[1]
Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nature reviews. Microbiology. 2021 Mar:19(3):141-154. doi: 10.1038/s41579-020-00459-7. Epub 2020 Oct 6
[PubMed PMID: 33024307]
[2]
Shang J, Ye G, Shi K, Wan Y, Luo C, Aihara H, Geng Q, Auerbach A, Li F. Structural basis of receptor recognition by SARS-CoV-2. Nature. 2020 May:581(7807):221-224. doi: 10.1038/s41586-020-2179-y. Epub 2020 Mar 30
[PubMed PMID: 32225175]
[3]
Wang Q, Zhang Y, Wu L, Niu S, Song C, Zhang Z, Lu G, Qiao C, Hu Y, Yuen KY, Wang Q, Zhou H, Yan J, Qi J. Structural and Functional Basis of SARS-CoV-2 Entry by Using Human ACE2. Cell. 2020 May 14:181(4):894-904.e9. doi: 10.1016/j.cell.2020.03.045. Epub 2020 Apr 9
[PubMed PMID: 32275855]
Level 2 (mid-level) evidence
[4]
Hue S, Beldi-Ferchiou A, Bendib I, Surenaud M, Fourati S, Frapard T, Rivoal S, Razazi K, Carteaux G, Delfau-Larue MH, Mekontso-Dessap A, Audureau E, de Prost N. Uncontrolled Innate and Impaired Adaptive Immune Responses in Patients with COVID-19 Acute Respiratory Distress Syndrome. American journal of respiratory and critical care medicine. 2020 Dec 1:202(11):1509-1519. doi: 10.1164/rccm.202005-1885OC. Epub
[PubMed PMID: 32866033]
[5]
Wichmann D, Sperhake JP, Lütgehetmann M, Steurer S, Edler C, Heinemann A, Heinrich F, Mushumba H, Kniep I, Schröder AS, Burdelski C, de Heer G, Nierhaus A, Frings D, Pfefferle S, Becker H, Bredereke-Wiedling H, de Weerth A, Paschen HR, Sheikhzadeh-Eggers S, Stang A, Schmiedel S, Bokemeyer C, Addo MM, Aepfelbacher M, Püschel K, Kluge S. Autopsy Findings and Venous Thromboembolism in Patients With COVID-19: A Prospective Cohort Study. Annals of internal medicine. 2020 Aug 18:173(4):268-277. doi: 10.7326/M20-2003. Epub 2020 May 6
[PubMed PMID: 32374815]
[6]
Ojo AS, Balogun SA, Williams OT, Ojo OS. Pulmonary Fibrosis in COVID-19 Survivors: Predictive Factors and Risk Reduction Strategies. Pulmonary medicine. 2020:2020():6175964. doi: 10.1155/2020/6175964. Epub 2020 Aug 10
[PubMed PMID: 32850151]
[7]
Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, Chiumello D. COVID-19 Does Not Lead to a "Typical" Acute Respiratory Distress Syndrome. American journal of respiratory and critical care medicine. 2020 May 15:201(10):1299-1300. doi: 10.1164/rccm.202003-0817LE. Epub
[PubMed PMID: 32228035]
[8]
Haudebourg AF,Perier F,Tuffet S,de Prost N,Razazi K,Mekontso Dessap A,Carteaux G, Respiratory Mechanics of COVID-19- versus Non-COVID-19-associated Acute Respiratory Distress Syndrome. American journal of respiratory and critical care medicine. 2020 Jul 15;
[PubMed PMID: 32479162]
[9]
Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, Prat G, Boulain T, Morawiec E, Cottereau A, Devaquet J, Nseir S, Razazi K, Mira JP, Argaud L, Chakarian JC, Ricard JD, Wittebole X, Chevalier S, Herbland A, Fartoukh M, Constantin JM, Tonnelier JM, Pierrot M, Mathonnet A, Béduneau G, Delétage-Métreau C, Richard JC, Brochard L, Robert R, FLORALI Study Group, REVA Network. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. The New England journal of medicine. 2015 Jun 4:372(23):2185-96. doi: 10.1056/NEJMoa1503326. Epub 2015 May 17
[PubMed PMID: 25981908]
[10]
Rochwerg B, Granton D, Wang DX, Helviz Y, Einav S, Frat JP, Mekontso-Dessap A, Schreiber A, Azoulay E, Mercat A, Demoule A, Lemiale V, Pesenti A, Riviello ED, Mauri T, Mancebo J, Brochard L, Burns K. High flow nasal cannula compared with conventional oxygen therapy for acute hypoxemic respiratory failure: a systematic review and meta-analysis. Intensive care medicine. 2019 May:45(5):563-572. doi: 10.1007/s00134-019-05590-5. Epub 2019 Mar 19
[PubMed PMID: 30888444]
Level 1 (high-level) evidence
[11]
Yoshida T, Uchiyama A, Fujino Y. The role of spontaneous effort during mechanical ventilation: normal lung versus injured lung. Journal of intensive care. 2015:3():18. doi: 10.1186/s40560-015-0083-6. Epub 2015 Jun 17
[PubMed PMID: 27408729]
[12]
Roca O,Messika J,Caralt B,García-de-Acilu M,Sztrymf B,Ricard JD,Masclans JR, Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index. Journal of critical care. 2016 Oct;
[PubMed PMID: 27481760]
[13]
Grieco DL, Menga LS, Cesarano M, Rosà T, Spadaro S, Bitondo MM, Montomoli J, Falò G, Tonetti T, Cutuli SL, Pintaudi G, Tanzarella ES, Piervincenzi E, Bongiovanni F, Dell'Anna AM, Delle Cese L, Berardi C, Carelli S, Bocci MG, Montini L, Bello G, Natalini D, De Pascale G, Velardo M, Volta CA, Ranieri VM, Conti G, Maggiore SM, Antonelli M, COVID-ICU Gemelli Study Group. Effect of Helmet Noninvasive Ventilation vs High-Flow Nasal Oxygen on Days Free of Respiratory Support in Patients With COVID-19 and Moderate to Severe Hypoxemic Respiratory Failure: The HENIVOT Randomized Clinical Trial. JAMA. 2021 May 4:325(17):1731-1743. doi: 10.1001/jama.2021.4682. Epub
[PubMed PMID: 33764378]
Level 1 (high-level) evidence
[14]
Bellani G, Laffey JG, Pham T, Madotto F, Fan E, Brochard L, Esteban A, Gattinoni L, Bumbasirevic V, Piquilloud L, van Haren F, Larsson A, McAuley DF, Bauer PR, Arabi YM, Ranieri M, Antonelli M, Rubenfeld GD, Thompson BT, Wrigge H, Slutsky AS, Pesenti A, LUNG SAFE Investigators, ESICM Trials Group. Noninvasive Ventilation of Patients with Acute Respiratory Distress Syndrome. Insights from the LUNG SAFE Study. American journal of respiratory and critical care medicine. 2017 Jan 1:195(1):67-77. doi: 10.1164/rccm.201606-1306OC. Epub
[PubMed PMID: 27753501]
[15]
Duan J, Han X, Bai L, Zhou L, Huang S. Assessment of heart rate, acidosis, consciousness, oxygenation, and respiratory rate to predict noninvasive ventilation failure in hypoxemic patients. Intensive care medicine. 2017 Feb:43(2):192-199. doi: 10.1007/s00134-016-4601-3. Epub 2016 Nov 3
[PubMed PMID: 27812731]
[16]
Perkins GD, Couper K, Connolly B, Baillie JK, Bradley JM, Dark P, De Soyza A, Gorman E, Gray A, Hamilton L, Hart N, Ji C, Lall R, McGowan N, Regan S, Simonds AK, Skilton E, Stallard N, Stimpson E, Yeung J, McAuley DF. RECOVERY- Respiratory Support: Respiratory Strategies for patients with suspected or proven COVID-19 respiratory failure; Continuous Positive Airway Pressure, High-flow Nasal Oxygen, and standard care: A structured summary of a study protocol for a randomised controlled trial. Trials. 2020 Jul 29:21(1):687. doi: 10.1186/s13063-020-04617-3. Epub 2020 Jul 29
[PubMed PMID: 32727624]
Level 1 (high-level) evidence
[17]
Munshi L, Walkey A, Goligher E, Pham T, Uleryk EM, Fan E. Venovenous extracorporeal membrane oxygenation for acute respiratory distress syndrome: a systematic review and meta-analysis. The Lancet. Respiratory medicine. 2019 Feb:7(2):163-172. doi: 10.1016/S2213-2600(18)30452-1. Epub 2019 Jan 11
[PubMed PMID: 30642776]
Level 1 (high-level) evidence
[18]
Zapol WM, Snider MT, Hill JD, Fallat RJ, Bartlett RH, Edmunds LH, Morris AH, Peirce EC 2nd, Thomas AN, Proctor HJ, Drinker PA, Pratt PC, Bagniewski A, Miller RG Jr. Extracorporeal membrane oxygenation in severe acute respiratory failure. A randomized prospective study. JAMA. 1979 Nov 16:242(20):2193-6
[PubMed PMID: 490805]
Level 1 (high-level) evidence
[19]
Brodie D, The Evolution of Extracorporeal Membrane Oxygenation for Adult Respiratory Failure. Annals of the American Thoracic Society. 2018 Feb;
[PubMed PMID: 29461889]
[20]
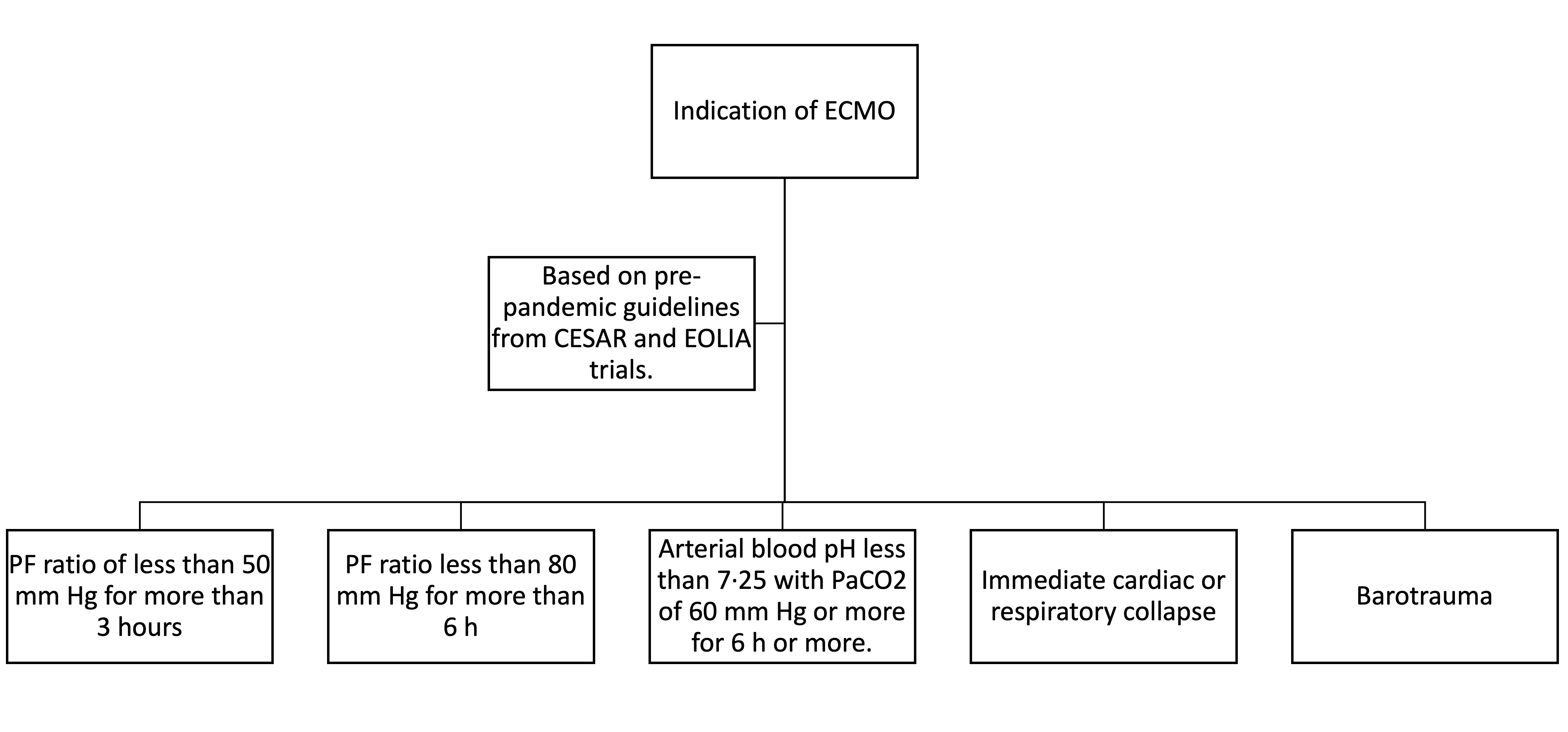
Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM, Hibbert CL, Truesdale A, Clemens F, Cooper N, Firmin RK, Elbourne D, CESAR trial collaboration. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet (London, England). 2009 Oct 17:374(9698):1351-63. doi: 10.1016/S0140-6736(09)61069-2. Epub 2009 Sep 15
[PubMed PMID: 19762075]
Level 1 (high-level) evidence
[21]
Harrington D, Drazen JM. Learning from a Trial Stopped by a Data and Safety Monitoring Board. The New England journal of medicine. 2018 May 24:378(21):2031-2032. doi: 10.1056/NEJMe1805123. Epub
[PubMed PMID: 29791830]
[22]
Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, Bellani G, Bonanomi E, Cabrini L, Carlesso E, Castelli G, Cattaneo S, Cereda D, Colombo S, Coluccello A, Crescini G, Forastieri Molinari A, Foti G, Fumagalli R, Iotti GA, Langer T, Latronico N, Lorini FL, Mojoli F, Natalini G, Pessina CM, Ranieri VM, Rech R, Scudeller L, Rosano A, Storti E, Thompson BT, Tirani M, Villani PG, Pesenti A, Cecconi M, COVID-19 Lombardy ICU Network. Risk Factors Associated With Mortality Among Patients With COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA internal medicine. 2020 Oct 1:180(10):1345-1355. doi: 10.1001/jamainternmed.2020.3539. Epub
[PubMed PMID: 32667669]
[23]
Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, Oczkowski S, Levy MM, Derde L, Dzierba A, Du B, Aboodi M, Wunsch H, Cecconi M, Koh Y, Chertow DS, Maitland K, Alshamsi F, Belley-Cote E, Greco M, Laundy M, Morgan JS, Kesecioglu J, McGeer A, Mermel L, Mammen MJ, Alexander PE, Arrington A, Centofanti JE, Citerio G, Baw B, Memish ZA, Hammond N, Hayden FG, Evans L, Rhodes A. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive care medicine. 2020 May:46(5):854-887. doi: 10.1007/s00134-020-06022-5. Epub 2020 Mar 28
[PubMed PMID: 32222812]
[24]
Bartlett RH, Ogino MT, Brodie D, McMullan DM, Lorusso R, MacLaren G, Stead CM, Rycus P, Fraser JF, Belohlavek J, Salazar L, Mehta Y, Raman L, Paden ML. Initial ELSO Guidance Document: ECMO for COVID-19 Patients with Severe Cardiopulmonary Failure. ASAIO journal (American Society for Artificial Internal Organs : 1992). 2020 May:66(5):472-474. doi: 10.1097/MAT.0000000000001173. Epub
[PubMed PMID: 32243267]
[25]
Ritter M, Ott DVM, Paul F, Haynes JD, Ritter K. COVID-19: a simple statistical model for predicting intensive care unit load in exponential phases of the disease. Scientific reports. 2021 Mar 3:11(1):5018. doi: 10.1038/s41598-021-83853-2. Epub 2021 Mar 3
[PubMed PMID: 33658593]
[26]
Rubinson L, Intensive Care Unit Strain and Mortality Risk Among Critically Ill Patients With COVID-19-There Is No
[PubMed PMID: 33464314]
[27]
Zeidan A, Bamadhaj M, Al-Faraidy M, Ali M. Videolaryngoscopy Intubation in Patients with COVID-19: How to Minimize Risk of Aerosolization? Anesthesiology. 2020 Aug:133(2):481-483. doi: 10.1097/ALN.0000000000003389. Epub
[PubMed PMID: 32427641]
[28]
Foley LJ, Urdaneta F, Berkow L, Aziz MF, Baker PA, Jagannathan N, Rosenblatt W, Straker TM, Wong DT, Hagberg CA. Difficult Airway Management in Adult Coronavirus Disease 2019 Patients: Statement by the Society of Airway Management. Anesthesia and analgesia. 2021 Oct 1:133(4):876-890. doi: 10.1213/ANE.0000000000005554. Epub
[PubMed PMID: 33711004]
[29]
Berlin DA, Gulick RM, Martinez FJ. Severe Covid-19. The New England journal of medicine. 2020 Dec 17:383(25):2451-2460. doi: 10.1056/NEJMcp2009575. Epub 2020 May 15
[PubMed PMID: 32412710]
[30]
Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The New England journal of medicine. 2000 May 4:342(18):1301-8
[PubMed PMID: 10793162]
[31]
Kacmarek RM, Villar J, Sulemanji D, Montiel R, Ferrando C, Blanco J, Koh Y, Soler JA, Martínez D, Hernández M, Tucci M, Borges JB, Lubillo S, Santos A, Araujo JB, Amato MB, Suárez-Sipmann F, Open Lung Approach Network. Open Lung Approach for the Acute Respiratory Distress Syndrome: A Pilot, Randomized Controlled Trial. Critical care medicine. 2016 Jan:44(1):32-42. doi: 10.1097/CCM.0000000000001383. Epub
[PubMed PMID: 26672923]
Level 3 (low-level) evidence
[32]
Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, Stewart TE, Briel M, Talmor D, Mercat A, Richard JC, Carvalho CR, Brower RG. Driving pressure and survival in the acute respiratory distress syndrome. The New England journal of medicine. 2015 Feb 19:372(8):747-55. doi: 10.1056/NEJMsa1410639. Epub
[PubMed PMID: 25693014]
[33]
Aggarwal NR, Brower RG. Targeting normoxemia in acute respiratory distress syndrome may cause worse short-term outcomes because of oxygen toxicity. Annals of the American Thoracic Society. 2014 Nov:11(9):1449-53. doi: 10.1513/AnnalsATS.201407-297PS. Epub
[PubMed PMID: 25314313]
[34]
Douglas WW, Rehder K, Beynen FM, Sessler AD, Marsh HM. Improved oxygenation in patients with acute respiratory failure: the prone position. The American review of respiratory disease. 1977 Apr:115(4):559-66
[PubMed PMID: 322557]
[35]
Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, Mercier E, Badet M, Mercat A, Baudin O, Clavel M, Chatellier D, Jaber S, Rosselli S, Mancebo J, Sirodot M, Hilbert G, Bengler C, Richecoeur J, Gainnier M, Bayle F, Bourdin G, Leray V, Girard R, Baboi L, Ayzac L, PROSEVA Study Group. Prone positioning in severe acute respiratory distress syndrome. The New England journal of medicine. 2013 Jun 6:368(23):2159-68. doi: 10.1056/NEJMoa1214103. Epub 2013 May 20
[PubMed PMID: 23688302]
[36]
Shelhamer MC, Wesson PD, Solari IL, Jensen DL, Steele WA, Dimitrov VG, Kelly JD, Aziz S, Gutierrez VP, Vittinghoff E, Chung KK, Menon VP, Ambris HA, Baxi SM. Prone Positioning in Moderate to Severe Acute Respiratory Distress Syndrome Due to COVID-19: A Cohort Study and Analysis of Physiology. Journal of intensive care medicine. 2021 Feb:36(2):241-252. doi: 10.1177/0885066620980399. Epub
[PubMed PMID: 33380236]
[37]
Gainnier M, Roch A, Forel JM, Thirion X, Arnal JM, Donati S, Papazian L. Effect of neuromuscular blocking agents on gas exchange in patients presenting with acute respiratory distress syndrome. Critical care medicine. 2004 Jan:32(1):113-9
[PubMed PMID: 14707568]
[38]
Forel JM, Roch A, Marin V, Michelet P, Demory D, Blache JL, Perrin G, Gainnier M, Bongrand P, Papazian L. Neuromuscular blocking agents decrease inflammatory response in patients presenting with acute respiratory distress syndrome. Critical care medicine. 2006 Nov:34(11):2749-57
[PubMed PMID: 16932229]
[39]
Papazian L, Forel JM, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, Jaber S, Arnal JM, Perez D, Seghboyan JM, Constantin JM, Courant P, Lefrant JY, Guérin C, Prat G, Morange S, Roch A, ACURASYS Study Investigators. Neuromuscular blockers in early acute respiratory distress syndrome. The New England journal of medicine. 2010 Sep 16:363(12):1107-16. doi: 10.1056/NEJMoa1005372. Epub
[PubMed PMID: 20843245]
[40]
National Heart, Lung, and Blood Institute PETAL Clinical Trials Network, Moss M, Huang DT, Brower RG, Ferguson ND, Ginde AA, Gong MN, Grissom CK, Gundel S, Hayden D, Hite RD, Hou PC, Hough CL, Iwashyna TJ, Khan A, Liu KD, Talmor D, Thompson BT, Ulysse CA, Yealy DM, Angus DC. Early Neuromuscular Blockade in the Acute Respiratory Distress Syndrome. The New England journal of medicine. 2019 May 23:380(21):1997-2008. doi: 10.1056/NEJMoa1901686. Epub 2019 May 19
[PubMed PMID: 31112383]
[41]
Kuhl T, Michels G, Pfister R, Wendt S, Langebartels G, Wahlers T. Comparison of the Avalon Dual-Lumen Cannula with Conventional Cannulation Technique for Venovenous Extracorporeal Membrane Oxygenation. The Thoracic and cardiovascular surgeon. 2015 Dec:63(8):653-62. doi: 10.1055/s-0035-1549359. Epub 2015 May 6
[PubMed PMID: 25959306]
[42]
Mustafa AK, Alexander PJ, Joshi DJ, Tabachnick DR, Cross CA, Pappas PS, Tatooles AJ. Extracorporeal Membrane Oxygenation for Patients With COVID-19 in Severe Respiratory Failure. JAMA surgery. 2020 Oct 1:155(10):990-992. doi: 10.1001/jamasurg.2020.3950. Epub
[PubMed PMID: 32780089]
[43]
Schmidt M, Tachon G, Devilliers C, Muller G, Hekimian G, Bréchot N, Merceron S, Luyt CE, Trouillet JL, Chastre J, Leprince P, Combes A. Blood oxygenation and decarboxylation determinants during venovenous ECMO for respiratory failure in adults. Intensive care medicine. 2013 May:39(5):838-46. doi: 10.1007/s00134-012-2785-8. Epub 2013 Jan 5
[PubMed PMID: 23291732]
[44]
Abrams D, Schmidt M, Pham T, Beitler JR, Fan E, Goligher EC, McNamee JJ, Patroniti N, Wilcox ME, Combes A, Ferguson ND, McAuley DF, Pesenti A, Quintel M, Fraser J, Hodgson CL, Hough CL, Mercat A, Mueller T, Pellegrino V, Ranieri VM, Rowan K, Shekar K, Brochard L, Brodie D. Mechanical Ventilation for Acute Respiratory Distress Syndrome during Extracorporeal Life Support. Research and Practice. American journal of respiratory and critical care medicine. 2020 Mar 1:201(5):514-525. doi: 10.1164/rccm.201907-1283CI. Epub
[PubMed PMID: 31726013]
[45]
Aoyama H, Pettenuzzo T, Aoyama K, Pinto R, Englesakis M, Fan E. Association of Driving Pressure With Mortality Among Ventilated Patients With Acute Respiratory Distress Syndrome: A Systematic Review and Meta-Analysis. Critical care medicine. 2018 Feb:46(2):300-306. doi: 10.1097/CCM.0000000000002838. Epub
[PubMed PMID: 29135500]
Level 1 (high-level) evidence
[46]
Tonetti T, Vasques F, Rapetti F, Maiolo G, Collino F, Romitti F, Camporota L, Cressoni M, Cadringher P, Quintel M, Gattinoni L. Driving pressure and mechanical power: new targets for VILI prevention. Annals of translational medicine. 2017 Jul:5(14):286. doi: 10.21037/atm.2017.07.08. Epub
[PubMed PMID: 28828361]
[47]
Schmidt M, Hajage D, Lebreton G, Monsel A, Voiriot G, Levy D, Baron E, Beurton A, Chommeloux J, Meng P, Nemlaghi S, Bay P, Leprince P, Demoule A, Guidet B, Constantin JM, Fartoukh M, Dres M, Combes A, Groupe de Recherche Clinique en REanimation et Soins intensifs du Patient en Insuffisance Respiratoire aiguE (GRC-RESPIRE) Sorbonne Université, Paris-Sorbonne ECMO-COVID investigators. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: a retrospective cohort study. The Lancet. Respiratory medicine. 2020 Nov:8(11):1121-1131. doi: 10.1016/S2213-2600(20)30328-3. Epub 2020 Aug 13
[PubMed PMID: 32798468]
Level 2 (mid-level) evidence
[48]
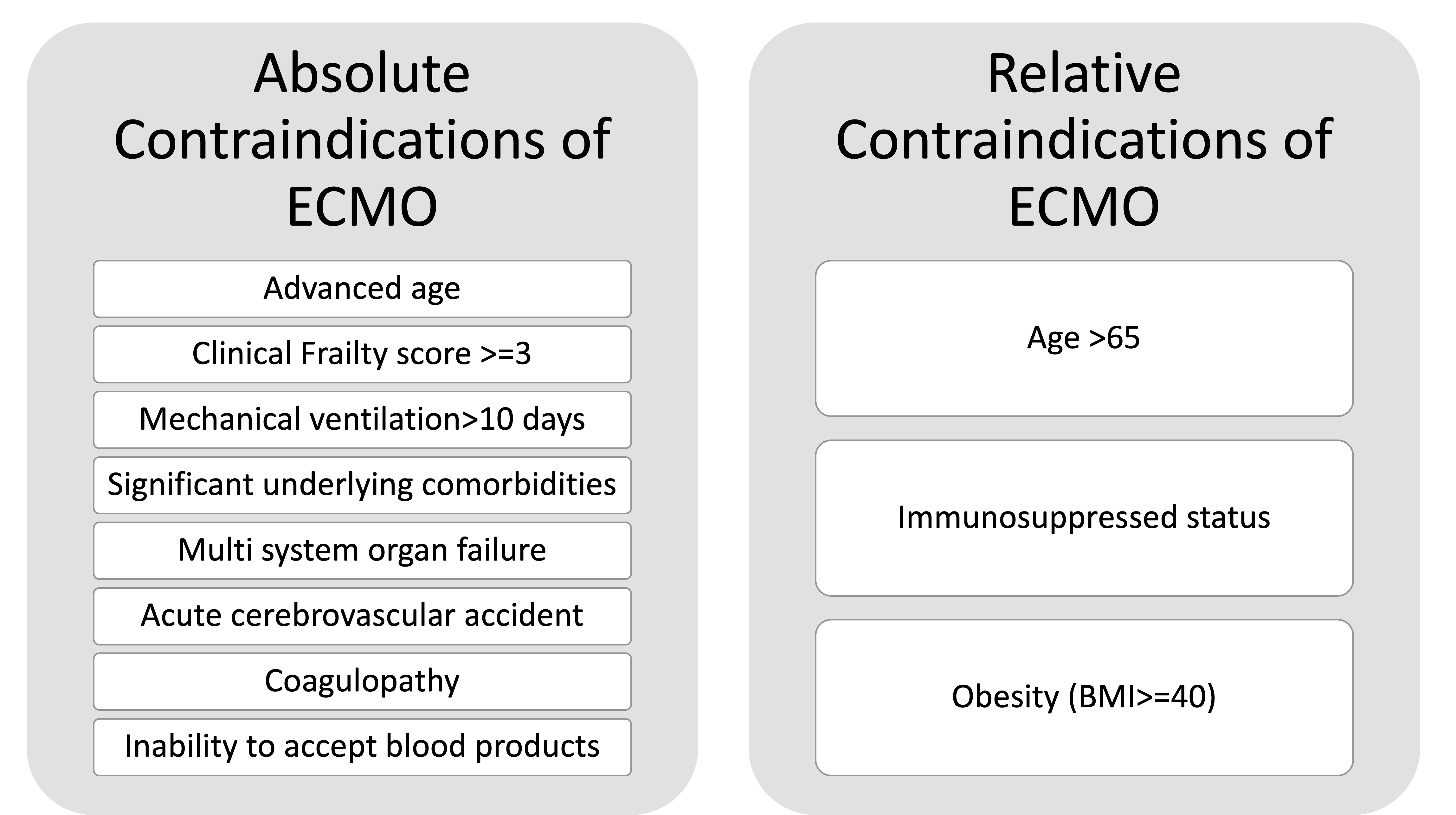
Makdisi T, Makdisi G. Ethical challenges in extra corporeal membrane oxygenation use. Annals of palliative medicine. 2017 Dec:6(Suppl 2):S128-S131. doi: 10.21037/apm.2017.03.11. Epub 2017 May 5
[PubMed PMID: 28595436]
[49]
Mazzeffi M, Greenwood J, Tanaka K, Menaker J, Rector R, Herr D, Kon Z, Lee J, Griffith B, Rajagopal K, Pham S. Bleeding, Transfusion, and Mortality on Extracorporeal Life Support: ECLS Working Group on Thrombosis and Hemostasis. The Annals of thoracic surgery. 2016 Feb:101(2):682-9. doi: 10.1016/j.athoracsur.2015.07.046. Epub 2015 Oct 9
[PubMed PMID: 26443879]
[50]
Khan I, Rehan M, Parikh G, Zammit C, Badjatia N, Herr D, Kon Z, Hogue C, Mazzeffi M. Regional Cerebral Oximetry as an Indicator of Acute Brain Injury in Adults Undergoing Veno-Arterial Extracorporeal Membrane Oxygenation-A Prospective Pilot Study. Frontiers in neurology. 2018:9():993. doi: 10.3389/fneur.2018.00993. Epub 2018 Nov 23
[PubMed PMID: 30532730]
Level 3 (low-level) evidence
[51]
Anderson BR, Ivascu NS, Brodie D, Weingarten JA, Manoach SM, Smith AJ, Millerman K, Yip NH, Su G, Kleinschmidt C, Khusid F, Olson M, Hochman BR, Hill LL, Burkart KM. Breaking Silos: The Team-Based Approach to Coronavirus Disease 2019 Pandemic Staffing. Critical care explorations. 2020 Nov:2(11):e0265. doi: 10.1097/CCE.0000000000000265. Epub 2020 Nov 3
[PubMed PMID: 33163970]
[52]
Tang L, Zhao XM, Yu XY. Team management in critical care units for patients with COVID-19: an experience from Hunan Province, China. Critical care (London, England). 2020 Jun 6:24(1):304. doi: 10.1186/s13054-020-02921-7. Epub 2020 Jun 6
[PubMed PMID: 32505189]
[53]
Gabarre P, Dumas G, Dupont T, Darmon M, Azoulay E, Zafrani L. Acute kidney injury in critically ill patients with COVID-19. Intensive care medicine. 2020 Jul:46(7):1339-1348. doi: 10.1007/s00134-020-06153-9. Epub 2020 Jun 12
[PubMed PMID: 32533197]
[54]
Aslakson RA, Curtis JR, Nelson JE. The changing role of palliative care in the ICU. Critical care medicine. 2014 Nov:42(11):2418-28. doi: 10.1097/CCM.0000000000000573. Epub
[PubMed PMID: 25167087]