[1]
Gonzalez-Araiza G, Haddad L, Patel S, Karageorgiou J. Percutaneous Embolization of a Postsurgical Prostatic Artery Pseudoaneurysm and Arteriovenous Fistula. Journal of vascular and interventional radiology : JVIR. 2019 Feb:30(2):269-271. doi: 10.1016/j.jvir.2018.11.011. Epub
[PubMed PMID: 30717965]
[2]
Faughnan ME, Lui YW, Wirth JA, Pugash RA, Redelmeier DA, Hyland RH, White RI Jr. Diffuse pulmonary arteriovenous malformations: characteristics and prognosis. Chest. 2000 Jan:117(1):31-8
[PubMed PMID: 10631195]
[3]
Antoniou GA, Lazarides MK, Georgiadis GS, Sfyroeras GS, Nikolopoulos ES, Giannoukas AD. Lower-extremity arteriovenous access for haemodialysis: a systematic review. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2009 Sep:38(3):365-72. doi: 10.1016/j.ejvs.2009.06.003. Epub 2009 Jul 10
[PubMed PMID: 19596598]
Level 1 (high-level) evidence
[5]
Demirci O, Celayir A. Prenatal diagnosis and treatment of intrahepatic arteriovenous fistulas: case reports and the literature review. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians. 2022 Mar:35(5):837-845. doi: 10.1080/14767058.2020.1731466. Epub 2020 Apr 2
[PubMed PMID: 32241194]
Level 3 (low-level) evidence
[6]
Jha AK, Sunder A. An unusual case of pulmonary arterio-venous fistula (PAVF). Journal of family medicine and primary care. 2019 Oct:8(10):3408-3411. doi: 10.4103/jfmpc.jfmpc_580_19. Epub 2019 Oct 31
[PubMed PMID: 31742178]
Level 3 (low-level) evidence
[7]
Kandemirli SG, Kizilkaya MH, Erdemli Gursel B, Akca T, Bostan OM. Congenital arteriovenous fistula between descending aorta and the left innominate vein. Surgical and radiologic anatomy : SRA. 2020 Apr:42(4):401-404. doi: 10.1007/s00276-019-02282-z. Epub 2019 Jul 10
[PubMed PMID: 31292677]
[9]
Kléber AG. Consequences of acute ischemia for the electrical and mechanical function of the ventricular myocardium. A brief review. Experientia. 1990 Dec 1:46(11-12):1162-7
[PubMed PMID: 2253715]
[10]
Guneyli S, Cinar C, Bozkaya H, Korkmaz M, Oran I. Endovascular management of congenital arteriovenous fistulae in the neck. Diagnostic and interventional imaging. 2016 Sep:97(9):871-5. doi: 10.1016/j.diii.2015.08.006. Epub 2016 Mar 11
[PubMed PMID: 26972281]
[11]
Ying A, Al-Asady R, Vicaretti M. Endovascular treatment of a large iatrogenic popliteal arteriovenous fistula. Journal of vascular surgery cases and innovative techniques. 2020 Mar:6(1):129-132. doi: 10.1016/j.jvscit.2019.10.010. Epub 2020 Feb 21
[PubMed PMID: 32123780]
Level 3 (low-level) evidence
[12]
Petrov I,Tasheva I,Stankov Z,Polomski P,Georgieva G,Marinov K, Uneventful Follow-Up 2 Years after Endovascular Treatment of a High-Flow Iatrogenic Aortocaval Fistula Causing Pulmonary Hypertension and Right Heart Failure. Methodist DeBakey cardiovascular journal. 2019 Apr-Jun;
[PubMed PMID: 31384380]
[13]
Farshidmehr P, Zafarghandi MR, Sadat A, Sayarifard A. Coil Embolization of an Iatrogenic Arteriovenous Fistula between the Superior Mesenteric Artery and Vein: A Case Report. The journal of Tehran Heart Center. 2019 Jan:14(1):37-39
[PubMed PMID: 31210769]
Level 3 (low-level) evidence
[14]
Şahin M, Yücel C, Kanber EM, İlal Mert FT, Bıçakhan B. Management of traumatic arteriovenous fistulas: A tertiary academic center experience. Ulusal travma ve acil cerrahi dergisi = Turkish journal of trauma & emergency surgery : TJTES. 2018 May:24(3):234-238. doi: 10.5505/tjtes.2017.49060. Epub
[PubMed PMID: 29786818]
[15]
Davison BD, Polak JF. Arterial injuries: a sonographic approach. Radiologic clinics of North America. 2004 Mar:42(2):383-96
[PubMed PMID: 15136023]
[16]
Van den Broecke M, Vereecke E, De Visschere P. Renal Arteriovenous Fistula. Journal of the Belgian Society of Radiology. 2020 Jan 31:104(1):10. doi: 10.5334/jbsr.2032. Epub 2020 Jan 31
[PubMed PMID: 32025626]
[17]
Fox CJ, Gillespie DL, O'Donnell SD, Rasmussen TE, Goff JM, Johnson CA, Galgon RE, Sarac TP, Rich NM. Contemporary management of wartime vascular trauma. Journal of vascular surgery. 2005 Apr:41(4):638-44
[PubMed PMID: 15874928]
[18]
Kim JW, Kim SJ, Kim MR. Traumatic carotid-cavernous sinus fistula accompanying abducens nerve (VI) palsy in blowout fractures: missed diagnosis of 'white-eyed shunt'. International journal of oral and maxillofacial surgery. 2013 Apr:42(4):470-3. doi: 10.1016/j.ijom.2013.01.007. Epub 2013 Feb 14
[PubMed PMID: 23415244]
[19]
Stathis A, Gan J. Traumatic arteriovenous fistula: a 25-year delay in presentation. Journal of surgical case reports. 2020 Mar:2020(3):rjaa042. doi: 10.1093/jscr/rjaa042. Epub 2020 Mar 24
[PubMed PMID: 32226601]
Level 3 (low-level) evidence
[20]
Cuoco JA, Guilliams EL, Klein BJ, Malaty GR, Witcher MR, Entwistle JJ. N-butyl cyanoacrylate embolization of a traumatic pseudoaneurysm and arteriovenous fistula of the middle meningeal artery. Radiology case reports. 2020 Apr:15(4):321-325. doi: 10.1016/j.radcr.2019.12.009. Epub 2020 Jan 20
[PubMed PMID: 31993092]
Level 3 (low-level) evidence
[21]
Dickey KW, Pollak JS, Meier GH 3rd, Denny DF, White RI Jr. Management of large high-flow arteriovenous malformations of the shoulder and upper extremity with transcatheter embolotherapy. Journal of vascular and interventional radiology : JVIR. 1995 Sep-Oct:6(5):765-73
[PubMed PMID: 8541682]
[23]
Baldini M, Catania A, Orsatti A, Manfredi MG, Motta P, Cantalamessa L. Inhibitory effect of somatostatin on abnormal GH response to TRH in primary hypothyroidism. Experimental and clinical endocrinology. 1992:99(2):80-3
[PubMed PMID: 1353454]
[24]
Zamani H, Meragi M, Arabi Moghadam MY, Alizadeh B, Babazadeh K, Mokhtari-Esbuie F. Clinical presentation of coronary arteriovenous fistula according to age and anatomic orientation. Caspian journal of internal medicine. 2015 Spring:6(2):108-12
[PubMed PMID: 26221510]
[25]
Allon M, Ornt DB, Schwab SJ, Rasmussen C, Delmez JA, Greene T, Kusek JW, Martin AA, Minda S. Factors associated with the prevalence of arteriovenous fistulas in hemodialysis patients in the HEMO study. Hemodialysis (HEMO) Study Group. Kidney international. 2000 Nov:58(5):2178-85
[PubMed PMID: 11044239]
[26]
Nagpal K, Ahmed K, Cuschieri R. Diagnosis and management of acute traumatic arteriovenous fistula. The International journal of angiology : official publication of the International College of Angiology, Inc. 2008 Winter:17(4):214-6
[PubMed PMID: 22477453]
[27]
Hashimoto O, Miyazaki T, Hosokawa J, Shimura Y, Okuyama H, Endo M. A case of high-output heart failure caused by a femoral arteriovenous fistula after endovenous laser ablation treatment of the saphenous vein. Phlebology. 2015 May:30(4):290-2. doi: 10.1177/0268355514525149. Epub 2014 Feb 19
[PubMed PMID: 24553135]
Level 3 (low-level) evidence
[28]
Miller-Thomas MM, West OC, Cohen AM. Diagnosing traumatic arterial injury in the extremities with CT angiography: pearls and pitfalls. Radiographics : a review publication of the Radiological Society of North America, Inc. 2005 Oct:25 Suppl 1():S133-42
[PubMed PMID: 16227487]
[29]
Biswas S, Chandran A, Radon M, Puthuran M, Bhojak M, Nahser HC, Das K. Accuracy of four-dimensional CT angiography in detection and characterisation of arteriovenous malformations and dural arteriovenous fistulas. The neuroradiology journal. 2015 Aug:28(4):376-84. doi: 10.1177/1971400915604526. Epub 2015 Oct 1
[PubMed PMID: 26427892]
[30]
In 't Veld M, Fronczek R, Dos Santos MP, van Walderveen MAA, Meijer FJA, Willems PWA. High sensitivity and specificity of 4D-CTA in the detection of cranial arteriovenous shunts. European radiology. 2019 Nov:29(11):5961-5970. doi: 10.1007/s00330-019-06234-4. Epub 2019 May 14
[PubMed PMID: 31089848]
[31]
Ares WJ, Jankowitz BT, Tonetti DA, Gross BA, Grandhi R. A comparison of digital subtraction angiography and computed tomography angiography for the diagnosis of penetrating cerebrovascular injury. Neurosurgical focus. 2019 Nov 1:47(5):E16. doi: 10.3171/2019.8.FOCUS19495. Epub
[PubMed PMID: 31675711]
[32]
Georgiadis GS, Charalampidis DG, Argyriou C, Georgakarakos EI, Lazarides MK. The Necessity for Routine Pre-operative Ultrasound Mapping Before Arteriovenous Fistula Creation: A Meta-analysis. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2015 May:49(5):600-5. doi: 10.1016/j.ejvs.2015.01.012. Epub 2015 Feb 27
[PubMed PMID: 25736517]
Level 1 (high-level) evidence
[33]
Marin ML, Veith FJ, Panetta TF, Cynamon J, Barone H, Schonholz C, Parodi JC. Percutaneous transfemoral insertion of a stented graft to repair a traumatic femoral arteriovenous fistula. Journal of vascular surgery. 1993 Aug:18(2):299-302
[PubMed PMID: 8350439]
[34]
Numan F, Omeroglu A, Kara B, Cantaşdemir M, Adaletli I, Kantarci F. Embolization of peripheral vascular malformations with ethylene vinyl alcohol copolymer (Onyx). Journal of vascular and interventional radiology : JVIR. 2004 Sep:15(9):939-46
[PubMed PMID: 15361561]
[35]
Zaki Ghali G, Zaki Ghali MG, Zaki Ghali E. Transvenous embolization of arteriovenous malformations. Clinical neurology and neurosurgery. 2019 Mar:178():70-76. doi: 10.1016/j.clineuro.2018.08.024. Epub 2018 Sep 11
[PubMed PMID: 30731326]
[36]
Guo H, Wang C, Yang M, Tong X, Wang J, Guan H, Song L, Zou Y. Management of iatrogenic renal arteriovenous fistula and renal arterial pseudoaneurysm by transarterial embolization: A single center analysis and outcomes. Medicine. 2017 Oct:96(40):e8187. doi: 10.1097/MD.0000000000008187. Epub
[PubMed PMID: 28984770]
[37]
Lee BB, Kim DI, Huh S, Kim HH, Choo IW, Byun HS, Do YS. New experiences with absolute ethanol sclerotherapy in the management of a complex form of congenital venous malformation. Journal of vascular surgery. 2001 Apr:33(4):764-72
[PubMed PMID: 11296330]
[38]
Nosher JL, Murillo PG, Liszewski M, Gendel V, Gribbin CE. Vascular anomalies: A pictorial review of nomenclature, diagnosis and treatment. World journal of radiology. 2014 Sep 28:6(9):677-92. doi: 10.4329/wjr.v6.i9.677. Epub
[PubMed PMID: 25276311]
[39]
CREECH O Jr, GANTT J, WREN H. TRAUMATIC ARTERIOVENOUS FISTULA AT UNUSUAL SITES. Annals of surgery. 1965 Jun:161(6):908-20
[PubMed PMID: 14295942]
[40]
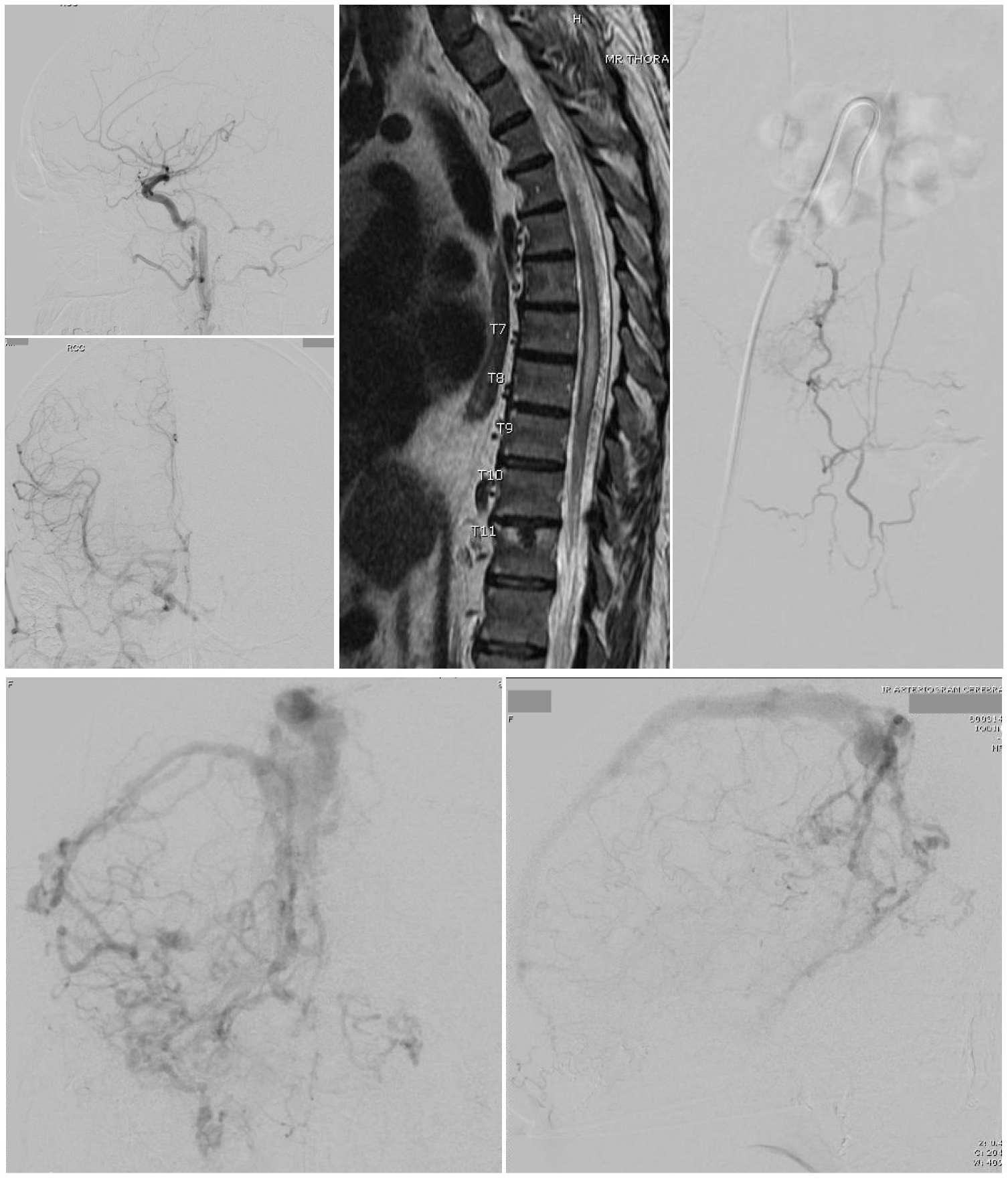
Brinjikji W, Nasr DM, Morris JM, Rabinstein AA, Lanzino G. Clinical Outcomes of Patients with Delayed Diagnosis of Spinal Dural Arteriovenous Fistulas. AJNR. American journal of neuroradiology. 2016 Feb:37(2):380-6. doi: 10.3174/ajnr.A4504. Epub 2015 Sep 3
[PubMed PMID: 26338916]
Level 2 (mid-level) evidence
[41]
Reddy YNV, Melenovsky V, Redfield MM, Nishimura RA, Borlaug BA. High-Output Heart Failure: A 15-Year Experience. Journal of the American College of Cardiology. 2016 Aug 2:68(5):473-482. doi: 10.1016/j.jacc.2016.05.043. Epub
[PubMed PMID: 27470455]
[42]
Reddy SN, Boros MC, Horrow MM. Approach to the Swollen Arm With Chronic Dialysis Access: It's Not Just Deep Vein Thrombosis. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2015 Oct:34(10):1901-10. doi: 10.7863/ultra.15.14.11063. Epub 2015 Aug 25
[PubMed PMID: 26307123]
[43]
Handlos P, Marecová K, Smatanová M, Dvořáček I, Dobiáš M. Fatal Hemorrhage from an Arteriovenous Fistula. Journal of forensic sciences. 2018 Sep:63(5):1577-1581. doi: 10.1111/1556-4029.13730. Epub 2018 Jan 16
[PubMed PMID: 29341134]