Continuing Education Activity
Intradiscal electrothermal therapy is a procedure of applying heat to the annulus in cases of low back pain due to discogenic conditions that fail to respond to non-operative techniques. This activity describes the intradiscal electrothermal therapy technique, highlighting the role of the interprofessional team in evaluating and improving care for patients who undergo this lumbar minimally invasive procedure.
Objectives:
- Identify the anatomical structures, indications, and contraindications of intradiscal electrothermal therapy.
- Identify the equipment, personnel, preparation, and technique in regards to intradiscal electrothermal therapy.
- Review the appropriate evaluation of the potential complications and clinical significance of intradiscal electrothermal therapy.
- Describe strategies for improving care coordination and communication among members of the interprofessional team for patients undergoing Intradiscal intradiscal electrothermal therapy to foster optimal patient care.
Introduction
Low back pain (LBP) is a very common and disabling disorder. Many causes of low back pain differ depending on the patient population; mechanical conditions are the most common ones, including facet joint disease, discogenic pain, spinal stenosis, disc herniations, and spondylolysis. Discogenic pain accounts for 30 to 40% of patients with LBP, and multiple interventional therapies have been developed to treat this condition.[1]
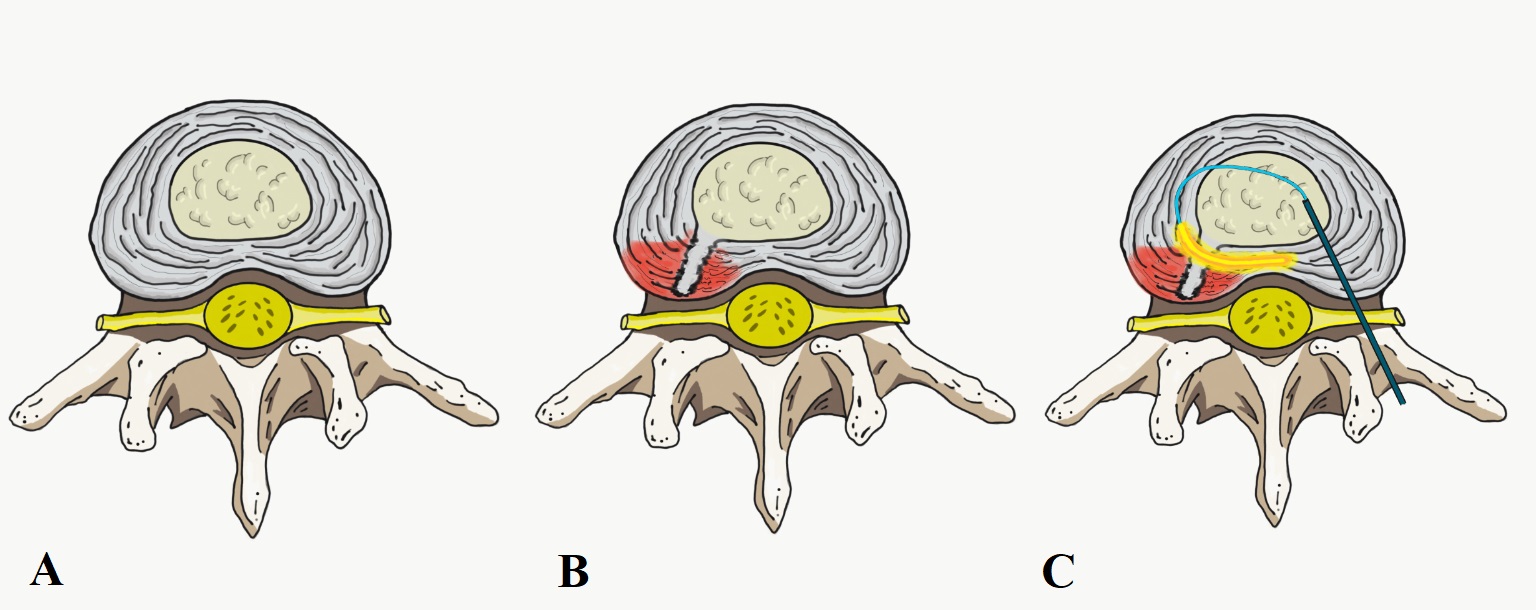
Intradiscal electrothermal therapy (IDET) is a minimally invasive surgical (MIS) procedure for the treatment of discogenic chronic low back pain. The technique involves applying heat to the annulus fibrosus through a catheter with a temperature-controlled thermal resistive heating coil. The goal of thermal disc treatment is to damage the nerve fibers, shrink collagen, and stiffen the disc tissue; this might seal any small tears and limit the expression of matrix components.[2]
Anatomy and Physiology
Intervertebral disc is a fibrocartilage structure that consists of two components: Nucleus pulposus and the annulus fibrosus. The discs absorb the forces across the vertebra and provide cushion during motion.
Mechanical failure of the intervertebral disc is associated with inflammation, dehydration of the nucleus pulposus, decreased disc height, and annular tears.[3]
Discogenic pain is attributable to pain signals arising from nerves in the outer layers of the disc (annulus fibrosus). Outer tears in the annulus fibrosus stimulate nociceptors and inflammatory mediators. LBP pain may also become from nucleus pulposus and vertebral endplates that might irritate the annulus of the intervertebral disc.[4]
Discogenic pain may cause chronic lumbago without sciatica; the pain usually increases with exercise, cough, and Valsalva maneuver. Moreover, physical exam findings differ from a prolapsed or herniated disc where the straight leg raise test is positive.
Indications
IDET is indicated for disc-related chronic low back pain. Ideally, for a select subgroup of patients with non-radicular chronic LBP (usually for at least 3 to 6 months) who fail to respond to conservative treatment including nonsteroidal anti-inflammatory drugs (NSAIDs), stretching, light exercise, traction, bracing and/or bed rest.[5]
Physical examination maneuvers such as straight leg raise test, neurologic assessments (limb strength, sensation, and deep tendon reflex) should be done to rule out the possibility of a nerve root compromise or impairment.
Patient selection and indication summary:
- Failed an intensive non-operative treatment protocol, including non-steroidal anti-inflammatory drugs (NSAIDs), traction, physical therapy and injections
- Patient with persistent low back pain with a normal neurologic exam and without sciatica
- Pain provocation by discography at the affected level and discordant pain at adjacent unaffected levels
- An MRI, which not demonstrate a neural compressive lesion or spinal stenosis
- Annular tears. Lumbar MRI T2-weighted may show a High-Intensity Zone (HIZ) in the posterior or posterolateral intervertebral disc zone (outer annular fibers fissure)
- Disc protrusions of size less than 3 to 4 mm.
- Well to moderate disc hydration (at least 50% remaining disc height)
The gold standard for diagnosing lumbar discogenic pain is a provocative discography. It is a procedure done before IDET in which a contrast gets injected into the nucleus pulposus of the disc, and concordant pain gets reproduced as intradiscal pressures increases. Usually is performed in patients when other diagnostic tests have failed to clear confirmation of a suspected disc as the source of pain. On top of that, provocative discography may characterize the architecture of the disc, providing both anatomical and functional information about a disc [6]. Nonetheless, studies have shown that provocative discography may lead to accelerated disc degeneration, including increased incidence of lumbar disc herniations, loss of disk height, and endplate changes. This procedure may accelerate the progression of degenerative changes in part due to morbidity associated with the injected contrast and also with the needle puncture.[7]
When patients with chronic lumbar back pain fail to respond to conservative treatment and/or minimal procedures such as injection therapy of the epidural space, Radiofrequency, or IDET, surgical treatment should merit consideration.[8][9] Surgical treatment options consist of spinal fusion, nerve decompression, and lumbar disc replacement.
Contraindications
IDET is contraindicated for patients who have severe disc degeneration (greater than 50% disc height loss), extruded or sequestered herniated disc, radiculopathy, spinal stenosis, or spinal instability (such as spondylolisthesis). Also, this procedure is not recommended for patients with previous lumbar spine surgery or IDET before (within the last six months at the same level).[10]
Equipment
Proper equipment is necessary for the IDET procedure:
- Standard radiolucent table with spinal frames and foams pads
- Biplanar fluoroscopy or C-Arm fluoroscopy to localize level and guide to reach intervertebral disc
- Set of access instruments, hollow needle, straight cannulae, temperature-controlled thermal resistive heating coil probe to deliver thermal energy, and an IDET generator
Personnel
No additional staff or personnel is required. Usually, one spinal surgeon, radiologist, a registered nurse staff, operating room nurse (circulator), and anesthesiologist.
Preparation
Medical clearance must be obtained, including pre-operative risk stratification and medical optimization.
The procedure takes place with the patient in a prone position on a supportive frame. The patient receives conscious sedation plus a local anesthetic as an outpatient procedure.
Technique or Treatment
IDET utilizes a 1.5 or a 5 cm flexible active-tip catheter to be placed in the junction between annulus and nucleus pulposus or in the posterior annulus.
Giving an intravenous dose of prophylactic antibiotics is recommended.
Before the IDET procedure, the discs undergo selection on clinical grounds according to the level of a provocative discography. This procedure takes place under biplanar fluoroscopy or C-arm fluoroscopy in which a single needle approach is performed with a stylet needle that ranges in size from 18- to 22- gauge. A posterolateral extradural approach is preferred to avoid damage to the dural sac. Once the lumbar level is confirmed and there is corroboration of the painful disc by provocative discography, the IDET procedure can begin.
IDET procedure is performed unilaterally by a posterolateral extradural approach using anatomic landmarks, the location of the entry point at each level is guided under biplanar fluoroscopy or C-arm fluoroscopy. A hollow needle is advanced containing a flexible catheter with a heating element via a safe triangle located at the anterior border of the ascending facet until reaching the posterolateral zone of the intervertebral disc. At this point, the active tip is advanced anterolaterally into the nucleus pulposus and directed in a circled way to return posteriorly to a final position inside the posterior annulus fibrosus. The introducer needle is then withdrawn, and the final position should be rechecked to obtain a satisfactory result. At this time, the catheter should be fixed and connected to the IDET generator. The standard protocol begins heating the catheter tip at 149 degrees F (65 degrees C) with increments of 33.8 degrees F (1 degree C) every half minute over 12.5 minutes up to a final peak of 194 degrees F (90 degrees C). (Figure 1). This temperature is then maintained for approximately 4 minutes. The total treatment time is 13.5 to 16.5 minutes, and the final temperature and duration are subject to the patient’s pain response.[11]
Antibiotics, either intravenous or injected into the disc, are used to prevent spondylodiscitis. No intradiscal corticosteroids or other medications should be injected into the disc.
The treatment procedure is repeatable in case there are multiple discogenic pain levels (no more than three levels).
Complications
Discography and IDET procedures are associated with very low complication rates.
Related-technique complications include[7][12]:
- Radiculopathy.
- Accelerated disc degeneration
- Endplates deformation
- Spondylodiscitis
- Transthecal puncture route may result in post-procedural headache
- Vertebral osteonecrosis
- -Cauda equina syndrome
Clinical Significance
The IDET mechanism of pain relief continues in controversial and debate regarding its effectiveness. The IDET mechanism of action presumably changes in disc biomechanics, decreased intradiscal pressure, annular denervation, and sealing annular tears.
There is no consistent evidence regarding the effectiveness of IDET, actually positive outcomes to placebo and sham procedures are well recognized, and there may exist an association between the magnitude of sham response and the invasiveness of the procedure.[13][14][15] Nonetheless, several clinical trials show that patients experience clinical benefit from this procedure, and also physical function scores demonstrated continued significant improvement between the 1- and 2-year observation points.[16][17]
The future directions should provide appropriate outcome and cost-effectiveness studies, taking into consideration technique and appropriate selection.
Enhancing Healthcare Team Outcomes
Before IDET consideration, patients should have treatment with a comprehensive exercise training regimen and an optimized regimen of medications such as nonsteroidal anti-inflammatory drugs. The performance of the IDET procedure requires collaboration from all members of the interprofessional medical team. Although a relatively safe procedure, all involved members of the interprofessional team need to communicate across interprofessional lines such as nursing staff working together with physicians and anesthesiologists to provide the highest level of care and patient comfort during the procedure. [Level 5]
Pain relief after IDET is not immediate. Furthermore, it may increase during the first couple of days. Physical therapy is a crucial aspect of recovery, and the PT should keep the rest of the team appraised of patient progress. Orthopedic specialized nursing staff can counsel and direct the patient following the procedure, and coordinate with the PT afterward as rehab begins. During the first month after IDET, 5the patient can plan to walk and do easy stretches. During the first 2 to 3 months, the patient should exercise as directed, and avoid lifting, bending, and long periods of sitting. It is recommendable for patients who have had IDET to wait at least 5 to 6 months to return to vigorous sports such as skiing, running, or tennis.[18]
The best possible outcome for patients undergoing IDET could be encouraged through clear and efficient communication and collaboration among the members of the interprofessional team, as outlined above. [Level V]
Nursing, Allied Health, and Interprofessional Team Interventions
The patient should receive appropriate information about what to expect before, during, and after an IDET procedure.
Before the start of the procedure, the patient should be interviewed about the type, location, and nature of the pain, and any history of prior surgery.
Preoperative instructions such as procedure time, shower or skin preparation, which routine medications to take and hold, prophylactic antibiotics, or anticoagulants, anesthesia premedication.
Remove jewelry preoperatively or tape over as appropriate. For the IDET procedure, it has to be taken into consideration that metals conduct electrical current and provide an electrocautery hazard. Secure patient on the OR table with a safety belt as appropriate, explaining the necessity for restraint.
Nursing, Allied Health, and Interprofessional Team Monitoring
The role of the nurse in the pre and postoperative period should include finite management of intravenous fluids, administering intravenous antibiotics, pain control, wound/dressing care and encouraging patient ambulation, initiate necessary lifestyle changes and participate in an early treatment regimen.
Perioperative nursing monitoring is essential in this outpatient procedure, such as accurate follow-through of instructions/development of preventable complications.
After the procedure is completed, monitoring of vital signs is also performed by the nurse.