Continuing Education Activity
Developmental dysplasia of the hip encompasses several hip abnormalities, including instability, acetabular dysplasia, subluxation, and dislocation. It typically occurs in children with no other comorbid or underlying conditions. While some cases may resolve spontaneously, others necessitate early intervention to prevent complications in adulthood. Accurate identification of the specific hip disorder is crucial for determining the appropriate management and expected prognosis.
Diagnosing developmental dysplasia of the hip involves clinical screening and imaging studies. Clinical examination, including the Ortolani test, the Barlow maneuver, and observation of specific physical signs, aids in early detection. Further x-ray or ultrasound imaging evaluation is warranted based on the clinical findings and the patient's age. Early diagnosis and management are paramount to prevent long-term complications such as persistent dislocation and early hip osteoarthritis. Management options range from conservative measures to surgical interventions, with individualized approaches tailored to the severity of the condition and the patient's age. This activity aims to enhance healthcare professionals' competency in diagnostic testing selection and developmental dysplasia of hip management and foster effective interprofessional collaboration to optimize patient outcomes.
Objectives:
Determine the risk factors for developmental dysplasia of the hip.
Screen patients for developmental dysplasia of the hip clinically.
Identify the management options available for developmental dysplasia of the hip.
Communication with interprofessional team members to improve outcomes and treatment efficacy for patients with developmental dysplasia of the hip.
Introduction
Developmental dysplasia of the hip occurs due to an abnormal hip development, presenting in infancy or early childhood with a spectrum ranging from dysplasia to dislocation of the hip joint. Developmental dysplasia of the hip encompasses several hip abnormalities, including instability, acetabular dysplasia, subluxation, and dislocation. These issues often occur in children with no other comorbid or underlying conditions. Previously referred to as "congenital dislocation of the hip," the term developmental is preferred since not all are present or are identified at birth.
Presentation varies from minor hip instability to frank dislocation. The exact etiology is still elusive. Multifactorial in nature, a combination of genetic, environmental, and mechanical factors play a role. Many genetic loci have also been identified in familial cases.
Though some types of developmental dysplasia of the hip resolve spontaneously, other cases require early intervention to avoid complications in adulthood. However, clinicians must be able to identify the type of hip disorder present as this determines the management indicated and the expected prognosis.[1][2]
Diagnosing developmental dysplasia of the hip consists of clinical screening and imaging studies. Clinical screening is generally done in newborns and children with risk factors for hip abnormalities. Clinical examination includes the Ortolani test, the Barlow maneuver, and noting limited hip abduction, asymmetric gluteus folds, or limb-length inequality, which suggest developmental hip dysplasia.
Abnormal findings on clinical screening should be further evaluated with x-ray or ultrasound imaging, depending on the patient's age.[1][2] Early diagnosis and management will prevent long-term complications like persistent dislocation and early hip osteoarthritis.[3]
Based on the severity of the hip abnormality and the patient's age, management of developmental hip dysplasia consists of conservative treatments (eg, activity modification, physical therapy, and splinting) or surgical interventions.[4][5] No definitive evidence demonstrates that one surgical approach is more effective than the others; therefore, the management is selected according to the surgeon's preferences and the overall clinical picture.[1][2]
Etiology
The following risk factors for developmental dysplasia of the hip have demonstrated an increased incidence of hip abnormalities, which should prompt clinicians to perform clinical screening, including:
- Female sex: There is a fourfold greater incidence in females than males. The increased incidence is likely due to ligamentous laxity from maternal hormones. The odds ratio for females is 4.14 (3 to 5.7).[6]
- Breech position: In the last trimester, breech position is the most significant risk factor for developmental dysplasia of the hip, with an odds ratio of 5.47 (2.58 to 11.6). Procedures that decrease the time spent in the breech position (eg, external cephalic version and prelabor cesarean section) reduce the risk for developmental dysplasia of the hip.[7]
- Family history: Many genes have been implicated in causing developmental dysplasia of the hip in the Asian population, including COL2A1, DKK1, HOXB9, HOXD9, and WISP3. The relative risk is 1.72 (0.05 to 55.00). The risk of recurrence is high, estimated to be 6%. Robert et al also suggested that IL-6 and transforming growth factor-beta 1 (TGF-β1) are the proinflammatory cytokines involved in the pathogenesis of osteoarthritis, which may be associated with developmental dysplasia of the hip in the Caucasian population.[8][9][8]
- Swaddling: Swaddling infants in the adducted and extended position may increase the incidence of developmental dysplasia of the hip in specific populations, including Native American, Japanese, and Turkish infants. International societies, including the American Academy of Pediatrics (AAP) and the Pediatric Orthopaedic Society of North America (POSNA), recommend hip-healthy swaddling. See the Swaddling and Developmental Dysplasia position statement available on POSNA.org.
- In utero restriction: Any physical limitation within the uterus (eg, large for gestational age infants, oligohydramnios, multiple gestations) can contribute to developmental dysplasia of the hip. Space restrictions can also increase the risk of abnormalities like metatarsus adducts, congenital muscular torticollis, and congenital knee dislocation.
- Postterm gestation: Postmaturity is a risk factor for developmental dysplasia of the hip. Prematurity, however, is not associated with an increased risk.[10]
Epidemiology
The incidence of developmental dysplasia of the hip in the UK and US is approximately 10 per 1000 live births, and at birth, 1 in 1000 cases have dislocated hips. In Native Americans, the reported incidence is significantly higher, estimated to be more than 10 times higher. However, in African individuals, developmental dysplasia of the hip is rarely identified. Therefore, the incidence varies with age at diagnosis, race, and modality by which diagnosis was made.[4]
Developmental dysplasia of the hip has a spectrum that ranges from mild hip instability, which resolves spontaneously, to dislocation, which requires surgery. In a prospective study, the sonographic incidence was reported as 69.5 per 1000 live births, but most self-resolved in about 6 to 8 weeks. The remaining incidence of developmental dysplasia of the hip that required some form of treatment was 4.8 per 1000 individuals. No additional cases were seen at the age of 1 year.[11]
Unilateral involvement occurs in 63% of cases, with 64% involving the left side due to the most frequent in utero fetal positioning (ie, left occipitoanterior), in which the left hip of the fetus is adducted against the mother's lumbosacral spine.[12][13] This positioning contributes to increased pressure and potential constraint on the left hip joint during fetal development.
Pathophysiology
Hip joint formation highly depends on the dynamic relationship between the femur and the acetabulum. Any interference with proper contact between these 2 in utero or infancy (eg, improper swaddling) leads to developmental dysplasia of the hip.
Lower limb buds begin to develop around 4 weeks, with chondroblasts aggregating to form the future bones of the hip joint. At 6 weeks of life, cartilage develops into the femur diaphysis, and precartilage develops into the future femoral head, which cannot be differentiated from the acetabulum. Blastemal cells form trochanteric projections. Around the 7th week, the interzone differentiates the sides of the hip joint. Proximally, the acetabulum is formed as a shallow depression at 65°; this later must deepen to 180°, while distally, the femoral head and articular cartilage develop. The middle layer undergoes autolysis to form joint space, synovial membrane, and ligamentum teres. By the 11th week, the hip joint is recognizable.
However, in utero, femoral head growth is faster than acetabulum growth, resulting in under-coverage of the femoral head; therefore, any disturbance in the contact will lead to abnormal development. The acetabulum continues to grow up to age 5 years.
Consequently, misaligned contact between the acetabulum and femur may result in instability, dysplasia (eg, underdevelopment of the acetabulum ), subluxation with some contact between the acetabulum and femur, or dislocation. Furthermore, chronic changes like hypertrophy of the capsule, ligament teres, and the formation of thickened acetabular edge (ie, neolimbus) further impede contact and prevent the relocation of the femoral head.[14]
History and Physical
Clinical features vary from mild hip instability and limited abduction in the infant to asymmetric gait in the toddler, hip pain in adolescence, and osteoarthritis in the adult. The AAP, the American Academy of Orthopaedic Surgeons (AAOS), POSNA, and the Canadian Task Force recommend screening newborns for developmental dysplasia of the hip.
Newborn Screening
Clinical examination is crucial in identifying developmental dysplasia of the hip, especially in babies with risk factors. The Barlow and Ortolani maneuvers can help identify hip instability or dislocation.
- Ortolani maneuver: With the infant in the supine position, the hip is flexed at 90° and in neutral rotation. The infant should be calm with clothes and diapers removed. This maneuver aims to reduce the dislocated hip by holding the hip so that the thumb is on the inner aspect and the index and ring finger are on the greater trochanter. While applying anterior force on the greater trochanter, gently abduct the hip. Clinicians will feel a jerk or clunk if the hip is dislocated. However, "hip clicks" are clinically insignificant without instability.[15]
- Barlow maneuver: Employing the same initial position as the Ortolani maneuver, force may be applied posteriorly to the trochanter, although the AAP recommends against posterior force, and the hip is adducted. A clunk or jerk is felt if the hip can be dislocated. This maneuver should be performed gently, as forceful adduction can cause instability.[16]
The sensitivity of these maneuvers with experienced hands ranges from 87% to 97 %, and the specificity varies from 98% to 99 %.[17] Asymmetry in the hip position and the number of gluteal skin folds may suggest developmental dysplasia of the hip. However, asymmetry is also a normal finding in 27% of infants without developmental hip dysplasia. Galeazzi sign compares knee height while the hips and knees are flexed and feet flat on the table.
Postneonatal Screening
A limited range of movement in the hip joint may indicate developmental dysplasia of the hip. Limited hip range of motion is typically defined as abduction of less than 75° or adduction exceeding 30° past midline. Asymmetrical gait (ie, Trendelenburg gait) due to abductor insufficiency, lumbar lordosis, toe walking, leg length discrepancies, and early hip osteoarthritis may also suggest hip dysplasia.
- Klisic test: The middle finger is placed over the greater trochanter and the index finger over the anterior superior iliac spine.
- An imaginary line between the 2 fingers points at or above the umbilicus on the normal hip.
- On a dislocated hip, the trochanter is elevated, and the line projects inferior to the umbilicus.
Evaluation
POSNA, the Canadian Task Force on DDH, the AAOS, and the AAP recommend periodic surveillance for developmental dysplasia of the hip throughout infancy. The goal of screening is to prevent a delayed diagnosis beyond the age of 6 months. AAP clinical practice guidelines recommended a hip ultrasound (US) at 6 weeks of age or a hip x-ray at 4 months of age in girls with a positive family history of developmental dysplasia of the hip or breech presentation in the third trimester.
Universal screening is controversial, as most of the instability found self-resolves.[18] Computed tomography (CT) or magnetic resonance imaging (MRI) is typically used to evaluate the hip after closed reduction and spica casting. Further evaluation following a positive screening examination depends on the patient's age and available expertise.
- Newborns
- Normal exam with risk factors: Perform US hip at 6 weeks, allowing physiologic immaturity and laxity to resolve.
- Inconclusive exam or hip clicks: Repeat exam in 2 to 4 weeks.
- Positive Ortolani or Barlow maneuvers: Refer to an orthopedic specialist with experience.
- Age 4 weeks to 4 months
- Inconclusive exam: Refer to a specialist or perform hip US at 6 weeks.
- Positive Barlow or Ortolani maneuvers: Refer to an orthopedic specialist with experience.
- Beyond 4 months
- Clinical examination is limited as capsule laxity decreases; the Barlow and Ortolani maneuvers may not be positive. Limited hip abduction becomes the most crucial screening method in older children.
- Femoral head nuclei usually appear between 4 and 6 months, ranging from 1.5 to 8 months, so x-ray is the preferred diagnostic modality over the hip US.
- Normal pelvic radiographs at 4 months can reliably exclude hip dysplasia in children with risk factors.
Ultrasound Imaging
The American Institute of Ultrasound in Medicine and the American College of Radiology recommend hip US to visualize acetabular dysplasia, hip dislocation, femoral head anatomy, ligament teres, and the hip capsule. The most important finding to identify is femoral head coverage by the acetabulum, a minimum of 50%, and depth of the bony acetabulum, known as the alpha angle, where a finding exceeding 60° is considered normal.[19] The following Graf classification lists criteria utilized to diagnose developmental dysplasia of the hip that was established for static imaging:
- Alpha angle: The angle between the bony acetabulum and ilium, normally >60°
- Beta angle: The angle between the labrum and ileum, normally <55°
X-ray Imaging
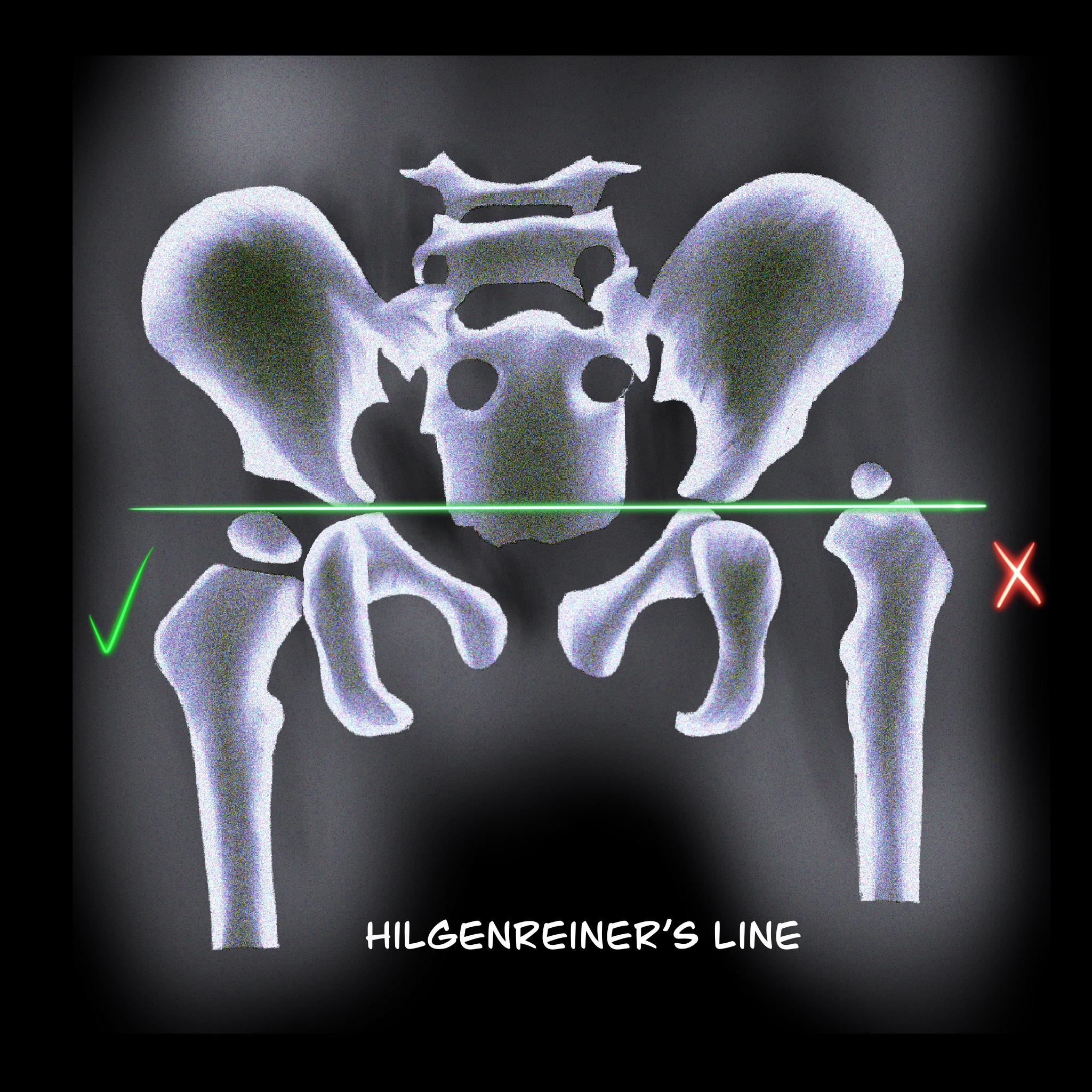
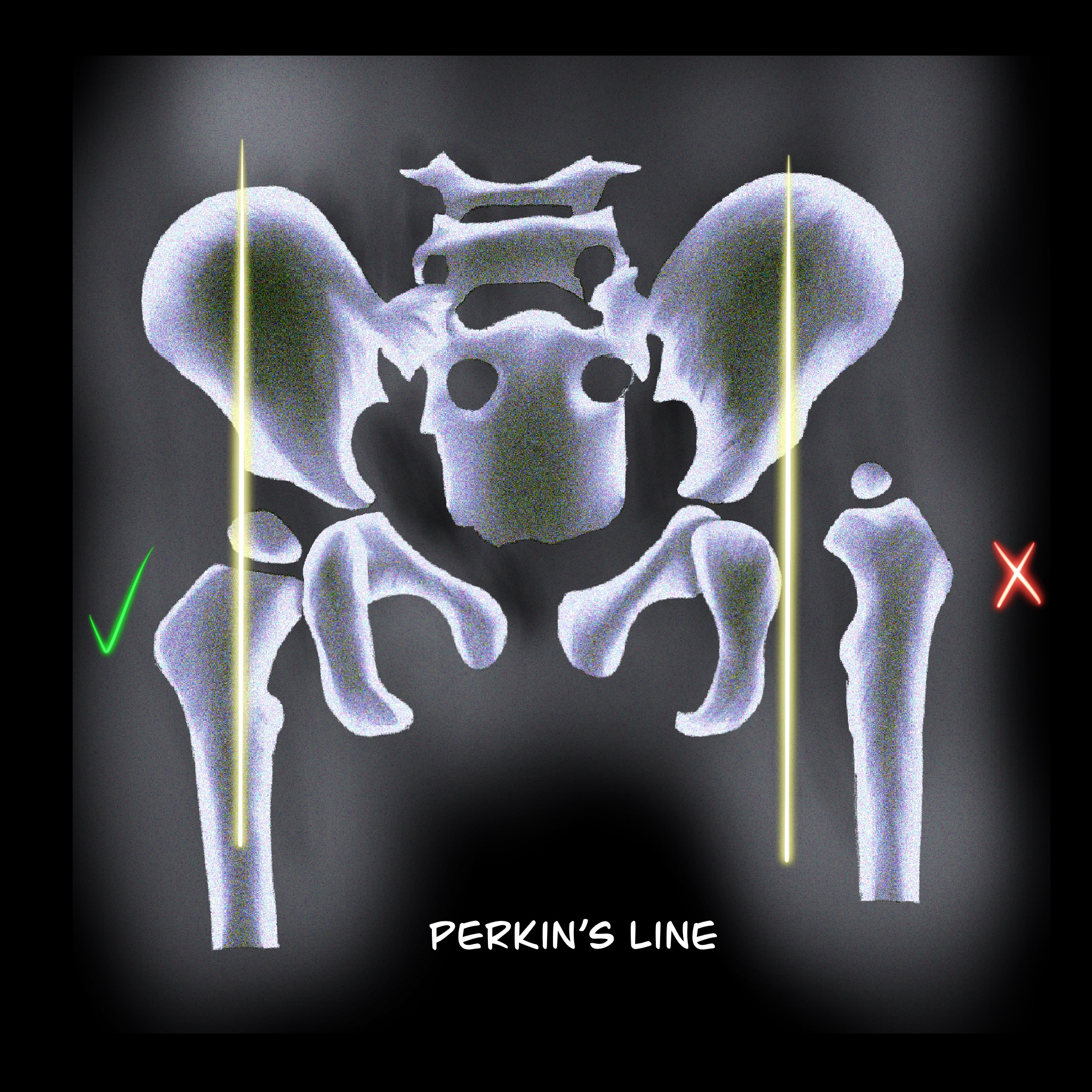
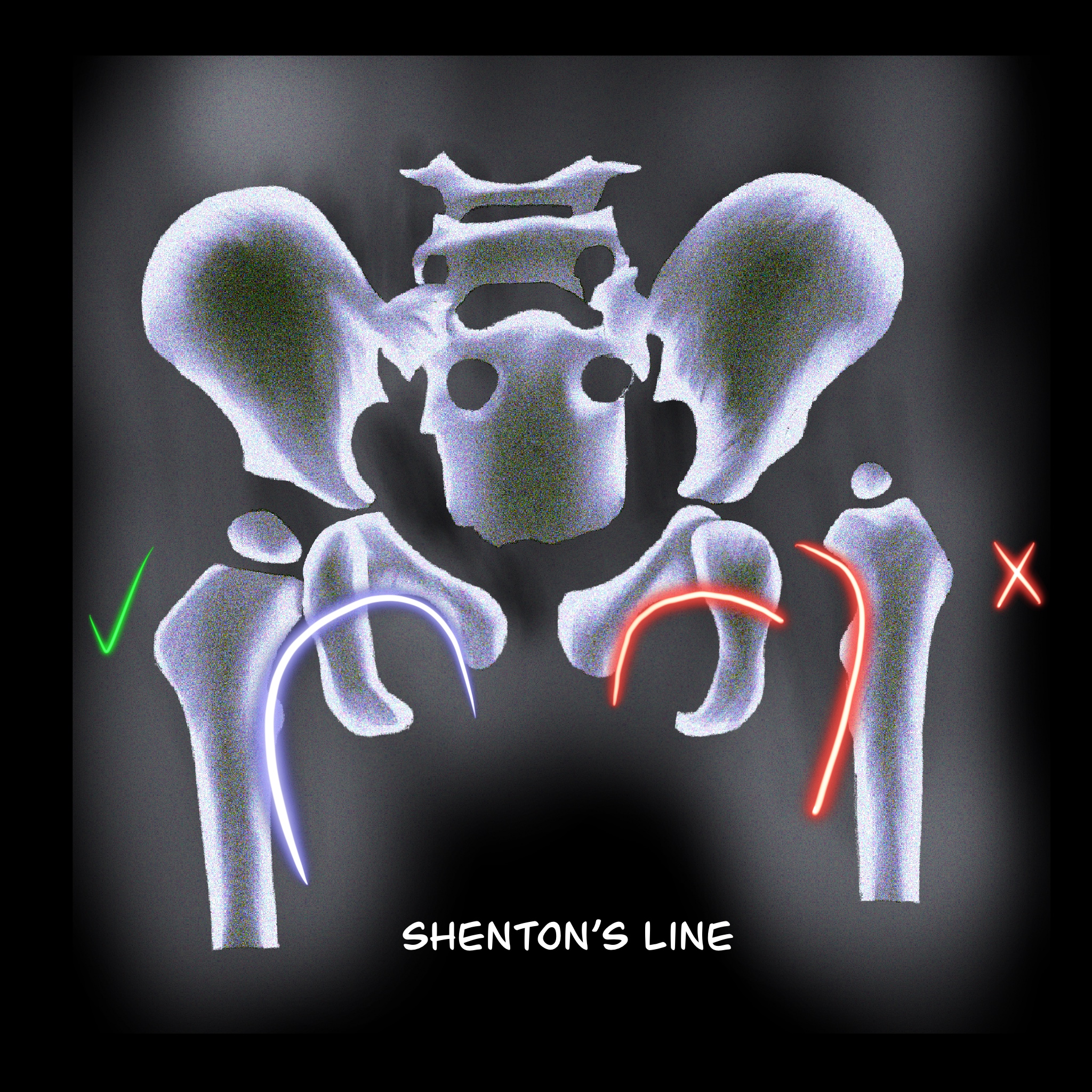
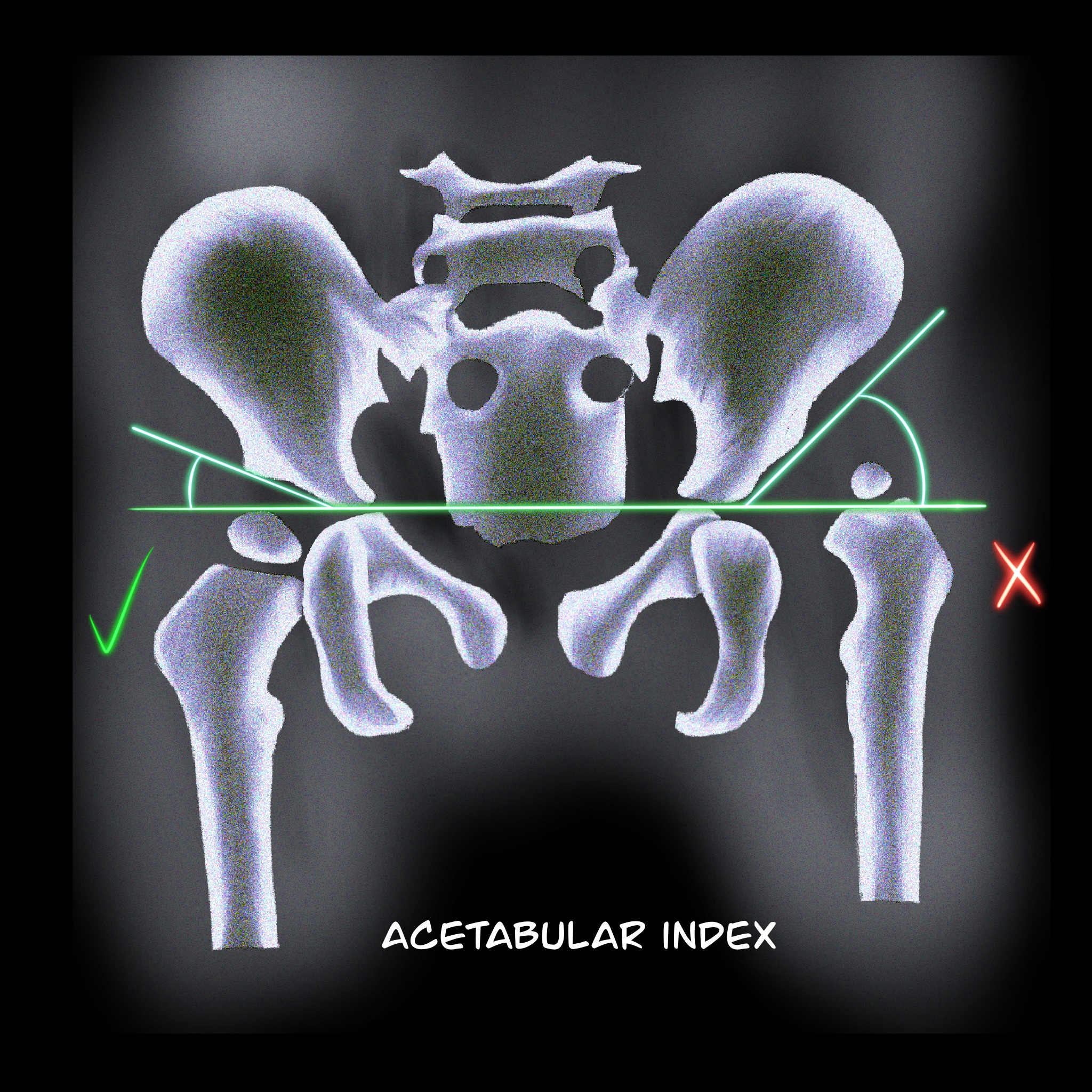
If x-ray studies are used to evaluate developmental dysplasia of the hip, the following findings can help identify hip abnormalities:
- Hilgenreiner line: A horizontal line through the right and left triradiate cartilage; the head of the femur should be inferior to this line (see Image. Hilgenreiner line).
- Perkin line: Perpendicular line to the Hilgenreine line through a focus at the lateral side of the acetabulum. The femoral head should be medial to this line (see Image. Perkin line).
- Shenton line: A Smooth arc that connects the femoral neck to the superior margin of the obturator foramen. Any disruption indicates an abnormality (see Image. Shenton line).
- Acetabular index: The intersection between the Hilgenreiner line and a line drawn tangential to the lateral ossific margin of the roof of the acetabulum. The standard index is <35° at birth and <25° at the age of 1 year. (see Image. Acetabular Index)
- The center-edge angle of Wiberg: Formed by the Perkin line and a line coming from the femoral head's center to the acetabulum's lateral edge. This measurement is reliable in patients older than 5 years old. Values should be >20°.
Treatment / Management
Treatment of developmental dysplasia of the hip aims to provide an optimal environment for the normal growth of the femoral head and acetabulum. Therefore, a high suspicion index and routine surveillance are needed to detect DDH and prevent complications. Treatment modalities like abduction splinting, closed reduction, and open reduction are available to establish optimal contact between the femoral head and the acetabulum. Double diapering is likely harmless but is not an effective treatment. The following management approaches are frequently implemented depending on the patient's age and severity of hip dysplasia:
Patients aged 0 to 4 weeks: Mild instability without a dislocatable hip can be observed.[20] Early referral to an orthopedic surgeon experienced in treating developmental dysplasia of the hip will be optimal if the hips are dislocatable. The application of abduction splints (ie, Pavlik harness) will determined by the attending orthopedic surgeon. However, a study by Larson JE et al concluded that waiting up to 30 days before initiation of treatment showed no significant difference in the outcome.[21]
Patients aged 1 to 6 months: Abduction devices can be tried, including the Pavlik harness, Von Rosen splint, Lausanne-developed abduction brace, Ilfeld orthosis, and Frejka pillow. The Pavlik harness is a widely used device for developmental dysplasia of the hip, consisting of an anterior strap that flexes the hip at 90° and prevents extension, along with a posterior strap to prevent adduction. The device is worn for 23 hours daily for at least 6 weeks or until the hip is stable.
A hip US is done every 3 to 4 weeks to monitor the position of the femoral head, with a success rate of about 90% for a Barlow's positive hip. The failure rate is high in patients who have an Ortolani-positive hip, initiation of treatment after 7 weeks, multigravidas, foot deformities, and males.[22] If the hips are not reduced by 3 weeks, semi-rigid, nonflexible abduction devices like Ilfed orthosis can be tried to keep the hip abducted. A study by Sankar et al reported an 82% success rate with an Ilfed orthosis after failure with a Pavlik harness.[23]
Patients aged 6 to 18 months: For infants diagnosed with developmental dysplasia of the hip at this age or those who have failed abduction devices, closed reduction with a hip spica cast is preferred. Under general anesthesia, the hip is placed in 90° to 100° flexion and 40° to 50° abduction. The failure rate is about 13.6%.[24]
The main complication is avascular necrosis of the head. CT or MRI is needed to confirm the hip position. In a study by Gornitzky AL et al, MRI with contrast can identify perfusion abnormalities following closed reduction, thus preventing avascular necrosis.[25]
Patients aged 18 months to 8 years: Open reduction is preferred for children diagnosed with developmental dysplasia of the hip older than 18 months and infants who have failed closed reduction. Open reduction can correct anatomical abnormalities, including inverted labrum, neolimbus, pulvinar, and hypertrophied ligamentum.
Capsulorrhaphy and release of tight iliopsoas tendons can also be performed. The preferred approaches are the anterior (ie, Smith-Peterson) and the medial techniques. The medial approach is less invasive, but the anterior is classical and corrects most anatomical abnormalities.
A femoral shortening osteotomy can be added to children if needed. The main complication is avascular necrosis. After open reduction, a spica cast is applied, and reduction is confirmed with CT or MRI.
Acetabular Dysplasia
Children with shallow or vertical acetabulum are at risk of developing osteoarthritis due to edge loading. Patients presenting with acetabular dysplasia up to the age of 5, without dislocation, can be treated with part-time or full-time abduction orthosis. After 5 years of age, pelvic osteotomies (eg, Salter, Pemberton, and Dega) use a single cut to increase anterior or anterolateral coverage. If the patient has an open triradiate cartilage center, a triple cut (ie, triple innominate osteotomy) can be performed.
Salvage pelvic osteotomies are indicated for patients older than 8 years old with a subluxated femoral head. The procedure involves placing an extra-articular buttress of bone to the lateral weight-bearing aspect of the acetabulum. The Chiari procedure is indicated for patients with inadequate femoral head coverage and a concentric reduction that cannot be obtained. This procedure involves medializing the acetabulum via iliac osteotomy.
Adolescent and Adult Hip Preservation Surgery
Patients who are presenting with hip pain and shallow acetabulum with radiographic findings of femoral head under coverage and closed triradiate cartilage but without signs of hip degeneration can be treated with a periacetabular osteotomy (PAO). Bernese PAO is a technique in which multiple cuts are made to modify and reorient acetabular cartilage while maintaining an intact posterior column.[26]
Differential Diagnosis
Other conditions causing leg length discrepancies include:
- Proximal femoral focal deficiency
- A femoral neck fracture
- Coxa vara
- Residual effects of infective arthritis
Prognosis
The long-term outcome of treated developmental dysplasia of the hip depends on several risk factors, including the degree of dysplasia, the age of diagnosis and type of treatment, and whether a concentrically reduced hip joint was obtained. Approximately 90% of neonatal hips with instability or mild dysplasia with a Barlow-positive hip, an alpha angle of 50° to 60°, and 50% to 60% of coverage resolve spontaneously with normal functional and radiographic outcomes.[5] A 95% reduction is achieved with the Pavlik harness, and residual dysplasia occurs in 20%. If left untread over a prolonged period, there will be a gradual progression of functional disability, which causes accelerated osteoarthritis.[27]
Complications
Failure to identify and treat developmental dysplasia of the hip can lead to functional disability, hip pain, and accelerated osteoarthritis. Some patients may develop complications following treatment with a pelvic harness. The most severe complication is avascular necrosis of the femoral head, which varies from 0% to 5%.[28] Proper fit can prevent this complication.
If the infant stops demonstrating spontaneous knee extension while in the Pavlik harness, femoral nerve palsy may be suspected. Incidence of about 2.5 %. Most are associated with severe dysplasia or maintaining the hip flexion beyond 120°. Femoral palsy resolves if the harness is removed. Residual hip dysplasia may occur following treatment with a harness. Follow-up biannual or annual x-rays are needed to monitor this condition until skeletal maturity is achieved. A normal x-ray at the age of 2 indicates a good prognosis. Other complications include skin irritation, pelvis erosion, and knee subluxation. Complications that can occur with open or closed reduction include redislocation, osteonecrosis, infection, and stiffness.
Deterrence and Patient Education
A primary postnatal risk factor for developmental dysplasia of the hip is swaddling, so parents need to learn the proper swaddling technique to prevent developmental dysplasia of the hip before leaving the hospital. Parents should also be educated about the importance of regular pediatric check-ups to monitor their child's hip development and detect signs of hip dysplasia early on.
Pearls and Other Issues
Key facts to keep in mind about developmental dysplasia of the hip include the following:
- Developmental dysplasia of the hip encompasses a spectrum of hip abnormalities ranging from mild instability to complete hip joint dislocation.
- Risk factors include beech presentation, female sex, family history, and swaddling techniques.
- Clinical examination techniques such as the Ortolani and Barlow maneuvers detect developmental dysplasia of the hip in infants.
- Imaging modalities such as ultrasound and x-ray are used to confirm the diagnosis of hip dysplasia.
- Treatment options for developmental dysplasia of the hip vary depending on the patient's age and the severity of the condition. They include a Pavlik harness, closed reduction with spica casting, and surgical interventions like pelvic osteotomy.
- Intreated developmental dysplasia of the hip can lead to long-term complications such as hip pain, limping, and early-onset osteoarthritis.
Enhancing Healthcare Team Outcomes
Management of developmental dysplasia of the hip requires early identification from pediatricians, family physicians, physician assistants, and nurse practitioners. Proper utilization of diagnostic technology, such as US versus x-ray, and timely referral to a specialist are crucial. The AAP, the American Association of Orthopedic Surgeons, and the Canadian Task Force provide clear guidelines for identifying and managing developmental dysplasia of the hip.[17][18][28]
The treatment of developmental dysplasia of the hip depends on the patient's age and the severity of the dysplasia. In cases of minor hip instability (Barlow positive, Ortalani negative), spontaneous recovery occurs in 90% of cases within the first 2 weeks of life.[12]
Continued surveillance by the primary care practitioner during infancy improves detection and early referral. Pavlik harness corrects 95% of developmental dysplasia of the hip if applied before 6 months of age. Residual dysplasia may still occur even after appropriate treatment, necessitating annual follow-up until skeletal maturity is reached.[29]
The child may develop a limp, leg length discrepancy, and limited hip abduction without early treatment. Developmental dysplasia of the hip is the most common cause of early osteoarthritis in women younger than 40 years. Therefore, screening and identifying developmental dysplasia of the hip before 6 months of age should be the goal to prevent long-term complications.