Continuing Education Activity
The sural nerve block is a regional anesthetic technique used as an alternative or adjunct to general anesthesia for foot and ankle surgery. Peripheral nerve blockade of the sural nerve is notably easy to perform since the nerve courses superficially above and at the ankle. One of the first reports and description of the sural nerve block dates back to 1965 when McCutcheon and colleagues reported a 10% failure rate. Ultrasound-guided sural nerve blockade is a more modern option; however, this small nerve is not typically visualized, and perivascular approaches may lead to improved block success. A traditional ankle block is comprised of peripheral nerve blocks to four other major nerves of the ankle, including the superficial peroneal, deep peroneal, saphenous, and tibial nerve, and may or may not include the sural nerve block depending on surgical exposure. However, the provider should include the sural nerve block regardless of operative location within the foot because deep sensory nerve block of the lateral foot and ankle (e.g., vibration coverage) is often desirable for patient comfort. This activity describes the indications of a sural nerve block and highlights the role of the interprofessional team in managing these patients.
Objectives:
- Identify the anatomy of the sural nerve.
- Describe the equipment and personnel required for a sural nerve block.
- Summarize the complications of sural nerve blocks.
- Explain interprofessional team strategies for enhancing care coordination and communication to advance the safe performance of sural nerve blocks and improve patient outcomes.
Introduction
The sural nerve block is a regional anesthetic technique used as an alternative or adjunct to general anesthesia for foot and ankle surgery (Figure 1). Peripheral nerve blockade of the sural nerve is notably easy to perform since the nerve courses superficially above and at the ankle.[1],[2] One of the first reports and description of the sural nerve block dates back to 1965 when McCutcheon and colleagues reported a 10% failure rate.[3] Ultrasound-guided sural nerve blockade is a more modern option; however, this small nerve is not typically visualized, and perivascular approaches may lead to improved block success. A traditional ankle block is comprised of peripheral nerve blocks to four other major nerves of the ankle, including the superficial peroneal, deep peroneal, saphenous, and tibial nerve, and may or may not include the sural nerve block depending on surgical exposure. However, the provider should include the sural nerve block regardless of operative location within the foot because deep sensory nerve block of the lateral foot and ankle (e.g., vibration coverage) is often desirable for patient comfort.[4]
Anatomy and Physiology
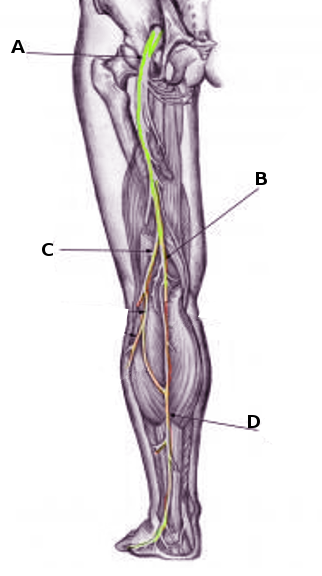
Proximal to the popliteal crease, the sciatic nerve branches into the tibial nerve and common peroneal (fibular) nerve. The tibial nerve courses distally to give rise to the medial sural nerve and posterior tibial nerve which primarily covers the posterior leg and plantar surface of the foot. The medial sural nerve travels between the heads of the gastrocnemius muscle, penetrates the deep fascia to become superficial approximately midway down the calf, and continues posterior to the lateral malleolus and superficial to the extensor retinaculum. [5]
Importantly, the sural nerve is a sensory nerve only with no motor fibers.[6] While ultrasound visualization is emerging within the practice, a sural nerve block can also be performed using anatomic landmarks only.
At the level of the ankle, the two-deep nerves are the tibial nerve and deep peroneal (fibular) nerve, whereas the superficial nerves include the superficial peroneal (fibular), sural, and saphenous nerves. All nerves are terminal branches of the sciatic nerve, except the saphenous which is a sensory branch of the femoral nerve. [7]
Indications
The sural nerve block delivers regional anesthesia during surgeries and postoperative pain control to the posterolateral calf and dorsolateral fifth digit. [1][2]
Contraindications
Contraindications applicable to peripheral nerve blockade also pertain to the sural nerve block (i.e., patient refusal, allergy to local anesthetics, infection at the site of injection or systemic infection, malignancy at the needle entry site, and coagulopathy). A regional nerve block is also not advised if pre-existing neural deficits exist in the distribution of the block. While caution is advised in patients maintained on anticoagulation therapy, the ankle and lateral leg are considered compressible or “superficial block” sites.
Equipment
The necessary equipment includes the following:
- Chlorhexidine gluconate or povidone iodine
- High-frequency ultrasound probe with sterile probe cover and gel
- Local anesthetic, typically 1% lidocaine, for superficial numbing
- Regional block local anesthetic solution (0.5% bupivacaine or 0.5% ropivacaine for postoperative analgesia, and 2% lidocaine or 1.5% mepivacaine when shorter onset time is desired)
- 10t o 20 mL syringe with extension tubing
- Short bevel block needle (2", 22-gauge)
Personnel
An anesthesiologist with training in regional anesthesia is preferable. Additional interprofessional team members, including nurses with sedation training, may be available to assist.
Preparation
The provider performs an informed consent process. A pre-procedural pause is completed, and the patient is positioned so that the lateral aspect of the leg is exposed and easily accessible. Sedation may be provided with midazolam and fentanyl. Aseptic technique is used with application of chlorhexidine gluconate 2% or povidone-iodine solution to the skin of the injection site. A sterile gel is placed on the ultrasound probe and then covered with a sterile probe cover.
Technique or Treatment
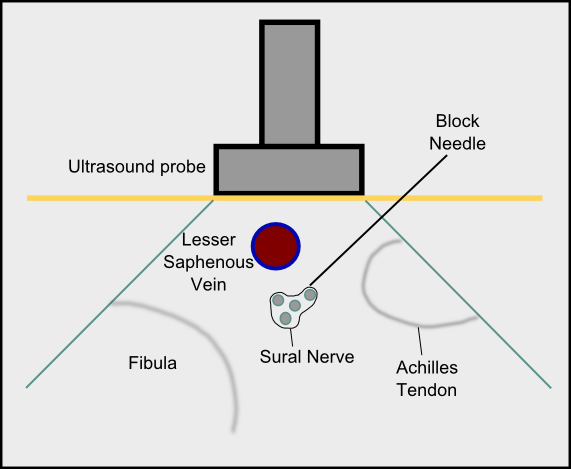
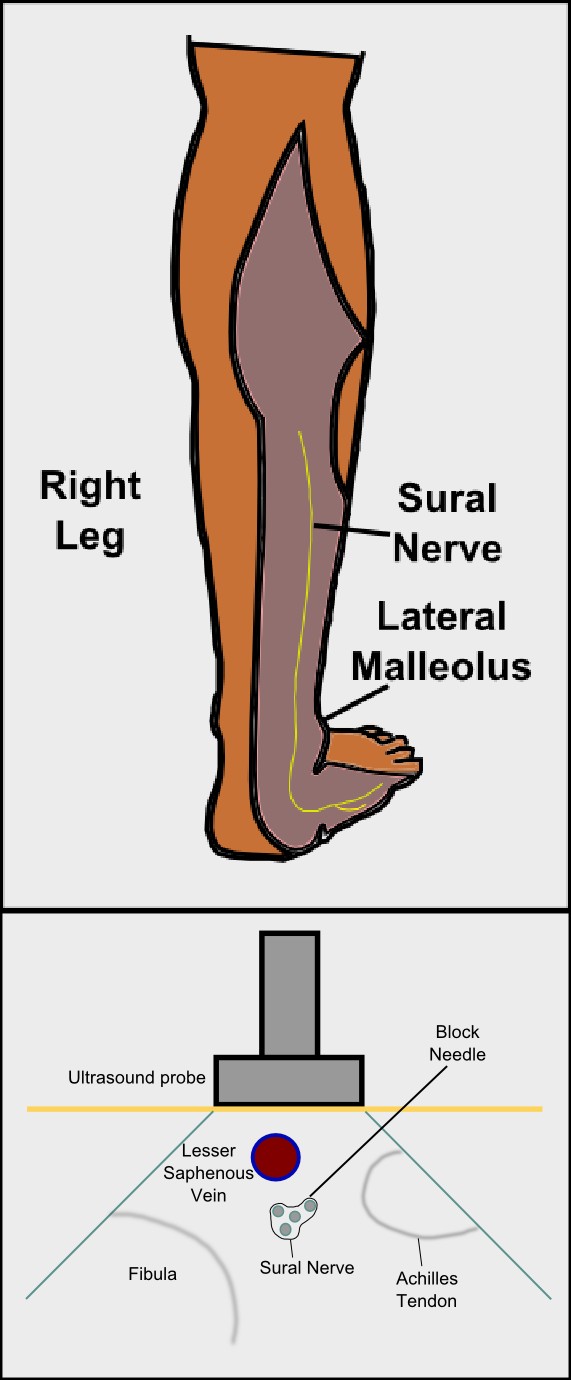
The sural nerve block is typically performed at the level of the ankle. In the ultrasound-guided approach, the provider first locates the key anatomical areas including the posterior border of the lateral malleolus and the Achilles tendon. The site lateral to the Achilles tendon and posteromedial to the lateral malleolus is marked. The linear high frequency (10-18 MHz) ultrasound probe is placed in this marked area in a transverse orientation, and the small saphenous vein is subsequently identified (Figure 2). An out-of-plane approach can be performed, ensuring the local anesthetic (typically 5 mL) is injected circumferentially around the lesser saphenous vein.[8] Alternatively, an in-plane approach may be utilized with the block needle advancing from posterior to anterior toward the sural nerve. A calf tourniquet or dependent position of the leg may increase vein size, aiding in sural nerve identification.
While ultrasound-guidance may lower total local anesthetic volume and minimize the risk of neural or intravascular injection, a standard landmark-based technique is still commonly performed. In this traditional approach, the Achilles tendon and the lateral malleolus are visually identified by palpation. At the level of the superior border of the lateral malleolus and lateral to the Achilles tendon, the needle is inserted with a trajectory aimed toward the lateral malleolus. If a paresthesia is generated, needle advancement is stopped, and a local anesthetic (about 3-5 mL) is injected after a negative aspiration. If no paresthesia is detected, the needle is advanced until it contacts the lateral malleolus bone, and a local anesthetic is subsequently injected as the needle is withdrawn.[3][9][10] In addition to anesthesia in the posterolateral calf and dorsolateral fifth digit, loss of sympathetic tone with color and rubor of the foot may also be indications of a successful block.
Complications
Complications are extremely rare but may include pain on injection, bleeding, infection, and allergic reaction. The intravascular injection can result in local anesthetic toxicity. Nerve damage and significant pain may occur if the needle tip is subfascicular, perineural, or intraneural. [11]
Clinical Significance
While the sural nerve innervates the posterolateral calf and dorsolateral foot, it is least represented in the scientific literature of the five major nerves in the ankle. An electronic PubMed search utilizing keywords “sural nerve” and “regional anesthesia” only yielded six references. Perhaps, this observation may be due to the omission of the sural nerve block in certain foot surgeries as it only provides a small contribution to the forefoot. A study by Coe and colleagues performed 30 ankle blocks that excluded the sural nerve and reported that patients undergoing surgery medial to the third toe reported excellent anesthesia in all cases. [12]
While both ultrasound-guided and traditional landmark-based approaches are utilized, one prospective randomized study by Redborg and colleagues investigated the efficacy of sural nerve block comparing both approaches. They reported that ultrasound guidance using the lesser saphenous vein as a reference point resulted in a more complete and longer lasting block compared to a traditional landmark approach. [8]
Finally, some discrepancy exists in the literature regarding the amount of local anesthetic that is adequate to obtain a successful sural nerve block. Among the first studies describing this technique, McCutcheon only used 1 to 2 mL of local anesthetic.[3] However, the majority of sources recommend at least 5 to 7 mL, but caution is advised for volumes greater than 10 mL due to a risk of vascular occlusion and compartment syndrome.[8][13]
Enhancing Healthcare Team Outcomes
The sural nerve block is usually performed by the anesthesiologist or nurse anesthetist; however, the patient must be monitored by an anesthetic nurse during the entire procedure. While the procedure is simple, inadvertent injection into an artery can occur, sometimes with acute catastrophic results. The nurse must constantly monitor the vital signs as well as check for complications and report back to the operative team if any abnormalities arise. Damage to the nerve can also result in paresthesias that may persist for weeks or months. Hence, the nurse and operative team must assist in patient education, especially if untoward events occur. After the procedure, the recovery room nurse must assess the sensation in the leg before discharge and report back if there are any concerns. To achieve the best outcomes, an interprofessional approach is necessary to achieve the best results. [Level 5]
Nursing, Allied Health, and Interprofessional Team Interventions
- Obtain consent
- Explain procedure to the patient
- Prep the leg
- Prepare the instrument tray
Nursing, Allied Health, and Interprofessional Team Monitoring
- Monitor the patient during the procedure
- Ensure that resuscitation equipment is in the room before the procedure