muscle. At the same time, the posterior lamella is formed of lid retractors, tarsal plate, and conjunctiva. The septum and the post septal fat lie between these two lamellae and are often referred to as the middle lamella.[8]
The lower eyelid is well apposed to the globe with the lower lid margin at the level of the inferior limbus. The palpebral fissure, the distance between the upper and lower eyelid margins, is around 10mm in the vertical plane and 30 mm in the horizontal plane. It usually slants obliquely from the medial to the lateral canthal angle (lateral canthal tilt) as the lateral canthus is located 2 mm superior to the medial canthus. The lower eyelid crease is identified within 5 to 6 mm from the lower lid margin. It roughly delineates the inferior border of the tarsus and the junction between the pretarsal and preseptal orbicularis oculi muscle.
The skin of the lower eyelid measures less than 1mm in thickness, and it gradually becomes thicker as it comes to the lateral orbital margin. It is devoid of any subcutaneous fatty layer and is anchored to the underlying orbicularis oculi by fine connective tissue attachments.
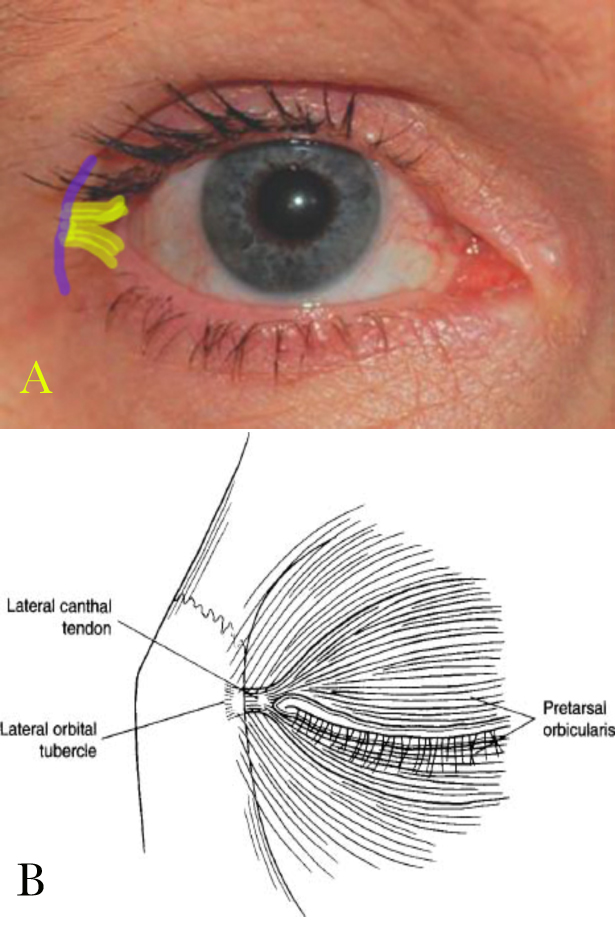
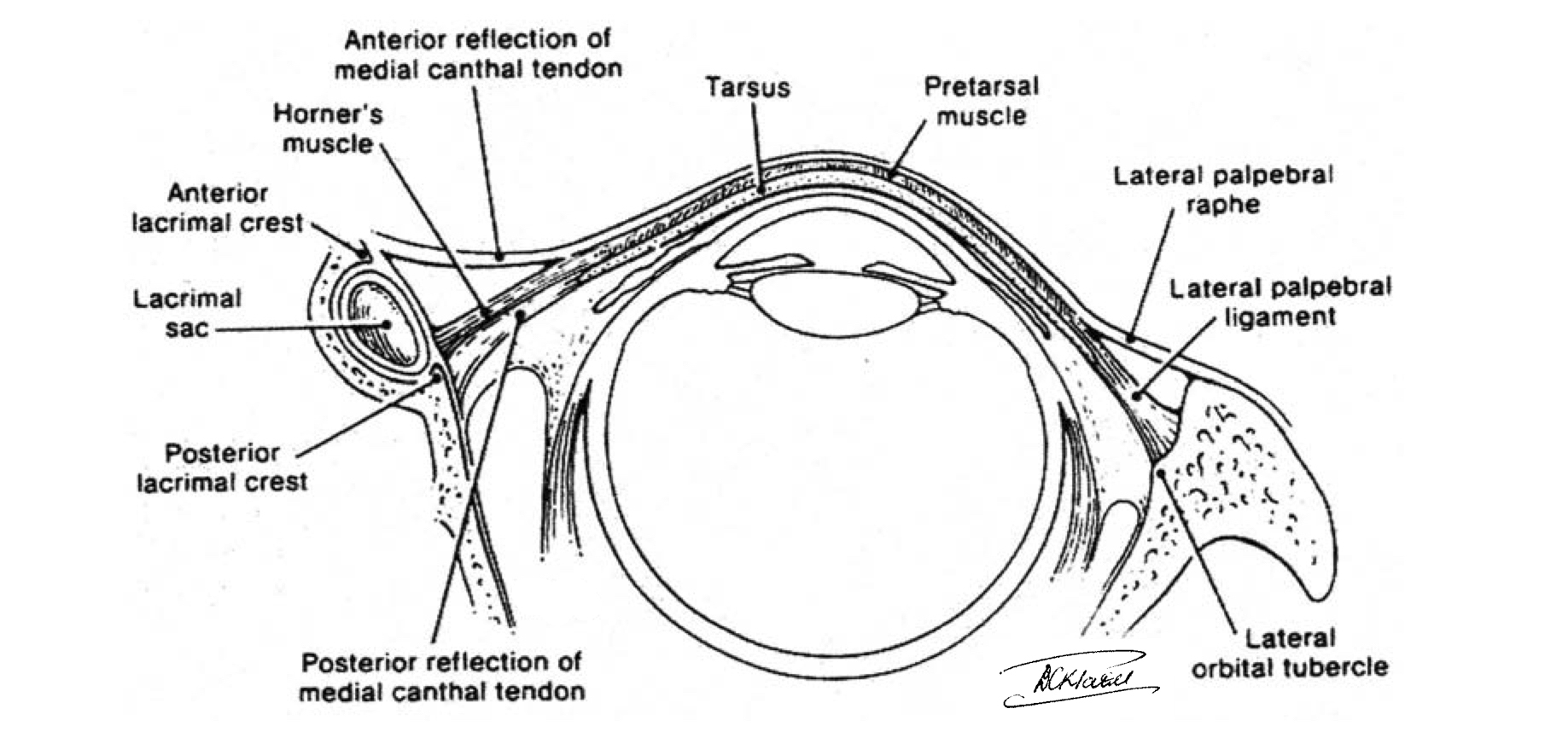
The orbicularis oculi muscle can be divided into a thick orbital part (voluntary) and a thin palpebral part (voluntary and involuntary). The palpebral part can then be subdivided into pretarsal and preseptal portions. The superficial head of the preseptal orbicularis oculi joins together medially to form the medial canthal tendon, which inserts in the anterior lacrimal crest. In contrast, the deeper head inserts in the posterior lacrimal crest. This posterior limb of the medial canthal tendon is mainly responsible for the snug position of the lower eyelid medially. Laterally, the muscle fibers condense and attach firmly to Whitnall’s tubercle, 3 to 4 mm posterior to the lateral orbital rim, as they form the posterior limb of the lateral canthal tendon.[8]
Although the preseptal muscle has a fixed attachment to the medial and lateral canthi, the orbital orbicularis muscle does not. Instead, it directly inserts into the subcutaneous tissue of the lateral orbital region (site of crow’s feet wrinkles). It also gets an attachment from the inferior orbital rim.[9]
The orbital septum lies immediately beneath the submuscular fascia, and it separates between the outer and the inner lamellae. It attaches to the orbital rim except in the inferolateral border, where it forms the recess of Eisler. The orbital septum fuses with the capsulopalpebral fascia posteriorly at 5mm below the inferior border of the tarsus to create a single layer that inserts near the tarsal base. This attachment allows the capsulopalpebral fascia to slightly retract the lower eyelid during downward gaze. The medial part is the thinnest part of the orbital septum. The lateral part shows inferior-lateral thickening, called arcuate expansion, which separates the lateral fat compartment from the central and medial fat compartments.
Orbital fat is contained behind the orbital septum within the orbital cavity, and it is allocated in three compartments (lateral, central, and medial). The lateral fat compartment is smaller, cranially situated, and separated from the central and medial fat compartments by the arcuate expansion. The larger nasal fat compartment is divided by the inferior oblique muscle into central and medial fat pads. Nonetheless, there is an isthmus of fat on top of the inferior oblique muscle that connects these two compartments anteriorly. If a surgeon wants to expose the inferior oblique muscle, he must tease this anterior fat of the muscle.[10]
The sensory nerve supply of the lower eyelid is mainly obtained from the infraorbital nerve with a small contribution from the infratrochlear and zygomaticofacial nerve branches. The main arterial blood supply is derived from angular, infraorbital, and transverse facial arteries. The marginal arcade is situated 2 mm from the lower eyelid ciliary margin, and care should be taken to avoid injuring it during the subciliary approach.
Aging Process
Surgeons must have a thorough understanding of the anatomic changes that occur with aging. Although these changes can vary between different individuals, they mainly occur as a combination of facial soft tissue deflation and descent. This descent is limited by the retaining ligaments in the periorbital area, which are fixed osteocutaneous structures. This creates a concavity that is usually perceived by the patient as a dark circle under the eyelids.[11]
The aging process can affect all layers of the lower eyelid. This can manifest with many clinical features, including dermatochalasis, fat prolapse, laxity of the canthal tendons, and a change in orbicularis oculi muscle tone. Dermatochalasis is excess skin of the lower eyelid that can become aggravated by repeated swelling and inflammation. Loss of the orbital septum integrity causes the orbital fat to protrude. This is also affected by the familial tendency and the history of repeated edema and inflammation. The inevitable loss of strength and laxity of the lower eyelid skeletal support significantly affects the position of the lower eyelid. The tendons usually lengthen, but there is very little lengthening of the tarsal plate (normally 56 mm high and 1 mm thick). This, in turn, can affect the lower eyelid position against the globe and the shape of the palpebral fissure.
The tarsoligamentous laxity can also ameliorate the tone of the orbicularis oculi muscle with subsequent interference with the eye closure mechanism. Moreover, some of these patients can develop ectropion and frequent tearing due to the decrease in the negative pressure usually exerted by the orbicularis oculi on the lacrimal sac with blinking. Some patients, instead, may develop hypertrophy in the orbicularis oculi, which may lead to entropion. The palpebral fissure may also change with aging. As a deep-seated eye patient ages, the lower eyelid moves upward, producing a small horizontal-looking eye fissure. In contrast, patients with prominent eyes are more prone to downward migration of the lateral canthus, which will give the shape of a bigger, rounded eye with a possible scleral show.[11]
Midface aging is another entity that surgeons should examine before any slower eyelid surgery as they interchangeably affect each other. Signs of midface aging may include tear trough deformity, midfacial folds, and malar festoons.[12]
Equipment
A lower eyelid laxity examination is usually performed as a part of the preoperative assessment. Some of the useful tools for completing the evaluations include a Snellen chart for visual acuity assessment, Hertel’s exophthalmometer in the evaluation of the axial eye position, a Schirmer test kit for assessment of dry eye syndrome, and slit-lamp ophthalmoscopy to assess different parts of the eye, especially corneal status.[13]
Personnel
Facial plastic or oculoplastic surgeons should be familiar with lower eyelid laxity examination. This is also applicable to any other surgeons dealing with lower eyelid pathologies such as skin cancers of the lower eyelid. Understanding the vector of pull and how to assess the laxity of the lower eyelid is crucial to prevent postoperative lower eyelid malposition.
Preparation
It is imperative to have a thorough and systematic approach when assessing lower eyelid laxity. This must include an assessment of the general medical condition and examination of the eyelid.
It is important to make sure that the patient is fit for surgery from a medical perspective. Proper history-taking should elicit any significant medical comorbidities that may affect the choice of anesthesia as patients with extensive comorbidities may not be suitable for general anesthesia. A history of frequent use of continuous positive airway pressure (CPAP) machines should be noted as it predisposes to postoperative malar edema. Moreover, any bleeding disorder or medications that influence the bleeding tendency should be documented and optimized before surgery if possible.[14] This, in turn, decreases the potential postoperative risk of retrobulbar hemorrhage and subsequent blindness. Whenever possible, nonsteroid anti-inflammatory drugs should be stopped two weeks before the operation, while warfarin should be held for at least three days until normalization of the prothrombin time. It is also crucial to ensure that hypertensive patients are well-controlled for at least two weeks before the surgery.[15][16]
Dry eye is a common postoperative complication because of the transient impairment of eye closure and blinking mechanisms. The patient should be asked about the history of frequent tearing, ocular discomfort or gritty sensation, and excessive blinking. Further assessment may be needed to elicit the etiology, which may be an allergy, collagen disease, Sjögren syndrome, Graves disease, or incomplete recovery of facial nerve palsy. A Schirmer test is useful to quantify the degree of dryness.[17][18]
Technique or Treatment
Assessment of the lower eyelid laxity should be done systematically, including evaluation of the skin envelope, lower eyelid position, fat compartments, tarsoligamentous laxity, and midface.
Skin
The skin of the lower eyelid and the periorbital area should be assessed for signs of sun damage, rhytids, laxity, edema, festoons, and associated pathologies such as xanthelasma. Skin laxity should be assessed while the patient looks up and while he opens his mouth. On each occasion, the surgeon will perform a pinch test to look for excess skin that can be excised. Moreover, patients with preoperative malar edema should be warned about the risk of postoperative swelling.[19]
Lower Eyelid Position
The lower eyelid position, which is normally at or just above the inferior corneal limbus, should be documented in millimeters. Causes of retraction such as previous eyelid surgery, thyroid orbitopathy, and previous facial burn should be further assessed. Examiner should also look for the presence of Bell's phenomenon (the eye moves up when the patient attempt to close his eyes while the examiner is holding the lids open).[20]
Fat Compartments
The prominence of any of the three fat compartments (lateral, central, and medial) should be noticed and documented with preoperative photography. There should be five views in sitting and standing positions. It should include a close-up view of the eyes when closed, open at rest, when looking upward, and when looking to the sides. Looking upward usually accentuates the medial and central fat pads, whereas looking to the contralateral side may accentuate the medial pocket.[21] Palpation of the inferior orbital rim is an essential part of this assessment. A prominent inferior orbital rim limits the amount of fat that can be excised, and surgeons must be cautious during fat resection as it may lead to a postoperative sunken-eye appearance.
Tarsoligamentous Laxity
The lateral canthus inserts 2mm superior to the medial canthus (canthal tilt). In the case of later canthal tendon laxity, this attachment may stretch or even disinsert, changing the lateral canthus level to the same level as the medial canthus. Moreover, the distance between the lateral canthal tendon and the lateral orbital rim, which is usually between 2 and 3 mm, can increase. This can give a C-shaped rather than a V-shaped lateral canthal angle.[22]
The most common cause of postoperative lower lid malposition is failure to recognize lower lid laxity preoperatively. A lid distraction test (Snapback test) is performed by gently pulling the middle part of the lower eyelid outward, displacing the lid from the globe. In normal lids, it should immediately spring back into the globe. This can be divided into four grades.[21]
- Grade 0: normal lid
- Grade I: takes 2 or 3 seconds
- Grade II: takes 4 or 5 seconds
- Grade III: takes more than 5 seconds but returns to its normal position with blinking
- Grade IV: Never returns back to the normal position.
The lid retraction is another test to assess the lower eyelid tone and the stability of the medial and lateral canthi. This can be done by a gentle downward pull of the lower eyelid towards the inferior orbital rim and observation of the puncta and lateral canthus position. Movement of more than 2 mm of the puncta from the medial canthus indicates laxity of the canthal tendon. Moreover, a slow return of the lid to the resting position opposing the globe is another indication of lower lid laxity.[23]
Medial canthal tendon laxity can also be assessed by gently pulling the lower eyelid laterally while the patient is looking straight ahead and observation of the punctum. Normally, the displacement should be limited to 0 to 1 mm, and it can also be divided into four grades.
- Grade 0: normal lid
- Grade I: 2 mm displacement
- Grade II: 3 mm displacement
- Grade III: more than 3mm displacement
- Grade IV: does not return to the normal position after blinking
Similarly, the lateral canthal corner should only move 2 mm when pulled the lower eyelid is pulled medially. It can also be divided into four grades.
- Grade 0: normal lid (0 to 2 mm displacement of the lateral canthal corner)
- Grade I: 2 to 4 mm
- Grade II: 4 to 6 mm
- Grade III: more than 6 mm
- Grade IV: does not return to the normal position after blinking.
Slit-lamp examination is useful to assess the corneal status and any evidence of dryness. It can be used to check the presence of punctum eversion or stenosis. Furthermore, it can measure the MDR-1 (margin to reflex distance: the distance from the upper lid margin to the corneal reflex, which usually measures 3 to 4 mm) and MRD2 ( the distance between the lower lid margin and the corneal reflex, which is usually between 3 to 5 mm). Assessment of visual acuity using a Snellen chart is another crucial part of the examination.[13]
Midface
The corneal surface is at the same level as the malar prominence. If the cheek is recessed, it is a negative vector or negative malar angle. These patients are at a higher risk of postoperative lower eyelid malposition, and lateral canthal support is always needed when performing lower blepharoplasty. Examiners should also look for signs of aging midface such as tear trough, nasojugal groove, and deepening of the nasolabial fold.[24]
Clinical Significance
Detailed knowledge of the anatomy and aging process of the lower eyelid and the periorbital region is crucial when assessing lower eyelid laxity. A thorough preoperative evaluation should include an assessment of the patient's general condition and a local assessment of the anterior, middle, and posterior lamellae. This systematic approach helps the surgeon to formulate a safe preoperative plan when rejuvenating the lower eyelid.
Enhancing Healthcare Team Outcomes
A thorough understanding of the lower eyelid anatomy and the effect of the aging process on the periorbital regions helps surgeons preoperatively assess the laxity of the lower eyelid and plan the appropriate surgical technique to decrease the chances of lower eyelid malposition. This evaluation may need an interaction between different specialties, especially in complex cases such as facial palsy, dry eye syndrome, or thyroid eye disease. This can be done through interprofessional communication between a facial plastic surgeon, an ophthalmologist, and an endocrinologist if needed. This holistic and integrated approach optimizes the preoperative assessment of these cases. [Level5]