Continuing Education Activity
A cataract is an ocular condition that refers to the opacification of the crystalline lens leading to visual impairment. A complicated Cataract is a secondary form of cataract that occurs secondary to an intra-ocular disease. A timely diagnosis and appropriate management is the key to a good visual outcome. This activity illustrates the etiology, evaluation, and management of complicated cataracts and highlights the role of an inter-professional team in evaluating and treating a patient diagnosed with complicated cataracts.
Objectives:
- Outline the etiology of complicated cataracts.
- Describe the clinical examination of the patients presenting with complicated cataracts in detail.
- Summarize the management, including medical, surgical, and post-operative, of complicated cataracts.
- Identify the importance of improving the coordination among the health care team for providing a better outcome to the patient.
Introduction
A cataract is an opacification of the eye's crystalline lens that prevents the light rays from reaching the retina, leading to a visual impairment that significantly affects the patient's quality of life. A complicated cataract refers to the opacification of the crystalline lens secondary to intraocular diseases, mainly intraocular inflammatory conditions that include anterior, intermediate, or posterior uveitis. However, other intraocular conditions have also been identified that lead to the development of complicated cataracts. It is especially disabling in the younger age group because of the visual impairment and need for cataract surgery with its own complications.[1]
Cataract formation in uveitis occurs due to uncontrolled inflammation and also because of the use of steroids. Managing the case of a complicated cataract is a challenging task for an ophthalmologist, as it also requires meticulous control of the inflammation and management of the primary intraocular disease. Hence, a multidisciplinary approach is required.[2]
Etiology
The various intraocular conditions leading to complicated cataracts are:
- Inflammatory conditions include inflammations of the uveal tract (iridocyclitis, pars planitis, posterior uveitis), hypopyon corneal ulcer, and endophthalmitis. The cataract begins as a posterior subcapsular cataract mainly.[3]
- Degenerative conditions include essential iris atrophy, Retinitis Pigmentosa, myopic chorioretinal degenerations, and other pigmentary retinal dystrophies. The development of cataracts is the most common complication of retinitis pigmentosa in the anterior segment.[4] The cataract begins as a Posterior Subcapsular cataract. It can be anterior polar or nuclear.
- Retinal detachment – longstanding cases of retinal detachment can lead to complicated cataracts.
- Glaucoma- primary or secondary glaucoma. Glaucomfleckens are grey-white epithelial and anterior cortical lens opacities following an episode of highly raised intraocular pressure.
- Intraocular tumors- retinoblastoma, melanoma, metastatic tumors involving the choroid or the anterior segment, can lead to complicated cataracts.
Clinically, most complicated cataracts occur secondary to chronic intraocular inflammation due to the various causes mentioned above and the use of corticosteroids in treating the inflammation. Hence, detailed knowledge of the primary intraocular condition is required to manage the condition skillfully.
Epidemiology
Cataract has emerged as a leading cause of visual impairment and blindness. It has been estimated that approximately 20 million people are blind because of cataracts. Complicated cataracts develop as one of the most common complications of chronic uveitis or recurrent uveitis. Complicated cataracts occur secondary to intraocular inflammation and steroid therapy, accounting for about 40% of the visual disability in patients with uveitis.
Complicated cataract surgery due to uveitis comprises almost 1.2% of all cataract surgeries. The prevalence of acquired cataracts increases with age. In 2013, there were more than 22 million people in the United States who had cataracts, with a prevalence of 30.1 million in 2020. The incidence of cataracts increases with age affecting about 70% of people over the age of 80 years. Females are more commonly affected.[5]
Pathophysiology
The crystalline lens is an avascular structure. It derives nutrition mainly from intraocular fluids. In complicated cataracts, the metabolism of the lens is deranged due to the diffusion of toxins released in the ocular fluids either due to inflammation or degenerative conditions. The posterior capsule of the lens is thin and lacks epithelial support; hence the toxins diffuse posteriorly, leading to the development of opacification in the posterior pole at the earliest stage. A posterior subcapsular cataract is the commonest manifestation of complicated cataracts.
History and Physical
A thorough history, detailed ophthalmic and systemic examination must be carried out to reach the diagnosis. The primary intraocular condition must be diagnosed and treated.
History
- Diminution of vision
- Duration of onset
- Mode of onset
- Progression
- Nature
- Diurnal variation
- Associated symptoms such as pain, redness, watering of the eyes
- Associated flashes, floaters, colored haloes, glare, diplopia
- History of recurrent episodes of pain, redness in the eyes
- Treatment history of steroids, immunosuppressive drugs, any surgical procedure, any chemotherapy for intraocular tumors
- Trauma
- Systemic illness such as diabetes mellitus, hypertension, any autoimmune disease, tuberculosis, sarcoidosis
General Physical Examination
- Pulse rate, respiratory rate, blood pressure
- Systemic examination - to look for any systemic illness
Comprehensive Ophthalmic Examination
- Visual Acuity
- Uncorrected visual acuity
- Refraction
- Best-corrected visual acuity
- Near vision
- Intraocular pressure (IOP) – by Goldmann applanation tonometry to rule out glaucoma and hypotony
- Examination of the lacrimal system- to rule out any lacrimal system obstruction
- Pupillary reactions - direct and consensual to assess the status of the optic nerve
- Slit-lamp Examination – should be meticulously carried
- Cornea: Edema, keratic precipitates, corneal ulcer, opacities, scars.
- Anterior chamber: Depth, cells, and flare in the anterior chamber, hypopyon.
- Iris: Heterochromia, atrophy, iridodonesis, vascularisation, synechiae.
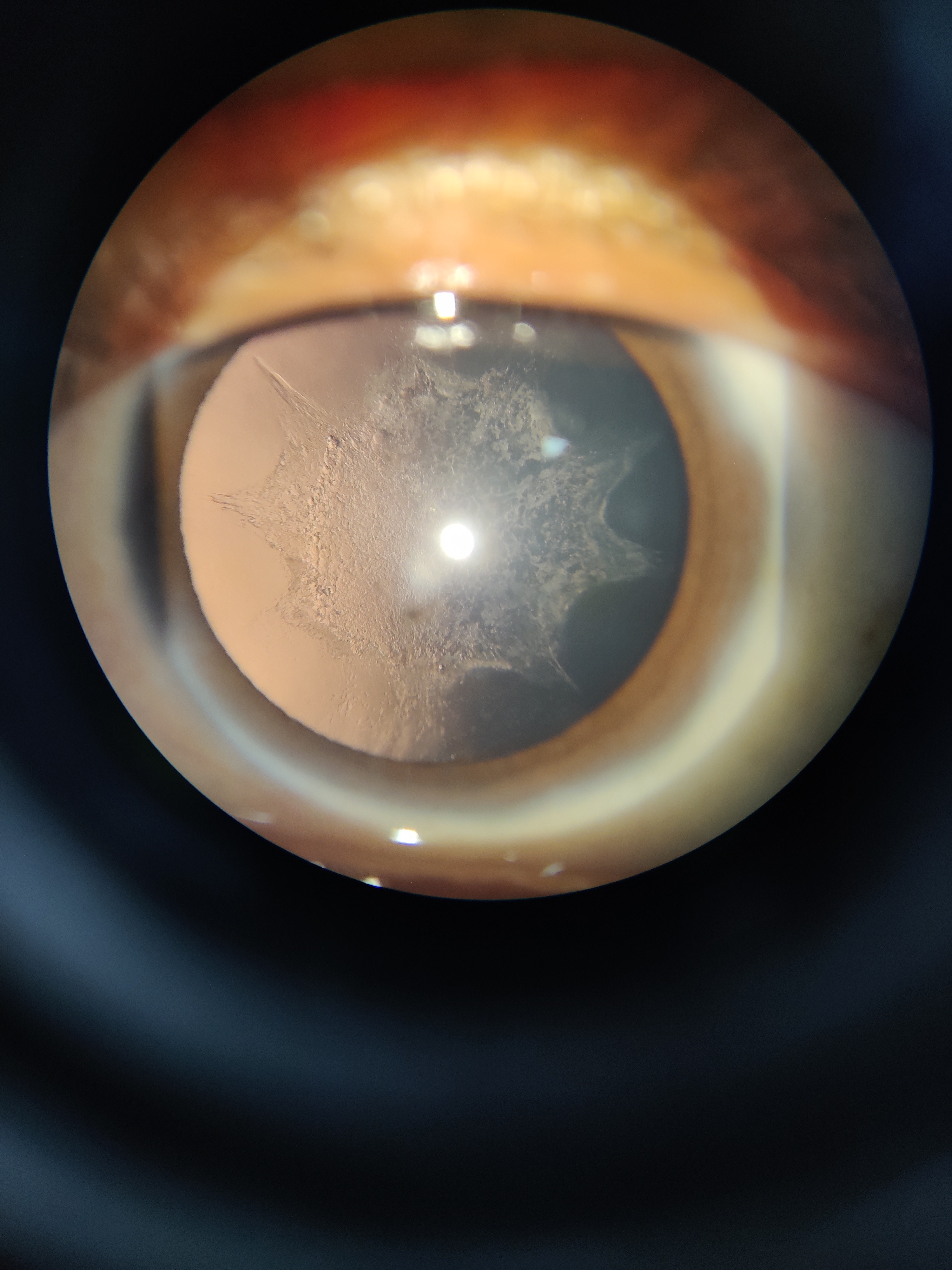
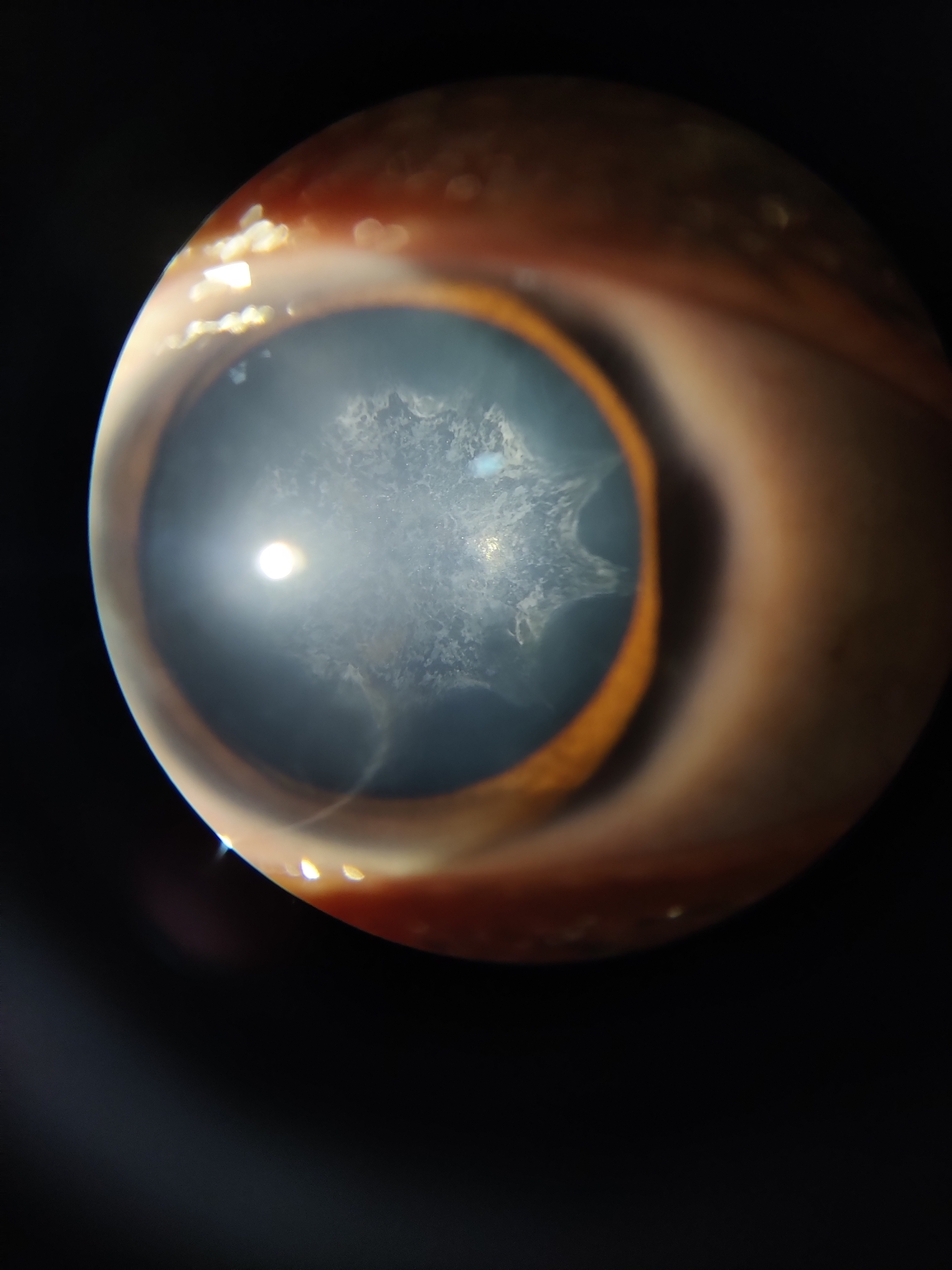
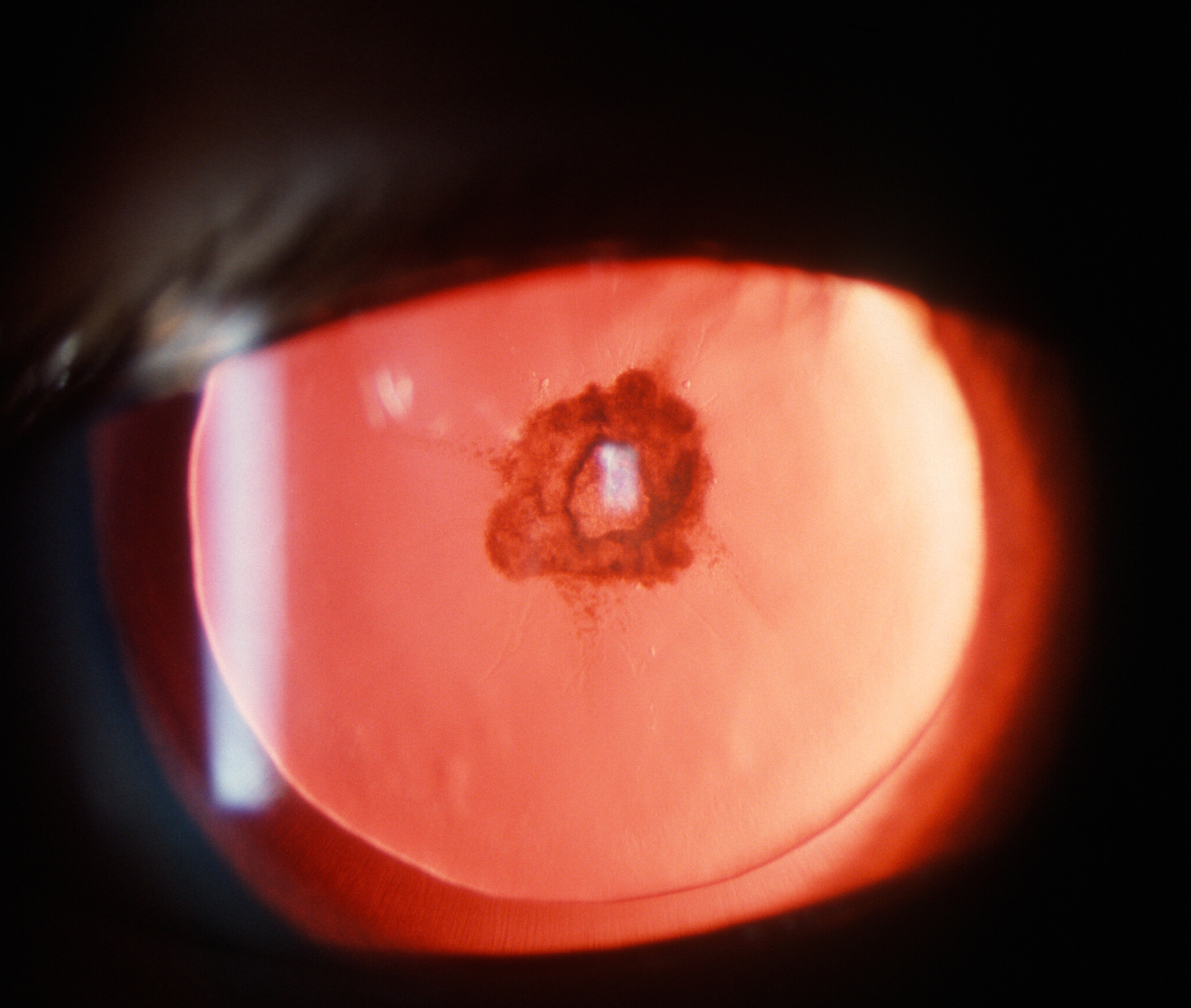
- The crystalline lens – anterior and posterior capsular status, grading of the cataract, zonular status, phacodonesis The cataract typically begins as a posterior subcapsular cortical cataract. The opacity is irregular in outline, appearing as 'BREADCRUMB' in the slit lamp. A characteristic sign is the appearance of iridescent colored particles "polychromatic lusture" of reds, greens, and blues. Gradually the opacity spreads in the remaining cortex, finally developing into a total cataract. Deposition of calcium is commonly seen in the later stage. In some anterior segment lesions, the anterior cortical cataract may occur. Anterior cortical cataracts may be seen in the presence of glaucoma, hypopyon corneal ulcer, and acute iritis.[6]
- Vitreous – Anterior 1/3 of the vitreous can be examined by slit lamp for any opacities, cells in the vitreous cavity.
- Slit-lamp biomicroscopy - To look for macular status. For example, macular ischemia, chronic macular edema, or any macular scar might result from the choroidal neovascular membrane. The status of the optic disc should also be assessed for glaucomatous optic disc changes.
- Dilated fundus examination- Carried out using indirect ophthalmoscopy to look for retinal pathologies. In the presence of retinal detachment, the extent of the detachment should be ascertained, and retinal breaks identified. Macular involvement is documented. The peripheral retina and the pars plana should be examined by scleral indentation for intermediate uveitis. The retina is examined for degenerative retinal conditions: retinitis pigmentosa is commonly associated with the development of cataracts.[7] The classic triad in retinitis pigmentosa comprises bony spicules in the mid periphery, waxy disc pallor, and arteriolar attenuation. Any choroidal tumors should be identified.
Evaluation
When visual loss is mainly secondary to cataract formation, the maximal benefit is obtained with cataract surgery. The postoperative outcome depends upon several factors, including the diagnosis, proper perioperative management, and meticulous surgery. Diseases that only involve the anterior segment generally have a better prognosis than those that affect the posterior segment. The visual potential of the eye should be carefully determined before planning cataract surgery, as this will directly impact the visual outcome. Investigations are performed to identify the coexisting ocular pathologies that may contribute to surgical challenges or warrant combined or staged procedures.
Laboratory Investigations
- Blood and routine investigations:
- Complete hemogram
- Erythrocyte sedimentation rate
- C- reactive protein
- Blood sugar
- Other tests (based on history and clinical examination)
- Sputum test for acid-fast bacilli (to rule out tuberculosis)
- NCCT scan chest for tuberculosis, sarcoidosis
- Serum calcium, serum ACE enzyme for sarcoidosis
- VDRL for syphilis
- TORCH profile
- RA factor for rheumatoid arthritis
- Serum ANA, p-anca, c-anca for other autoimmune conditions
Ocular Investigations
- Gonioscopy- To look for anterior chamber angle status.
- Laser flare meter - To measure flare in the anterior chamber and can also be used to guide therapy.
- Ultrasound B scan- To look for the status of the retina in case of total opacification of the lens, to rule out choroidal effusion, and identify any intraocular tumors.
- Ultrasound biomicroscopy- Should be done in the eyes with hypotony to look for the status of the ciliary body and its processes, zonular status, status of the posterior capsule, and cyclitic membranes.
- Optical coherence tomography of the macula- To assess the thickness of the macula, presence of any neovascular membrane, epiretinal membrane.
- Fundus fluorescein angiography- To look for retinal ischemia, edema, leakages.
- Perimetry- If any optic nerve pathology is suspected.
- Ultrasound Biometry- For calculation of optical parameters such as axial length (AL), anterior chamber depth (ACD), and lens thickness (LT) which are required for intraocular lens (IOL) power calculation.
- Potential acuity meter and laser interferometer- To assess the visual potential.
Treatment / Management
The first step in managing patients with complicated cataracts involves arriving at an etiological diagnosis. Appropriate patient selection is important to identify those that will benefit from cataract surgery. Different forms of conditions have varied prognoses. Hence a proper diagnosis is the most important step. Since the majority of complicated cataracts develop secondary to uveitis, detailed management of uveitic cataracts is required.
Medical Management
The management should aim at the control of preoperative and postoperative Inflammation. The use of preoperative supplementary steroids reduces the risk of postoperative complications. The patient should be started on steroid treatment with topical drops, oral or periocular. The aim is to achieve adequate control of intraocular inflammation to avoid intraoperative and postoperative complications. To achieve a good visual prognosis postoperatively, the eyes at significant risk of complications should be identified, and appropriate management started. Eyes at risk of developing cystoid macular edema (CME) include chronic anterior uveitis secondary to sarcoidosis, eyes with earlier episodes of CME (e.g., intermediate uveitis).
In these situations, perioperative steroid prophylaxis should be given. Intraoperative steroids in the form of intravitreal preservative-free triamcinolone acetonide (4 mg in 0.1 ml) yield good control. The risk of recurrence of uveitis should be assessed in conditions such as Vogt-Koyanagi Harada disease, Behcet disease, and birdshot choroidopathy. In these situations, steroids can be given orally 1 mg per kg/day starting 3 days preoperatively, tapering according to the level of inflammation postoperatively. Topical prednisolone acetate 1% eye drops may also be used as well as periocular steroids. In eyes with infectious uveitis that tends to recur, such as ocular toxoplasmosis and herpes simplex uveitis, antimicrobial prophylaxis should be considered in the preoperative period. In these cases, oral acyclovir 400 mg twice daily or oral valacyclovir 0.5 mg four times daily should be started in the preoperative period and continued for 2 to 3 weeks postoperatively to prevent a recurrence.[8]
Surgical Management
- Indications for surgery in patients with uveitis include:
- Phacoantigenic uveitis (leakage of lens proteins leading to inflammation). Cataract removal is obligatory
- Visually significant cataract-the preoperative inflammation has to be controlled
- Dense cataracts that obscure the posterior segment visibility in cases of suspected posterior segment pathology
- Cataract that impedes adequate visualization of the posterior segment in cases where posterior segment surgery is indicated
- Timing of cataract surgery: For a successful surgical outcome, the eye needs to be quiet for at least 3 months prior to surgery. The disease should also be well-controlled in the postoperative period. This will curtail the risk of postoperative complications.
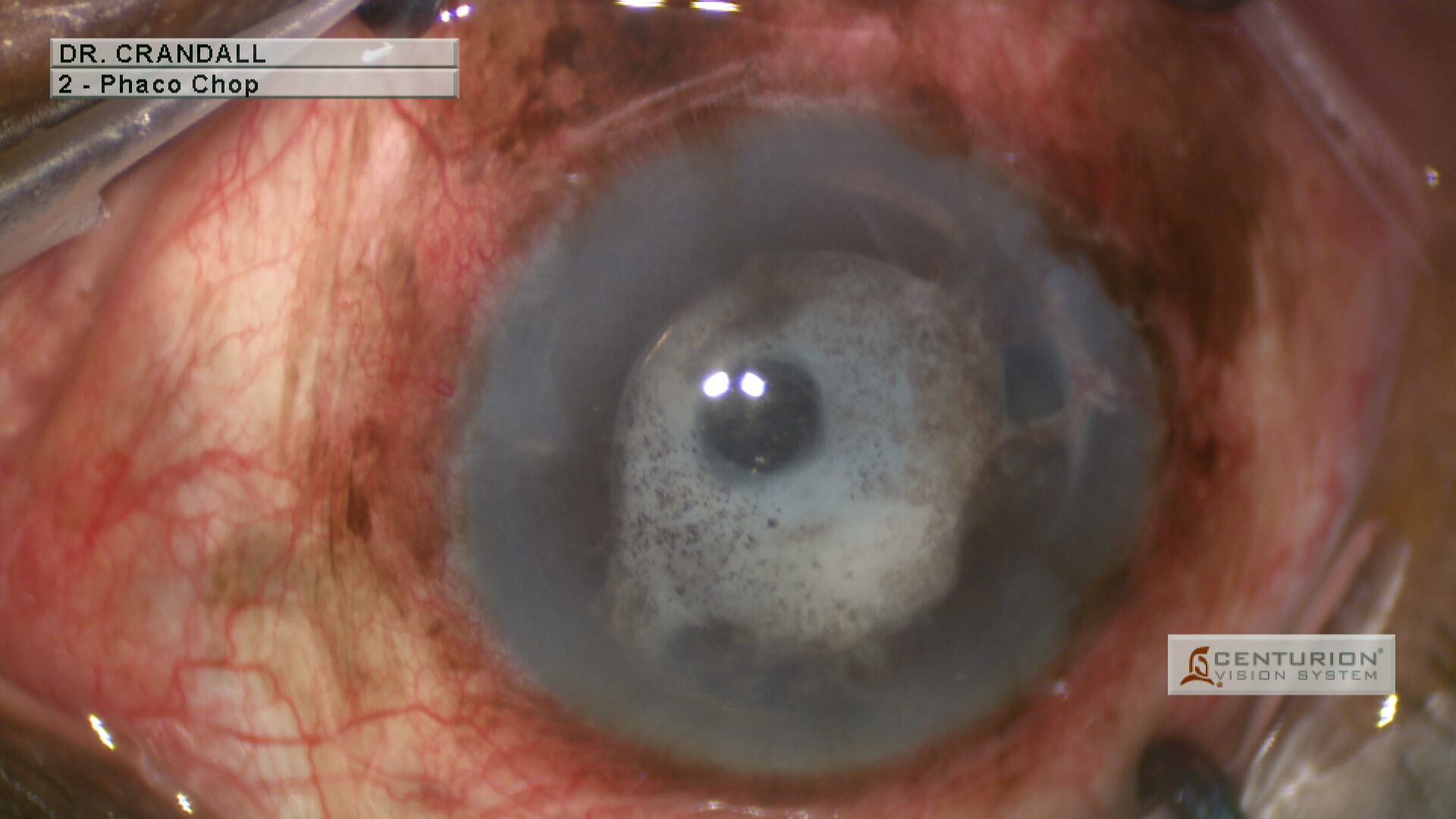
- Cataract surgery technique- Cataract extraction by phacoemulsification and in-the-bag Intraocular lens implantation is preferred for the uveitic cataract due to a reduced chance of inflammation. Phacoemulsification technique may vary depending upon the zonular status and the density of the cataract. An effort should be made to use less ultrasound power to prevent a posterior capsular tear. However, the surgical technique can be modified depending on the intraocular conditions. For eyes complicated by glaucoma, cataract surgery is not combined with trabeculectomy as the risk of bleb failure is high. Cataract extraction should be done first. When there are retinal complications such as epiretinal membranes or retinal detachment, cataract surgery can be combined with vitreoretinal surgery. In such cases, the decision for IOL implantation is to be taken by the surgeon.[9]
- Intraocular lens- Ideally, an in-the-bag IOL implantation should be performed. However, anterior chamber IOL, sulcus fixated IOL, and scleral-fixated IOL are other options. The most suitable IOL for in-the-bag implantation and the anterior chamber is an acrylic, single-piece, square-edged IOL. This reduces the rate of complications such as postoperative cystoid macular edema, posterior synechiae, pupillary membrane, posterior capsular opacification as compared to silicone IOL.
Surgical Challenges - The various challenges faced intraoperatively include inadequate visualization due to a small pupil, synechiae, pupillary membranes, and corneal opacification. There is a high risk of intraoperative complications such as posterior capsular rent, zonular dehiscence, anterior chamber hemorrhage, and pigment dispersion. The common challenges faced include-
- Small pupil- This situation can be tackled by using intracameral adrenaline diluted with a balanced salt solution. High molecular weight ophthalmic viscosurgical devices such as sodium hyaluronate 2.3% are also useful.
- Anterior or posterior synechiae - Peripheral anterior synechiae( PAS) should be managed before the posterior synechiae. PAS can be released by injecting high molecular weight viscoelastic, sweeping a 27 gauge cannula to separate the iris from the cornea and not detach the Descemet's membrane. For posterior synechiae, iris synechiolysis, pupillary membrane removal, use of iris hooks, and other pupil expansion devices should be implemented.
- Zonular dehiscence- Should be managed using capsular tension rings.
Differential Diagnosis
The complicated cataract being a secondary pathology, the differential diagnoses include disorders such as:
- Uveitis
- Glaucoma
- Retinal detachment
- Retinitis pigmentosa
- Optic atrophy
- Intraocular tumors
- Refractive errors
- Macular degenerations
Prognosis
Cataract extraction is expected to improve the visual outcome. However, the primary pathology also plays an important role in the final visual prognosis.
- In inflammatory conditions such as uveitis, the visual prognosis varies according to the different forms of uveitis and depends on the preoperative and postoperative control of inflammation. Fuchs’ heterochromic iridocyclitis has a good visual outcome and no significant postoperative inflammation. Juvenile idiopathic arthritis-associated uveitis has a guarded visual prognosis due to the high risk of postoperative inflammation. However, strict control of inflammation can achieve a satisfactory visual outcome. Cataract surgery in Behcet’s disease has a guarded prognosis due to intense inflammation and other complications such as optic atrophy, epiretinal membrane. Besides these autoimmune conditions, the infectious uveitis should be treated properly by appropriate antimicrobial prophylaxis as it has a high risk of recurrence, which will complicate the postoperative outcome.[10]
- In degenerative conditions, where a decrease in vision is mainly caused by visually significant cataracts rather than the pathology, cataract extraction with IOL implantation will improve the visual outcome. However, in the presence of significant macular damage, the visual prognosis is poor.
- In the presence of retinal detachment, glaucoma, and intraocular tumors, the visual prognosis is affected by the extent of intraocular damage by the primary pathology.
Complications
Intraoperative Complications
- Zonulolysis- Can occur in eyes with chronic uveitis. A capsular tension ring (CTR) is often necessary for conditions of significant zonular weakness to prevent IOL decentration.
- Phototoxic retinal damage
- Retained lens or nuclear fragments-Due to the compromised visibility, small nuclear fragments may be left in the eye, which later can cause severe inflammation. Hence, a careful extraction should be done.
- Posterior capsular rent- it can cause significant postoperative inflammation and should be managed carefully. An anterior vitrectomy should be performed. An IOL is implanted depending on the capsular status. If the rent is small, an in-the-bag IOL implantation is preferred. If the tear is large, but the capsular rim is intact, an IOL can be implanted in the ciliary sulcus, or an anterior chamber IOL implantation is performed. However, if there is no significant support for the IOL, a scleral fixated IOL can be implanted, or the patient may be left aphakic.[11]
Postoperative Complications
- Excessive postoperative inflammation- the patient should be started on topical steroids, eye drops, and topical non-steroidal anti-inflammatory eye drops in the immediate postoperative period. However, if the inflammation is not controlled, then oral steroids should be started.
- Intraocular Pressure (IOP) abnormalities- the intraocular pressure may be high or low. IOP may be raised in the early postoperative period due to compromised trabecular meshwork or angles. It can be managed with anti-glaucoma medications. The intraocular pressure may be low, which may be due to choroidal detachment or phthisis bulbi. Oral steroids should be prescribed.
- Recurrence of uveitis
- Posterior capsular opacification- usually occurs in the late postoperative period, should be treated after 3 months of cataract surgery by YAG laser capsulotomy.[12]
- Endophthalmitis
- Cystoid macular edema- It can occur as a complication preoperatively as well as postoperatively. It is one of the major contributors to blindness in uveitis. It occurs due to the breakdown of the inner or outer blood-retinal barrier induced by the inflammation. The mainstay of treatment of this condition is administering steroids in topical, oral, periocular, or intravitreal.[13]
Postoperative and Rehabilitation Care
Postoperative Management
The patient should be prescribed topical prednisolone acetate 1%, topical flurbiprofen, topical moxifloxacin or tobramycin, eye ointment atropine 1% in the immediate postoperative period to control inflammation. Intraocular pressure should be monitored digitally, and medication is given if required. If the patient was on oral corticosteroids or any antimicrobial prophylaxis, the maintenance dose should be continued. The drugs should be tapered gradually as the inflammation subsides. Oral corticosteroid is indicated for eyes with severe inflammation, mainly eyes with panuveitis ( Vogt-Koyanagi-Harada disease, Behcet disease), one-eyed patients. In pseudophakic patients, the accommodation for near vision is lost. Hence once the postoperative ocular condition is stabilized, refractive glasses for near vision should be prescribed to give a better vision to the patient.
Deterrence and Patient Education
A complicated cataract causes significant visual impairment in addition to the effects of the primary intraocular disease. This can affect the patient physically and mentally to a significant degree. Hence, the patient should be well motivated and educated about the nature of the condition, possible complications, benefits of timely treatment, and the need for long-term follow-up. In addition, careful counseling is needed in these patients as many patients will have been receiving treatment for a prolonged period already.
Enhancing Healthcare Team Outcomes
Patients with complicated cataracts usually present with the primary underlying disease. Therefore, meticulous and timely management of the primary intraocular condition is the most important task for an ophthalmologist. If the primary disease is managed properly, the chance of developing a complicated cataract is reduced. Hence, an interprofessional team approach is required, including the primary health care providers (physicians), specialists (ophthalmologists, rheumatologists, internal medicine specialists), and nursing staff.
The patient presenting with inflammatory intraocular diseases should be started on immediate treatment to control the inflammation. The systemic condition of the patient should also be monitored. The patient should be referred to a rheumatologist for appropriate immunosuppressives in case of uncontrolled inflammation, an Internal Medicine specialist for management of the patient, and the treatment's side effects. Similarly, patients with retinal conditions as a primary intraocular disease should be referred to a Retina specialist for management. Likewise, consultation with a glaucoma specialist is required in patients with glaucomatous damage.
Nursing staff and other professionals should educate the patient about the condition any complications. They should also motivate the patient to seek treatment. The ophthalmologists, along with their team, should provide comprehensive treatment to the patient. The patient should be referred to the appropriate specialist as and when required. If the patient develops a complicated cataract, timely cataract extraction with intraocular lens implantation should be done by an ophthalmic surgeon. Hence, an interprofessional team approach is important to diagnose the primary intraocular disease and provide timely treatment. However, if the patient develops a cataract, timely surgery should be done with appropriate precautions to ensure the best visual outcome for the patient. Also, postoperatively, the patient should be kept in follow-up to tackle the primary intraocular disease, monitor complications, and treat them when required. [Level 5]