[1]
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension (Dallas, Tex. : 1979). 2018 Jun:71(6):e13-e115. doi: 10.1161/HYP.0000000000000065. Epub 2017 Nov 13
[PubMed PMID: 29133356]
Level 3 (low-level) evidence
[2]
Knežević T, Gellineo L, Jelaković A, Premužić V, Dika Ž, Laganović M, Jelaković B. Treatment of Hypertension Induced Albuminuria. Current pharmaceutical design. 2018:24(37):4404-4412. doi: 10.2174/1381612825666181126170354. Epub
[PubMed PMID: 30479206]
[4]
Leru PM,Anton VF,Bumbea H, Nine year follow-up of a rare case of angioedema due to acquired C1-inhibitor deficiency with late onset and good response to attenuated androgen. Allergy, asthma, and clinical immunology : official journal of the Canadian Society of Allergy and Clinical Immunology. 2018
[PubMed PMID: 30386386]
Level 3 (low-level) evidence
[5]
Viberti G, Mogensen CE, Groop LC, Pauls JF. Effect of captopril on progression to clinical proteinuria in patients with insulin-dependent diabetes mellitus and microalbuminuria. European Microalbuminuria Captopril Study Group. JAMA. 1994 Jan 26:271(4):275-9
[PubMed PMID: 8295285]
[6]
Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. The New England journal of medicine. 1993 Nov 11:329(20):1456-62
[PubMed PMID: 8413456]
[7]
Krečak I,Morić Perić M,Zekanović I,Holik H,Coha B,Gverić-Krečak V,Lucijanić M, Beneficial effect of ACE inhibitors on kidney function in polycythemia vera. Wiener klinische Wochenschrift. 2021 Aug
[PubMed PMID: 33555393]
[8]
Yao J, Fan S, Shi X, Gong X, Zhao J, Fan G. Angiotensin-converting enzyme inhibitors versus angiotensin II receptor blockers on insulin sensitivity in hypertensive patients: A meta-analysis of randomized controlled trials. PloS one. 2021:16(7):e0253492. doi: 10.1371/journal.pone.0253492. Epub 2021 Jul 7
[PubMed PMID: 34234365]
Level 1 (high-level) evidence
[9]
Salmenkari H, Korpela R, Vapaatalo H. Renin-angiotensin system in intestinal inflammation-Angiotensin inhibitors to treat inflammatory bowel diseases? Basic & clinical pharmacology & toxicology. 2021 Sep:129(3):161-172. doi: 10.1111/bcpt.13624. Epub 2021 Jun 27
[PubMed PMID: 34128327]
[10]
Chen YJ,Li LJ,Tang WL,Song JY,Qiu R,Li Q,Xue H,Wright JM, First-line drugs inhibiting the renin angiotensin system versus other first-line antihypertensive drug classes for hypertension. The Cochrane database of systematic reviews. 2018 Nov 14
[PubMed PMID: 30480768]
Level 2 (mid-level) evidence
[11]
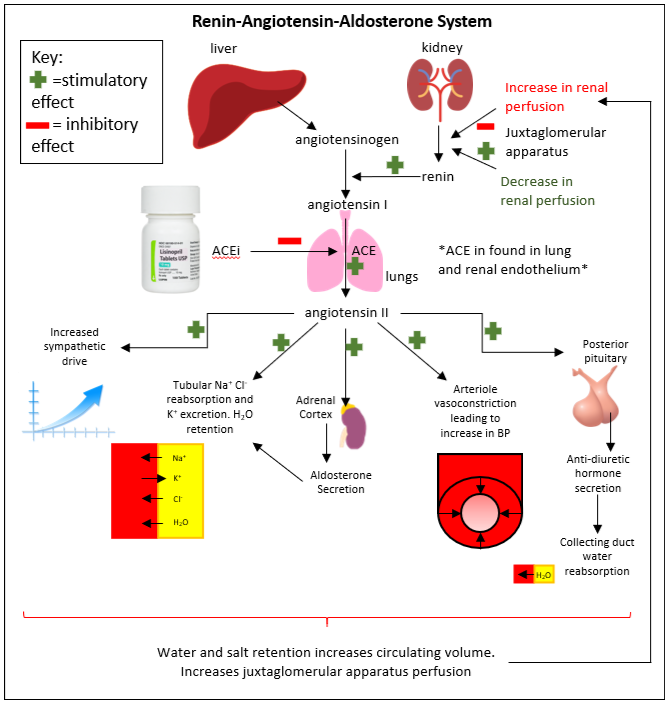
Patel S, Rauf A, Khan H, Abu-Izneid T. Renin-angiotensin-aldosterone (RAAS): The ubiquitous system for homeostasis and pathologies. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie. 2017 Oct:94():317-325. doi: 10.1016/j.biopha.2017.07.091. Epub 2017 Jul 31
[PubMed PMID: 28772209]
[12]
Silva P, Brown RS, Epstein FH. Adaptation to potassium. Kidney international. 1977 Jun:11(6):466-75
[PubMed PMID: 327141]
[13]
Yee AH, Burns JD, Wijdicks EF. Cerebral salt wasting: pathophysiology, diagnosis, and treatment. Neurosurgery clinics of North America. 2010 Apr:21(2):339-52. doi: 10.1016/j.nec.2009.10.011. Epub
[PubMed PMID: 20380974]
[14]
Williams B, Drug discovery in renin-angiotensin system intervention: past and future. Therapeutic advances in cardiovascular disease. 2016 Jun;
[PubMed PMID: 27126389]
Level 3 (low-level) evidence
[15]
Yeo WW,Chadwick IG,Kraskiewicz M,Jackson PR,Ramsay LE, Resolution of ACE inhibitor cough: changes in subjective cough and responses to inhaled capsaicin, intradermal bradykinin and substance-P. British journal of clinical pharmacology. 1995 Nov;
[PubMed PMID: 8703645]
[16]
Lunde H, Hedner T, Samuelsson O, Lötvall J, Andrén L, Lindholm L, Wiholm BE. Dyspnoea, asthma, and bronchospasm in relation to treatment with angiotensin converting enzyme inhibitors. BMJ (Clinical research ed.). 1994 Jan 1:308(6920):18-21
[PubMed PMID: 8298346]
[17]
Malini PL,Strocchi E,Zanardi M,Milani M,Ambrosioni E, Thromboxane antagonism and cough induced by angiotensin-converting-enzyme inhibitor. Lancet (London, England). 1997 Jul 5;
[PubMed PMID: 9217714]
[18]
Matchar DB, McCrory DC, Orlando LA, Patel MR, Patel UD, Patwardhan MB, Powers B, Samsa GP, Gray RN. Systematic review: comparative effectiveness of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers for treating essential hypertension. Annals of internal medicine. 2008 Jan 1:148(1):16-29
[PubMed PMID: 17984484]
Level 2 (mid-level) evidence
[19]
Ghouse J, Ahlberg G, Andreasen L, Banasik K, Brunak S, Schwinn M, Larsen IH, Petersen O, Sørensen E, Ullum H, Rasmussen ER, Eriksson N, Hallberg P, Wadelius M, Bundgaard H, Olesen MS. Association of Variants Near the Bradykinin Receptor B(2) Gene With Angioedema in Patients Taking ACE Inhibitors. Journal of the American College of Cardiology. 2021 Aug 17:78(7):696-709. doi: 10.1016/j.jacc.2021.05.054. Epub
[PubMed PMID: 34384552]
[20]
Kifor I,Moore TJ,Fallo F,Sperling E,Chiou CY,Menachery A,Williams GH, Potassium-stimulated angiotensin release from superfused adrenal capsules and enzymatically dispersed cells of the zona glomerulosa. Endocrinology. 1991 Aug;
[PubMed PMID: 1855477]
[21]
Bakris GL, Weir MR. Angiotensin-converting enzyme inhibitor-associated elevations in serum creatinine: is this a cause for concern? Archives of internal medicine. 2000 Mar 13:160(5):685-93
[PubMed PMID: 10724055]
[22]
Kostis JB, Shelton B, Gosselin G, Goulet C, Hood WB Jr, Kohn RM, Kubo SH, Schron E, Weiss MB, Willis PW 3rd, Young JB, Probstfield J. Adverse effects of enalapril in the Studies of Left Ventricular Dysfunction (SOLVD). SOLVD Investigators. American heart journal. 1996 Feb:131(2):350-5
[PubMed PMID: 8579032]
[23]
Sachs B,Meier T,Nöthen MM,Stieber C,Stingl J, [Drug-induced angioedema : Focus on bradykinin]. Der Hautarzt; Zeitschrift fur Dermatologie, Venerologie, und verwandte Gebiete. 2018 Apr
[PubMed PMID: 29392343]
[24]
Khera R, Clark C, Lu Y, Guo Y, Ren S, Truax B, Spatz ES, Murugiah K, Lin Z, Omer SB, Vojta D, Krumholz HM. Association of Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers With the Risk of Hospitalization and Death in Hypertensive Patients With COVID-19. Journal of the American Heart Association. 2021 Jul 6:10(13):e018086. doi: 10.1161/JAHA.120.018086. Epub 2021 Feb 24
[PubMed PMID: 33624516]
[25]
Wilkins B, Hullikunte S, Simmonds M, Sasse A, Larsen P, Harding SA. Improving the Prescribing Gap For Guideline Recommended Medications Post Myocardial Infarction. Heart, lung & circulation. 2019 Feb:28(2):257-262. doi: 10.1016/j.hlc.2017.10.025. Epub 2017 Nov 14
[PubMed PMID: 29523466]
[26]
Shaikh A. A Practical Approach to Hypertension Management in Diabetes. Diabetes therapy : research, treatment and education of diabetes and related disorders. 2017 Oct:8(5):981-989. doi: 10.1007/s13300-017-0310-3. Epub 2017 Sep 19
[PubMed PMID: 28929319]
[27]
Gubler MC,Antignac C, Renin-angiotensin system in kidney development: renal tubular dysgenesis. Kidney international. 2010 Mar;
[PubMed PMID: 19924102]
[28]
Raebel MA,McClure DL,Simon SR,Chan KA,Feldstein A,Andrade SE,Lafata JE,Roblin D,Davis RL,Gunter MJ,Platt R, Laboratory monitoring of potassium and creatinine in ambulatory patients receiving angiotensin converting enzyme inhibitors and angiotensin receptor blockers. Pharmacoepidemiology and drug safety. 2007 Jan;
[PubMed PMID: 16470693]
[29]
DiBianco R. Adverse reactions with angiotensin converting enzyme (ACE) inhibitors. Medical toxicology. 1986 Mar-Apr:1(2):122-41
[PubMed PMID: 3023783]
[30]
Lip GY, Ferner RE. Poisoning with anti-hypertensive drugs: angiotensin converting enzyme inhibitors. Journal of human hypertension. 1995 Sep:9(9):711-5
[PubMed PMID: 8551483]
[31]
Alzahrani T,Tiu J,Panjrath G,Solomon A, The effect of angiotensin-converting enzyme inhibitors on clinical outcomes in patients with ischemic cardiomyopathy and midrange ejection fraction: a post hoc subgroup analysis from the PEACE trial. Therapeutic advances in cardiovascular disease. 2018 Nov 15
[PubMed PMID: 30442080]
Level 2 (mid-level) evidence
[32]
Brar S, Ye F, James MT, Hemmelgarn B, Klarenbach S, Pannu N, Interdisciplinary Chronic Disease Collaboration. Association of Angiotensin-Converting Enzyme Inhibitor or Angiotensin Receptor Blocker Use With Outcomes After Acute Kidney Injury. JAMA internal medicine. 2018 Dec 1:178(12):1681-1690. doi: 10.1001/jamainternmed.2018.4749. Epub
[PubMed PMID: 30422153]
[33]
Saglimbene V,Palmer SC,Ruospo M,Natale P,Maione A,Nicolucci A,Vecchio M,Tognoni G,Craig JC,Pellegrini F,Lucisano G,Hegbrant J,Ariano R,Lamacchia O,Sasso A,Morano S,Filardi T,De Cosmo S,Pugliese G,Procaccini DA,Gesualdo L,Palasciano G,Johnson DW,Tonelli M,Strippoli GFM, The Long-Term Impact of Renin-Angiotensin System (RAS) Inhibition on Cardiorenal Outcomes (LIRICO): A Randomized, Controlled Trial. Journal of the American Society of Nephrology : JASN. 2018 Nov 12
[PubMed PMID: 30420421]
Level 1 (high-level) evidence
[35]
Simonetti V,Comparcini D,Tomietto M,Pavone D,Flacco ME,Cicolini G, Effectiveness of a family nurse-led programme on accuracy of blood pressure self-measurement: A randomised controlled trial. Journal of clinical nursing. 2021 Apr 19;
[PubMed PMID: 33872417]
Level 1 (high-level) evidence
[36]
Mao CT, Liu MH, Hsu KH, Fu TC, Wang JS, Huang YY, Yang NI, Wang CH. Effect of multidisciplinary disease management for hospitalized heart failure under a national health insurance programme. Journal of cardiovascular medicine (Hagerstown, Md.). 2015 Sep:16(9):616-24. doi: 10.2459/JCM.0000000000000089. Epub
[PubMed PMID: 25105284]