[1]
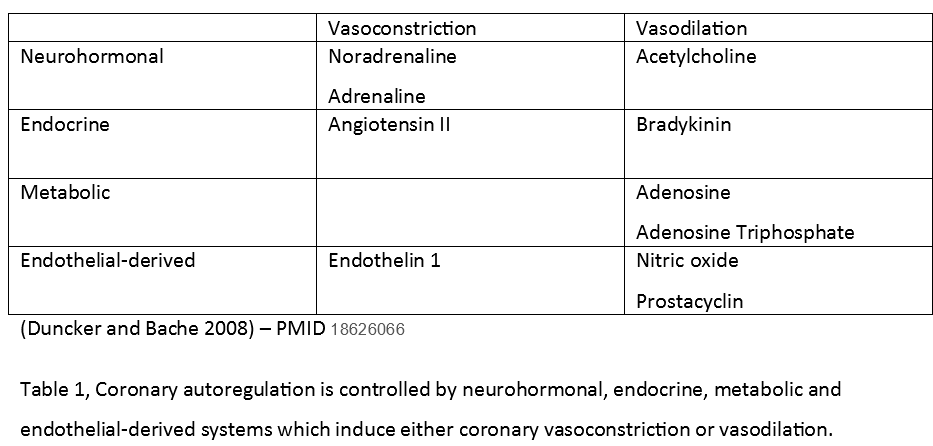
Duncker DJ, Bache RJ. Regulation of coronary blood flow during exercise. Physiological reviews. 2008 Jul:88(3):1009-86. doi: 10.1152/physrev.00045.2006. Epub
[PubMed PMID: 18626066]
[3]
Nguyen T, Do H, Pham T, Vu LT, Zuin M, Rigatelli G. Left ventricular dysfunction causing ischemia in patients with patent coronary arteries. Perfusion. 2018 Mar:33(2):115-122. doi: 10.1177/0267659117727826. Epub 2017 Aug 21
[PubMed PMID: 28823216]
[4]
Loukas M, Sharma A, Blaak C, Sorenson E, Mian A. The clinical anatomy of the coronary arteries. Journal of cardiovascular translational research. 2013 Apr:6(2):197-207. doi: 10.1007/s12265-013-9452-5. Epub 2013 Feb 20
[PubMed PMID: 23423864]
[5]
Brooks H, Kirk ES, Vokonas PS, Urschel CW, Sonnenblick EH. Performance of the right ventricle under stress: relation to right coronary flow. The Journal of clinical investigation. 1971 Oct:50(10):2176-83
[PubMed PMID: 5116207]
[6]
Feigl EO. Coronary autoregulation. Journal of hypertension. Supplement : official journal of the International Society of Hypertension. 1989 Sep:7(4):S55-8; discussion S59
[PubMed PMID: 2681597]
[7]
Goodwill AG, Dick GM, Kiel AM, Tune JD. Regulation of Coronary Blood Flow. Comprehensive Physiology. 2017 Mar 16:7(2):321-382. doi: 10.1002/cphy.c160016. Epub 2017 Mar 16
[PubMed PMID: 28333376]
[8]
Heusch G. Heart rate in the pathophysiology of coronary blood flow and myocardial ischaemia: benefit from selective bradycardic agents. British journal of pharmacology. 2008 Apr:153(8):1589-601. doi: 10.1038/sj.bjp.0707673. Epub 2008 Jan 28
[PubMed PMID: 18223669]
[9]
Banerjee P. Heart failure: a story of damage, fatigue and injury? Open heart. 2017:4(2):e000684. doi: 10.1136/openhrt-2017-000684. Epub 2017 Oct 15
[PubMed PMID: 29081980]
[10]
Choi S, Shin JH, Park WC, Kim SG, Shin J, Lim YH, Lee Y. Two Distinct Responses of Left Ventricular End-Diastolic Pressure to Leg-Raise Exercise in Euvolemic Patients with Exertional Dyspnea. Korean circulation journal. 2016 May:46(3):350-64. doi: 10.4070/kcj.2016.46.3.350. Epub 2016 May 27
[PubMed PMID: 27275172]
[11]
Zhang DY, Anderson AS. The sympathetic nervous system and heart failure. Cardiology clinics. 2014 Feb:32(1):33-45, vii. doi: 10.1016/j.ccl.2013.09.010. Epub
[PubMed PMID: 24286577]
[12]
Cruickshank JM. Clinical importance of coronary perfusion pressure in the hypertensive patient with left ventricular hypertrophy. Cardiology. 1992:81(4-5):283-90
[PubMed PMID: 1301256]
[13]
Gupta S, Vaidya SR, Arora S, Bahekar A, Devarapally SR. Type 2 versus type 1 myocardial infarction: a comparison of clinical characteristics and outcomes with a meta-analysis of observational studies. Cardiovascular diagnosis and therapy. 2017 Aug:7(4):348-358. doi: 10.21037/cdt.2017.03.21. Epub
[PubMed PMID: 28890871]
Level 1 (high-level) evidence
[14]
Chapman AR, Adamson PD, Mills NL. Assessment and classification of patients with myocardial injury and infarction in clinical practice. Heart (British Cardiac Society). 2017 Jan 1:103(1):10-18. doi: 10.1136/heartjnl-2016-309530. Epub 2016 Nov 2
[PubMed PMID: 27806987]
[15]
Yaginuma T, Avolio A, O'Rourke M, Nichols W, Morgan JJ, Roy P, Baron D, Branson J, Feneley M. Effect of glyceryl trinitrate on peripheral arteries alters left ventricular hydraulic load in man. Cardiovascular research. 1986 Feb:20(2):153-60
[PubMed PMID: 3085950]
[16]
Sequeira V,van der Velden J, Historical perspective on heart function: the Frank-Starling Law. Biophysical reviews. 2015 Dec;
[PubMed PMID: 28510104]
Level 3 (low-level) evidence
[17]
Parissis H, Graham V, Lampridis S, Lau M, Hooks G, Mhandu PC. IABP: history-evolution-pathophysiology-indications: what we need to know. Journal of cardiothoracic surgery. 2016 Aug 4:11(1):122. doi: 10.1186/s13019-016-0513-0. Epub 2016 Aug 4
[PubMed PMID: 27487772]
[18]
Johansson S, Rosengren A, Young K, Jennings E. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC cardiovascular disorders. 2017 Feb 7:17(1):53. doi: 10.1186/s12872-017-0482-9. Epub 2017 Feb 7
[PubMed PMID: 28173750]
Level 1 (high-level) evidence
[19]
Marik PE, Varon J. Perioperative hypertension: a review of current and emerging therapeutic agents. Journal of clinical anesthesia. 2009 May:21(3):220-9. doi: 10.1016/j.jclinane.2008.09.003. Epub
[PubMed PMID: 19464619]
[20]
Sutton RM, Friess SH, Maltese MR, Naim MY, Bratinov G, Weiland TR, Garuccio M, Bhalala U, Nadkarni VM, Becker LB, Berg RA. Hemodynamic-directed cardiopulmonary resuscitation during in-hospital cardiac arrest. Resuscitation. 2014 Aug:85(8):983-6. doi: 10.1016/j.resuscitation.2014.04.015. Epub 2014 Apr 28
[PubMed PMID: 24783998]
[21]
Paradis NA, Martin GB, Rivers EP, Goetting MG, Appleton TJ, Feingold M, Nowak RM. Coronary perfusion pressure and the return of spontaneous circulation in human cardiopulmonary resuscitation. JAMA. 1990 Feb 23:263(8):1106-13
[PubMed PMID: 2386557]
[22]
Chapman AR,Shah ASV,Lee KK,Anand A,Francis O,Adamson P,McAllister DA,Strachan FE,Newby DE,Mills NL, Long-Term Outcomes in Patients With Type 2 Myocardial Infarction and Myocardial Injury. Circulation. 2018 Mar 20
[PubMed PMID: 29150426]
[23]
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive care medicine. 2017 Mar:43(3):304-377. doi: 10.1007/s00134-017-4683-6. Epub 2017 Jan 18
[PubMed PMID: 28101605]