[1]
Chapman T, Ilyas AM. Pyogenic Flexor Tenosynovitis: Evaluation and Treatment Strategies. Journal of hand and microsurgery. 2019 Dec:11(3):121-126. doi: 10.1055/s-0039-1700370. Epub 2019 Nov 2
[PubMed PMID: 31814662]
[2]
Pang HN, Teoh LC, Yam AK, Lee JY, Puhaindran ME, Tan AB. Factors affecting the prognosis of pyogenic flexor tenosynovitis. The Journal of bone and joint surgery. American volume. 2007 Aug:89(8):1742-8
[PubMed PMID: 17671013]
[3]
Stern PJ, Staneck JL, McDonough JJ, Neale HW, Tyler G. Established hand infections: a controlled, prospective study. The Journal of hand surgery. 1983 Sep:8(5 Pt 1):553-9
[PubMed PMID: 6355263]
[4]
Kennedy CD, Huang JI, Hanel DP. In Brief: Kanavel's Signs and Pyogenic Flexor Tenosynovitis. Clinical orthopaedics and related research. 2016 Jan:474(1):280-4. doi: 10.1007/s11999-015-4367-x. Epub 2015 May 29
[PubMed PMID: 26022113]
[5]
Kennedy CD, Lauder AS, Pribaz JR, Kennedy SA. Differentiation Between Pyogenic Flexor Tenosynovitis and Other Finger Infections. Hand (New York, N.Y.). 2017 Nov:12(6):585-590. doi: 10.1177/1558944717692089. Epub 2017 Feb 1
[PubMed PMID: 28720000]
[6]
Patel DB, Emmanuel NB, Stevanovic MV, Matcuk GR Jr, Gottsegen CJ, Forrester DM, White EA. Hand infections: anatomy, types and spread of infection, imaging findings, and treatment options. Radiographics : a review publication of the Radiological Society of North America, Inc. 2014 Nov-Dec:34(7):1968-86. doi: 10.1148/rg.347130101. Epub
[PubMed PMID: 25384296]
[7]
Ochiai N, Matsui T, Miyaji N, Merklin RJ, Hunter JM. Vascular anatomy of flexor tendons. I. Vincular system and blood supply of the profundus tendon in the digital sheath. The Journal of hand surgery. 1979 Jul:4(4):321-30
[PubMed PMID: 469207]
[8]
Schnall SB, Vu-Rose T, Holtom PD, Doyle B, Stevanovic M. Tissue pressures in pyogenic flexor tenosynovitis of the finger. Compartment syndrome and its management. The Journal of bone and joint surgery. British volume. 1996 Sep:78(5):793-5
[PubMed PMID: 8836073]
[9]
Aguiar RO, Gasparetto EL, Escuissato DL, Marchiori E, Trudell DJ, Haghighi P, Resnick D. Radial and ulnar bursae of the wrist: cadaveric investigation of regional anatomy with ultrasonographic-guided tenography and MR imaging. Skeletal radiology. 2006 Nov:35(11):828-32
[PubMed PMID: 16688447]
[10]
SCHELDRUP EW. Tendon sheath patterns in the hand; an anatomical study based on 367 hand dissections. Surgery, gynecology & obstetrics. 1951 Jul:93(1):16-22
[PubMed PMID: 14855245]
[11]
Goyal K, Speeckaert AL. Pyogenic Flexor Tenosynovitis: Evaluation and Management. Hand clinics. 2020 Aug:36(3):323-329. doi: 10.1016/j.hcl.2020.03.005. Epub
[PubMed PMID: 32586458]
[12]
Abrams RA, Botte MJ. Hand Infections: Treatment Recommendations for Specific Types. The Journal of the American Academy of Orthopaedic Surgeons. 1996 Jul:4(4):219-230
[PubMed PMID: 10795057]
[13]
Harris PA, Nanchahal J. Closed continuous irrigation in the treatment of hand infections. Journal of hand surgery (Edinburgh, Scotland). 1999 Jun:24(3):328-33
[PubMed PMID: 10433448]
[14]
Small LN, Ross JJ. Suppurative tenosynovitis and septic bursitis. Infectious disease clinics of North America. 2005 Dec:19(4):991-1005, xi
[PubMed PMID: 16297744]
[15]
Schaefer RA, Enzenauer RJ, Pruitt A, Corpe RS. Acute gonococcal flexor tenosynovitis in an adolescent male with pharyngitis. A case report and literature review. Clinical orthopaedics and related research. 1992 Aug:(281):212-5
[PubMed PMID: 1499214]
Level 3 (low-level) evidence
[16]
Dailiana ZH, Rigopoulos N, Varitimidis S, Hantes M, Bargiotas K, Malizos KN. Purulent flexor tenosynovitis: factors influencing the functional outcome. The Journal of hand surgery, European volume. 2008 Jun:33(3):280-5. doi: 10.1177/1753193408087071. Epub
[PubMed PMID: 18562357]
[17]
Katsoulis E, Bissell I, Hargreaves DG. MRSA pyogenic flexor tenosynovitis leading to digital ischaemic necrosis and amputation. Journal of hand surgery (Edinburgh, Scotland). 2006 Jun:31(3):350-2
[PubMed PMID: 16616976]
[18]
Langer MF, Grünert JG, Unglaub F, Ueberberg J, Glasbrenner J, Oeckenpöhler S. [Pyogenic Flexor Tenosynovitis]. Handchirurgie, Mikrochirurgie, plastische Chirurgie : Organ der Deutschsprachigen Arbeitsgemeinschaft fur Handchirurgie : Organ der Deutschsprachigen Arbeitsgemeinschaft fur Mikrochirurgie der Peripheren Nerven und Gefasse : Organ der V.... 2021 Jun:53(3):267-275. doi: 10.1055/a-1472-1689. Epub 2021 Jun 16
[PubMed PMID: 34134159]
[19]
Hyatt BT, Bagg MR. Flexor Tenosynovitis. The Orthopedic clinics of North America. 2017 Apr:48(2):217-227. doi: 10.1016/j.ocl.2016.12.010. Epub
[PubMed PMID: 28336044]
[20]
Draeger RW, Bynum DK Jr. Flexor tendon sheath infections of the hand. The Journal of the American Academy of Orthopaedic Surgeons. 2012 Jun:20(6):373-82. doi: 10.5435/JAAOS-20-06-373. Epub
[PubMed PMID: 22661567]
[21]
Giladi AM, Malay S, Chung KC. A systematic review of the management of acute pyogenic flexor tenosynovitis. The Journal of hand surgery, European volume. 2015 Sep:40(7):720-8. doi: 10.1177/1753193415570248. Epub 2015 Feb 10
[PubMed PMID: 25670687]
Level 1 (high-level) evidence
[22]
Paniagua CT, Bean AS. Pyogenic flexor tenosynovitis: assessment and management in the emergency department setting. Advanced emergency nursing journal. 2014 Jan-Mar:36(1):36-43. doi: 10.1097/TME.0000000000000002. Epub
[PubMed PMID: 24487262]
[23]
Siska RC, Davidson AL, Driscoll CR, Browne DT, Maus JC, Prabhu SS, Rudolph MA, Schneider MA, Runyan CM, Reynolds M. A1 Pulley Tenderness as a Modification to Tenderness along the Flexor Sheath in Diagnosing Pyogenic Flexor Tenosynovitis. Plastic and reconstructive surgery. Global open. 2022 Mar:10(3):e4165. doi: 10.1097/GOX.0000000000004165. Epub 2022 Mar 2
[PubMed PMID: 35261842]
[24]
Yi A, Kennedy C, Chia B, Kennedy SA. Radiographic Soft Tissue Thickness Differentiating Pyogenic Flexor Tenosynovitis From Other Finger Infections. The Journal of hand surgery. 2019 May:44(5):394-399. doi: 10.1016/j.jhsa.2019.01.013. Epub 2019 Feb 21
[PubMed PMID: 30797654]
[25]
Jardin E, Delord M, Aubry S, Loisel F, Obert L. Usefulness of ultrasound for the diagnosis of pyogenic flexor tenosynovitis: A prospective single-center study of 57 cases. Hand surgery & rehabilitation. 2018 Apr:37(2):95-98. doi: 10.1016/j.hansur.2017.12.004. Epub 2018 Feb 1
[PubMed PMID: 29396150]
Level 3 (low-level) evidence
[26]
Chaudhary S, Maji S, Garg V, Singh V. Isolated multidrug-resistant tubercular tenosynovitis of the flexor tendon of the little finger. BMJ case reports. 2021 Feb 19:14(2):. doi: 10.1136/bcr-2020-238339. Epub 2021 Feb 19
[PubMed PMID: 33608337]
Level 3 (low-level) evidence
[27]
Myers DM, Goubeaux C, Skura B, Warmoth PJ, Taylor BC. Contrast Enhanced Computed Tomography in the Diagnosis of Acute Pyogenic Flexor Tenosynovitis. Hand (New York, N.Y.). 2023 Nov:18(8):1323-1329. doi: 10.1177/15589447221092058. Epub 2022 May 24
[PubMed PMID: 35611491]
[28]
Millerioux S, Rousset M, Canavese F. Pyogenic tenosynovitis of the flexor hallucis longus in a healthy 11-year-old boy: a case report and review of the literature. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2013 Nov:23 Suppl 2():S311-5. doi: 10.1007/s00590-012-1147-0. Epub 2012 Dec 8
[PubMed PMID: 23412272]
Level 3 (low-level) evidence
[29]
Latario L, Abeler J, Clegg S, Thurber L, Igiesuorobo O, Jones M. Antibiotics Versus Surgery in Treatment of Early Flexor Tenosynovitis. Hand (New York, N.Y.). 2023 Jul:18(5):804-810. doi: 10.1177/15589447211043187. Epub 2022 Jan 26
[PubMed PMID: 35081807]
[30]
Carter SJ, Burman SO, Mersheimer WL. Treatment of digital tenosynovitis by irrigation with peroxide and oxytetracycline: review of nine cases. Annals of surgery. 1966 Apr:163(4):645-50
[PubMed PMID: 5934641]
Level 3 (low-level) evidence
[31]
Born TR, Wagner ER, Kakar S. Comparison of Open Drainage Versus Closed Catheter Irrigation for Treatment of Suppurative Flexor Tenosynovitis. Hand (New York, N.Y.). 2017 Nov:12(6):579-584. doi: 10.1177/1558944716675131. Epub 2016 Oct 25
[PubMed PMID: 29091483]
[32]
Gutowski KA, Ochoa O, Adams WP Jr. Closed-catheter irrigation is as effective as open drainage for treatment of pyogenic flexor tenosynovitis. Annals of plastic surgery. 2002 Oct:49(4):350-4
[PubMed PMID: 12370638]
[33]
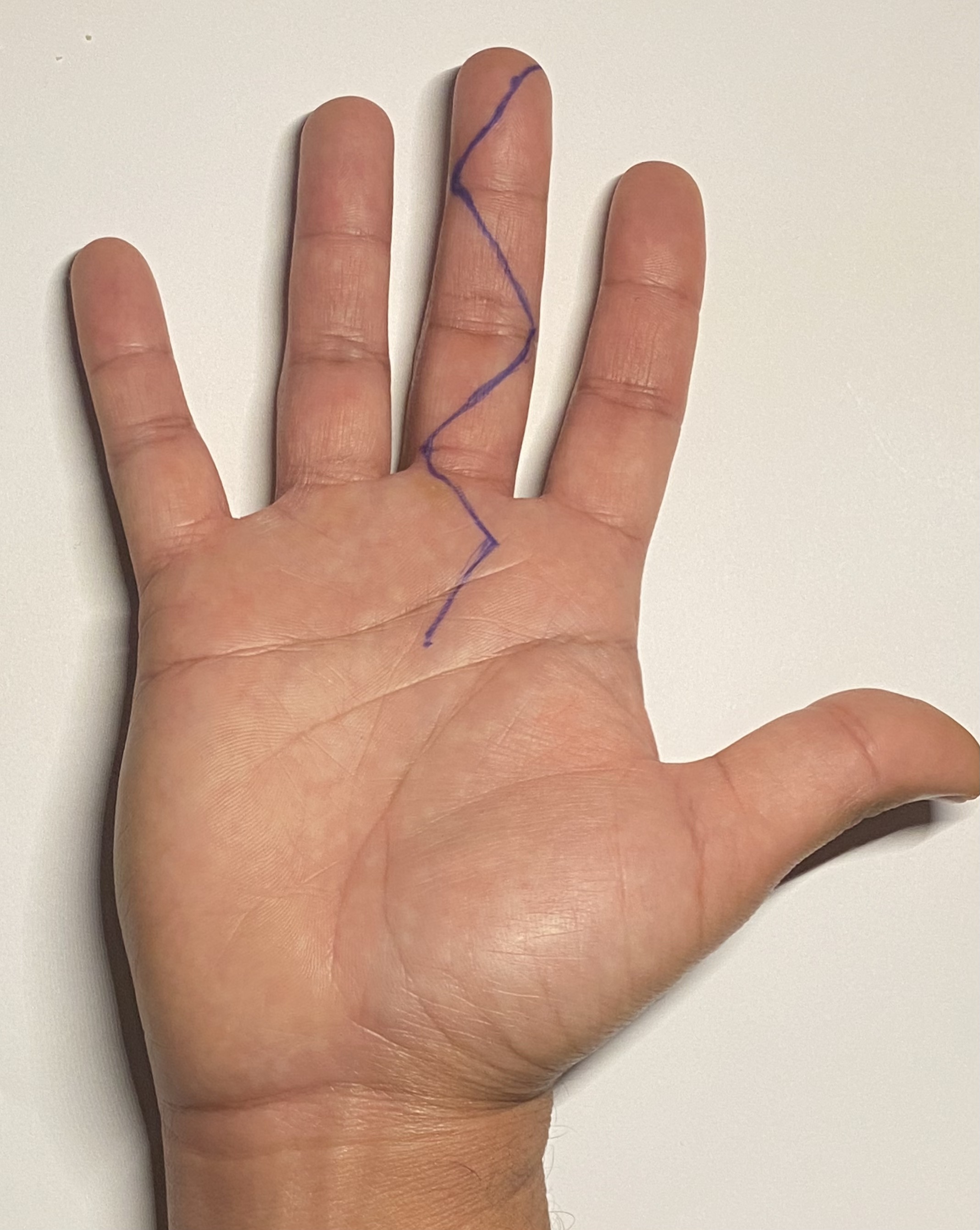
Bruner JM. The zig-zag volar-digital incision for flexor-tendon surgery. Plastic and reconstructive surgery. 1967 Dec:40(6):571-4
[PubMed PMID: 6077719]
[35]
Dujeux C, Cottebrune T, Malherbe M, Michon J, Fournier A, Hulet C. Use of antibiotics in pyogenic flexor tenosynovitis. Hand surgery & rehabilitation. 2022 Oct:41(5):624-630. doi: 10.1016/j.hansur.2022.07.006. Epub 2022 Aug 3
[PubMed PMID: 35933026]
[36]
McDonald LS, Bavaro MF, Hofmeister EP, Kroonen LT. Hand infections. The Journal of hand surgery. 2011 Aug:36(8):1403-12. doi: 10.1016/j.jhsa.2011.05.035. Epub
[PubMed PMID: 21816297]
[39]
Koshy JC, Bell B. Hand Infections. The Journal of hand surgery. 2019 Jan:44(1):46-54. doi: 10.1016/j.jhsa.2018.05.027. Epub 2018 Jul 14
[PubMed PMID: 30017648]
[40]
Lille S, Hayakawa T, Neumeister MW, Brown RE, Zook EG, Murray K. Continuous postoperative catheter irrigation is not necessary for the treatment of suppurative flexor tenosynovitis. Journal of hand surgery (Edinburgh, Scotland). 2000 Jun:25(3):304-7
[PubMed PMID: 10961561]
[41]
Gaston RG, Greenberg JA. Use of continuous marcaine irrigation in the management of suppurative flexor tenosynovitis. Techniques in hand & upper extremity surgery. 2009 Dec:13(4):182-6. doi: 10.1097/BTH.0b013e3181bef5a3. Epub
[PubMed PMID: 19956043]