Continuing Education Activity
Distal clavicular osteolysis (DCO) is an overuse injury most often seen in athletes and weight lifters that causes pain in the AC joint. This is an atypical injury with multiple effective treatment modalities. Distal clavicular osteolysis results from repetitive excess load to the AC joint, typically through horizontal adduction, adduction, internal rotation, and forward/lateral flexion of the shoulder, such as bench pressing or overhead lifting. This activity reviews the evaluation and treatment of distal clavicular osteolysis and highlights the role of the interprofessional team in managing patients with this condition.
Objectives:
- Review the etiology of distal clavicular osteolysis.
- Describe the typical patient history and presentation for distal clavicular osteolysis.
- Explain treatment considerations for patients with distal clavicular osteolysis.
- Review the diagnostic imaging findings associated with distal clavicular osteolysis.
Introduction
Distal clavicular osteolysis (DCO) is an atypical injury occurring most often in athletes and weight lifters, specifically those who perform repetitive overhead movements. The clavicle spans two of the four joints of the shoulder. The proximal clavicle interfaces with the sternum at the sternoclavicular (SC) joint, and the distal clavicle adjoins the acromion process to make the acromioclavicular (AC) joint. The AC joint receives its static stability from the AC joint capsule (AC ligaments) and the coracoclavicular ligaments; its dynamic stability from the deltoid and trapezius muscles.[1]
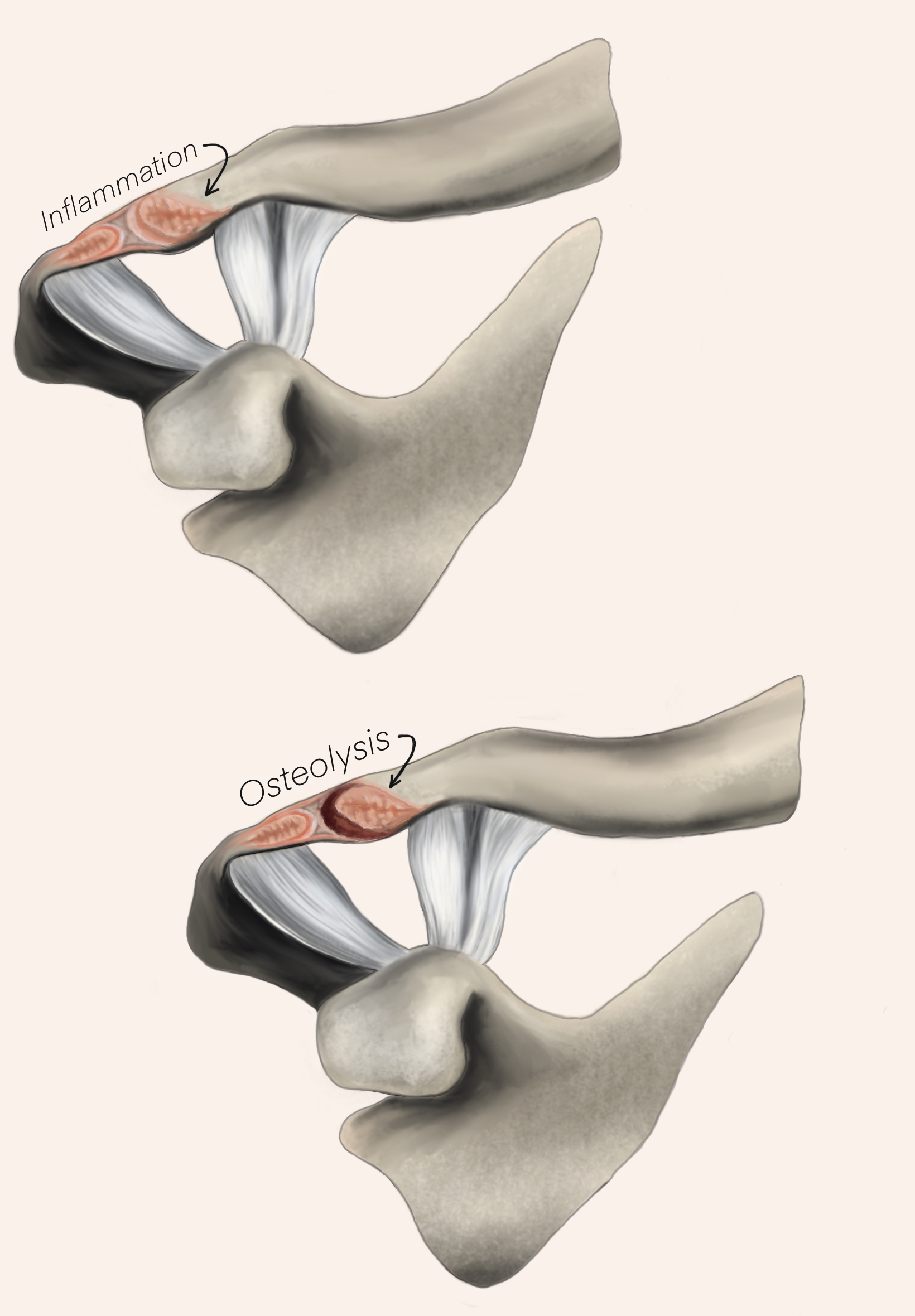
Distal clavicular osteolysis results from repetitive excess load to the AC joint, typically through horizontal adduction, adduction, internal rotation, and forward/lateral flexion of the shoulder, such as bench pressing or overhead lifting. In theory, this repetitive loading causes micro-trauma to the subchondral bone of the distal clavicular head, resulting in subchondral cystic changes, disruption of the articular cartilage, and metaplastic bone formation with increased osteoclastic activity.[2]
Cessation of weight lifting or other inciting activities may alleviate symptoms. Some therapies have shown promise to decrease pain and improve function.[3]
Etiology
The most common aggravating activities in distal clavicular osteolysis are bench pressing, overhead lifting, and overhead athletic movements such as volleyball, basketball, tennis, and swimming.[4]
These movements cause frequent traction and compression loading of the AC joint, which leads to the repetitive microtrauma pattern implicated in DCO. One of the most associated causes of DCO is the bench press, specifically high-intensity bench press, defined as a one-rep maximum of more than 1.5 times the individual's body weight.[5]
Epidemiology
Distal clavicular osteolysis is almost exclusively a diagnosis of young athletes and weight lifters, particularly those engaging in repetitive pressing or overhead activities. However, there is no limit to the age at which DCO can occur physiologically. Historically, DCO was exclusively a disease of young male weightlifters and athletes, but it is now known to appear in females engaged in similar provoking activities.[4]
A retrospective study of 1,432 MRI results of 13 to 19-year-olds with shoulder pain attributed 6.5% of the cases to DCO based on imaging findings, 24% of whom were female.[3]
Pathophysiology
The pathophysiology of DCO is controversial, but according to Schwarzkopf et al., Cahill presented the most widely accepted theory, which described microfractures of the subchondral bone and repeated attempts at repair.[2]
Repetitive stress increases osteolytic and osteoblastic activity, further disrupting the articular cartilage and metaplastic bone formation. Kassarjian et al. further supported the atraumatic repetitive stress hypothesis in their MR evaluation which demonstrated that all patients with apparent DCO displayed a hypo-intense line in the distal clavicle most consistent with a subchondral fracture.[6]
Additionally, findings include subchondral cysts and increased osteoblastic and osteoclastic activity.[2]
History and Physical
Patients presenting with distal clavicular osteolysis typically reveal a history of weight lifting, frequent repetitive overhead movements (typically from various sports), or trauma to the AC joint.[4]
Often, the account includes an increased emphasis on bench pressing or similar activities that increase traction or compression stress on the AC joint. These movements worsen pain (i.e., bench pressing, hang cleans, overhead press). They also likely have a pattern of pain improving with cessation of instigating activities and then worsening on resumption of activity. A typical presentation features the gradual onset of dull aching pain, which may be unilateral or bilateral over the distal clavicle and AC joint.
A physical exam denotes pain with palpation over the area of the AC joint. Strength is often preserved but may have some pain inhibition during testing. Range of motion is also typically complete and pain-free outside of the extremes of shoulder abduction and internal rotation. Loading of the AC joint through Hawkins and Scarf tests elicits pain. Including a cervical spine and neurologic exam helps rule out referred pain.[2]
Evaluation
Plain film radiology of the AC joint is typically sufficient to evaluate for distal clavicular osteolysis. Imaging of DCO often demonstrates microcysts, loss of subchondral bone detail, and osteolysis of the distal clavicle.
Early, mild, or unclear radiograph findings warrant considering other imaging modalities such as MRI, bone scan, or ultrasound. Diagnostic musculoskeletal ultrasound is an emerging option for diagnosing DCO. Ultrasound may be performed during evaluation by a trained clinician and is significantly less expensive than MRI and bone scan. It may also be more sensitive than plain film x-ray.[7]
The imaging modality selection warrants consideration of the differential diagnosis or concomitant pain generators. For example, high suspicion of SLAP lesion in addition to SCO requires magnetic resonance to evaluate adequately. No laboratory tests are necessary for the diagnosis but should be considered based on other medical causes in the differential.
Treatment / Management
The first-line therapy for distal clavicular osteolysis remains conservative with activity modification/avoidance, nonsteroidal anti-inflammatory medication use, and physical therapy.[8] Although no studies or position statements to date advocate a specific physical therapy regimen for DCO, restoring flexibility and rotator cuff strength are standard recommendations for those with additional shoulder pathology.[8]
Modification of bench press motion modification is widely recommended. Narrowing barbell hand placement to less than 1.5 times the bi-acromial width and controlling the descent phase of the bench press to end 4 to 6 cm over the anterior chest, often aided by a towel or spacer use, can help decrease the stress placed on the distal clavicle.[2]
An essential adjunct to conservative management is corticosteroid injection. Intra-articular AC joint injection may be beneficial therapeutically and diagnostically. It can help correctly identify the primary pain generator by decreasing pain and improving function. If pain is not improved after injection, other targeted injections can evaluate for alternate shoulder pathology.[8]
An emerging option for treating intractable DCO-associated pain is botulinum toxin injection. A case study showed benefit to one patient with severe, intractable DCO-associated pain, citing the antinociceptive properties of botulinum toxin injection, specifically in osteoarthritis, as evidence of the mechanism of action.[9]
No current literature demonstrates the efficacy of orthobiologic injectables, such as platelet-rich plasma, bone marrow aspirate concentrate, or adipose-derived mesenchymal stem cells.
Surgical management can be highly effective for those who fail nonoperative management or athletes unable to modify specific athletic tasks and activities. The mainstay of surgical intervention is resectioning the distal clavicle with no more than 8 mm of excision to avoid iatrogenic AC joint instability. This is performed through an open or arthroscopic technique.[1]
The open procedure offers the surgeon direct visualization and the ability to adjust the resection margin with a broader frame of reference. Additionally, many patients have a large superior osteophyte, which is more easily resected through an open approach. Recovery time for the open approach ranges from 5 to 12 weeks. The argument against the open technique is that it disrupts the deltotrapezial fascia superiorly.[2]
The two arthroscopic approaches are direct and indirect. The advantages of these techniques are less tissue dissection and potentially an earlier return to sport and recovery.[2] The direct approach utilizes two portals, one located 1 cm posterior to the AC joint and the other 1 cm anterior.
The indirect method requires three portals (anterior, posterior, and lateral), utilizing the subacromial space to visualize the inferior AC joint capsule. Both procedures involve a cutting burr to remove no more than 8 mm of the distal end of the clavicle to preserve the anterior and posterior AC ligaments.
In a study directly comparing the two approaches, out of 34 patients included in the final analysis, all reported excellent outcomes and returned to sport except for one treatment failure. However, the study noted that the direct approach had a faster return to sport time with a mean of 21 days compared to a 42-day average for the indirect approach. Functional performance measures were also higher in the direct approach group at all postoperative assessments.[10]
Differential Diagnosis
The differential diagnosis for distal clavicular osteolysis includes AC joint arthritis, subacromial bursitis, superior labral (SLAP) tears, and other musculoskeletal causes of superior shoulder pain.
These additional causes are difficult to differentiate based solely on a physical exam, so imaging is often pursued based on the most likely diagnoses. Non-musculoskeletal etiologies also warrant consideration, such as hyperparathyroidism, gout, scleroderma, rheumatoid arthritis, multiple myeloma, infection, and Gorham disease. Complete cervical spine and neurovascular evaluations are essential if referred pain is suspected.[2]
Most comorbid medical conditions are ruled out through a good physical exam, given the younger demographic of DCO. Consider laboratory and imaging studies based on a patient's risk factors for a specific medical illness, such as a family history of autoimmune disease or additional symptoms pointing towards a medical diagnosis.
Prognosis
The prognosis of DCO is generally excellent. In one radiology-based study, 93% of patients were successfully treated with conservative therapy.[4]
No current identified studies specify a regimen or algorithm for treatment, but most include NSAIDs, post-activity icing, and activity modification.[2] Restrictions may be temporary, but sometimes long-term conservative management is only successful with continued cessation of causative activity, which may not be feasible for high-level athletes, labor workers, or warfighters.[11].
Surgical interventions are effective, and with newer arthroscopic approaches, a return to sports/activity is faster and more successful.[1]
Complications
Resorption of the distal clavicle is a notable mark of pathology progression in patients who do not restrict painful movements and, in a sense, cause a "self-surgery."[2]
One long-term study of the sequelae of DCO using MRI imaging found that the most common long-term complications of DCO are AC joint widening and AC joint osteoarthritis. However, the significance of the MRI findings is not known, as not all patients with the finding were symptomatic.[12]
Deterrence and Patient Education
As with other overuse injuries, the limitation of provocative maneuvers, such as repetitive loading and traction of the AC joint, can prevent the worsening of DCO. Young athletes who participate in sports with repetitive overhead movements benefit from cross-training in other activities with less loading of the AC joint. A specifically identified risk factor is high-intensity bench pressing a one-rep max of more than 1.5 times body weight.[5]
Low-intensity bench press was not a risk factor in this study. However, the risk of DCO increased with bench pressing frequency (more than once per week), intensity (more than 1.5 times body weight), and duration (more than five years), both individually and with cumulative risk.[5]
Additionally, avoiding over-reliance on push-ups, dips, and straight bar bench pressing for chest and triceps strengthening can help limit AC joint stress. Substitution of a cable crossover, dumbbell decline, incline, and narrow grip bench press can be preventative and risk-mitigating following diagnosis.[2]
Enhancing Healthcare Team Outcomes
Early identification and intervention are imperative to limit time away from activity for athletes. Distal clavicular osteolysis should be on the differential for any patient presenting for AC joint or superior shoulder pain evaluation.
Athletic trainers and primary care physicians should be empowered to obtain imaging of these patients, especially ultrasound or plain radiographs, as these are the most cost-effective ways of identifying distal clavicular osteolysis. Frontline healthcare workers must receive education to guide the patient through various conservative measures, including injections, appropriate activity modifications, or surgical intervention.
Musculoskeletal specialists such as athletic trainers, strength coaches, physical therapists, sports medicine physicians, and orthopedists are well suited to diagnose and manage DCO. Shared decision-making allows for counseling these specific patients and identifying their goals and treatment options. Overall, optimal care requires a multi-disciplinary team approach to healthcare that can identify them and provide them with their definitive treatment most effectively.