Continuing Education Activity
PET/CT (positron emission tomography) is a widely utilized nuclear medicine imaging modality used to evaluate the staging, treatment response, or recurrence of various cancers. While mammography remains the first-line imaging exam used in detecting and screening cancer, currently used secondary imaging modalities include ultrasound, MRI, and in special instances, PET/CT. This activity reviews the use of PET/CT as an adjunctive imaging modality used in the evaluation of patients with breast cancer. Furthermore, this activity highlights the indications, imaging technique, patient preparation, and the use of PET/CT by the interprofessional team in the setting of breast cancer.
Objectives:
- Describe the indications of PET/CT in its use in breast cancer.
- Explain the technique involved in PET/CT acquisition.
- Summarize the clinical value of 18F-FDG PET/CT in breast cancer.
- Outline some interprofessional strategies that can improve patient results when using 18F-FDG PET/CT in breast cancer cases.
Introduction
PET/CT (positron emission tomography) is a widely utilized nuclear medicine imaging modality in which fluorodeoxyglucose (FDG) follows glucose uptake into highly metabolic tissues, most commonly used in the evaluation of staging, treatment response, or recurrence of various cancers. While mammography remains the first-line imaging exam used in detecting and screening breast cancer, currently used secondary imaging modalities include ultrasound, MRI, and in special instances, PET/CT. Fluency in the anatomy and pathophysiology of breast tissue is crucial in the interpretation of breast imaging. This activity reviews the use of PET/CT in the setting of breast cancer staging and recurrence, breast anatomy, and pathophysiology.
Anatomy and Physiology
Given the wide range in appearance of the breast from patient to patient, it’s crucial in breast imaging interpretation to understand breast anatomy and pathophysiology. The human breasts develop under the influence of hormones on ectodermal cells. Female breast stroma primarily consisting of fat, fibroglandular stroma, ducts, and lobules. With the onset of puberty, ductal and stromal growth is dependent on the proliferative effects of estrogen. Thus in the male breast, the antagonistic effects androgens demonstrated on ductal and stromal growth result in a predominantly fatty breast. The volume of fibroglandular tissue varies tremendously from patient to patient and throughout an individual's life. In pregnancy, lobular tissue within the breast parenchyma reaches functional maturity with ductal proliferation and adipose tissue decrease.[1]
Breast fibroglandular tissue demonstrates variable FDG uptake and is often secondary to hormonal influences on breast vascularity, thus changing significantly throughout life, often becoming minimal in the post-menopausal state. FDG uptake is typically mild in normal breast tissue and marked in the lactating breast. The abundant lymphatic system of the breast begins within the mammary ducts. Deep lymphatic channels, including the subareolar plexus, primarily drain to axillary and internal mammary lymph nodes, which are the two most important nodal sites to evaluate nodal radiotracer uptake on PET scans.
Indications
Currently, FDG PET/CT does not have a role in screening for breast cancer. Studies have found FDG PET/CT to be most clinically useful in staging recurrent or metastatic breast cancer in addition to the evaluation of the response of locally advanced breast cancer during neoadjuvant and post-treatment. Currently, FDG is the main radiotracer utilized in clinical practice though studies have found 18F-Fluoroestradiol to be used in imaging estrogen receptor expression.[2] The clinical indications for FDG PET/CT in patients with breast cancer routinely reimbursed by Centers for Medicare and Medicaid services include locoregional staging, axillary nodal disease in high-risk patients, internal mammary nodal status, systemic staging, and in the evaluation for skeletal metastatic involvement.[3]
PET/CT for staging replaces CT of the chest, abdomen, and pelvis plus bone scan to assess metastatic disease and is indicated per NCCN guidelines. Given the sensitivity of PET to be superior to that of CT in the detection of nodal disease, it may be beneficial in the staging and restaging of locally recurrent disease. Further, in known breast cancer patients with rising tumor marker levels, FDG PET allows a more accurate diagnosis of metastatic disease when compared to conventional imaging, with PET/CT having a sensitivity of 90%.[4]
Contraindications
- There are no absolute contraindications to PET/CT; however, risks versus benefits should be considered in pregnant patients.
- Patient obesity may be a factor for scanner weight limits, require a higher dose of FDG, and reduce image quality and interpretation.
- Patients with diabetes will need blood sugar control to levels below 200 mg/dL to prevent glucose competition with FDG for cellular uptake.
- Patients with iodine allergy may require premedication for prophylaxis only if iodinated contrast is used for the CT portion.
Equipment
PET/CT is performed in a specialized scanner within an imaging facility or within a mobile unit. IV access is required to inject FDG.
Personnel
Specialized radiology technologists perform the PET/CT. Post-processing and interpretation are performed by a physician radiologist or nuclear medicine specialist.
Preparation
The pathophysiology of FDG as a glucose analog used in PET imaging makes patient preparation crucial in the image acquisition process as the distribution of FDG largely follows the physiologic metabolism of glucose. Glucose and insulin, especially in excess states, act as competitive inhibitors of FDG. Patients are directed to fast for a minimum of 4 to 6 hours before FDG injection to decrease baseline insulin levels. In doing this, the highest target to background ratio images are acquired.[5]
Blood glucose levels should be below 150-200 mg/dl to also decrease competitive inhibition. In insulin-dependent patients, administering fast-acting insulin close to FDG injection time will reduce tumor uptake and encourage physiologic uptake in adipose and muscle, which would decrease the overall tumor to background ratio. Increased physiologic uptake is still seen despite fasting in high glycolytic organs such as the myocardium and brain. Low-level homogenous uptake is typically seen in organs, including the liver, spleen, and bone marrow. Proper patient preparation, including adequate documentation of patient history and current medications, allows for proper imaging acquisition and interpretation.[6]
Technique or Treatment
Glucose metabolism plays a key role as the primary source of energy for humans. Its dysregulation is associated with cancer, resulting in the loss of control of proliferation, invasion, and metastasis. Fluorodeoxyglucose (FDG) is a radiolabeled glucose analog used in positron emission tomography (PET) imaging. 2-deoxy-2-[18F]fluoro-glucose (18F-FDG) based positron emission/computed tomography (PET/CT) is known as the most popular glucose-based radiopharmaceutical in molecular imaging. It is the only glucose-based radiopharmaceutical that has been approved by the Food and Drug Administration worldwide.[7]
Nuclear medicine imaging is defined by the visualization, characterization, and biological process measurements at the molecular level. Medical imaging with PET utilizes short-lived isotopes which emit positrons in a process known as beta plus decay.[5] The basis of image production is centered around two gamma photons traveling in opposite directions from one another at 180degrees produced when a positron collides with an electron.
The basic concept used in FDG imaging is that tumor cells consume more glucose than other tissues because of the increased intracellular glycolysis, also known as the Warburg effect. Despite the chemical and structural differences between FDG and glucose, FDG is processed in human cells identical to glucose. FDG enters the cell via facilitated transport mediated by the glucose transporters known as GLUTs. The most common GLUT transporter in humans is GLUT1 which is also most commonly overexpressed in cancers. Further, it has been found that GLUT1 overexpression correlates with tumor development and, thus, a more unfavorable prognosis.[5]
After FDG has entered the cell, it is phosphorylated to form FDG-6-Phosphate, which, unlike glucose, can only exit the cell if it is dephosphorylated by glucose-6-phosphatase. Tumor cells express reduced levels of glucose-6-phosphatase, which subsequently leads to the accumulation of FDG-phosphate in cancer cells. Like tumor cells, cells with high glucose turnover such as sites of infection can also accumulate FDG, thus making increased radiotracer uptake not specific for cancer.
Although cancer cells are known to consume more glucose, several factors influence radiotracer uptake that is important to keep in mind when evaluating PET imaging. Tumors without adequate vascularization will result in insufficient delivery of glucose and oxygen and thus tumor hypoxia. Areas of hypoxic and occasionally infarcted tissue appear as tumor necrosis and are often associated with increased malignancy and a poor prognosis.
The uptake of FDG on imaging is measured as the standardized uptake value (SUV), and if properly corrected, PET images are quantitative. This means each radioactivity value in each voxel correlates with the concentration of absolute radioactivity in vivo. Studies have shown a positive correlation between the standardized uptake value of a tumor with its GLUT1 expression.
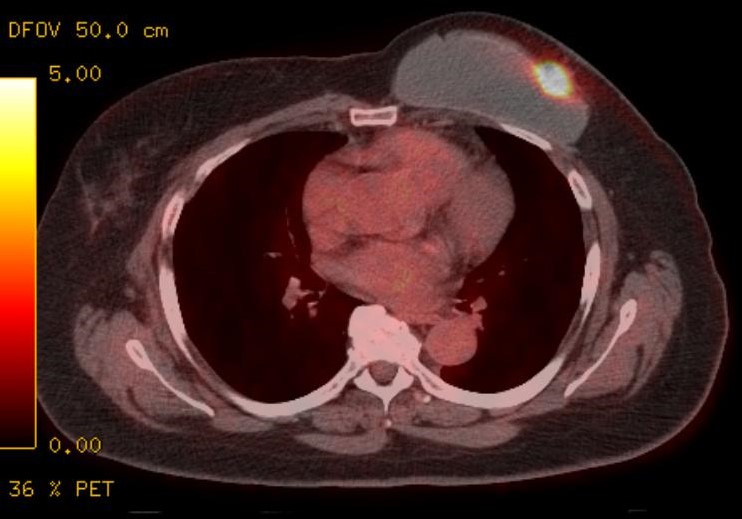
PET/CT images are viewed and interpreted using specialized software to evaluate abnormal areas of uptake with corresponding CT anatomy. The CT images themselves are nonenhanced and are somewhat limited for evaluation and characterization of pathology.
Complications
Complications of PET/CT are limited to complications related to IV access and include extravasation, localized pain, and swelling. Allergic reactions are rare.
Clinical Significance
Although breast cancer mortality rates have decreased in the past few decades, breast cancer remains the most commonly diagnosed cancer in women. The tumor, node, and metastasis (TNM) classification is utilized in breast cancer staging. The tumor or T stage refers to the primary tumor's actual size typically evaluated via conventional techniques such as MRI, ultrasound, and mammography. The nodal or N stage refers to axillary nodal staging. Axillary nodes are commonly first evaluated on mammography and ultrasound. Sentinel lymph node biopsy has become a standard approach with intraoperative histopathological analysis. Metastasis or M stage refers to identifying extra-axillary lymph nodes involvement and distant metastatic disease and is the major contribution of FDG PET.
A retrospective study analyzed breast cancer patients who underwent cancer staging performed initially clinically. Histopathological results followed by PET/CT examinations found 35% of patients' cancer staging was modified following PET imaging evaluation. The study reported that 68% of patients were upstaged to stage 3B following FDG PET/CT imaging.
The location and number of extra-axillary metastatic lymph nodes are an important prognostic indicator in breast cancer. The knowledge of their presence changes the stage and the management of the disease. Similarly, bony metastasis is frequently observed, especially in breast cancer, and might be evaluated via Tc99MDP bone scan; however, studies have found that FDG PET has a higher rate of specificity and a greater potential for monitoring treatment response.[8]
Enhancing Healthcare Team Outcomes
Breast cancer diagnosis and treatment use a multidisciplinary team's multimodality imaging approach to provide thorough evaluation and staging. Breast cancer detection begins with skilled mammography technicians and physician radiologists trained under Mammographic Quality Standard Act (MQSA) program guidelines to acquire and interpret screening mammography.[9] The importance of quality control in imaging acquisition is emphasized with both technicians and interpreting physicians to improve the quality of screening interpretations.
While imaging may be the center of breast cancer detection and staging, fluent conversation with the institution's breast surgeons and radiation oncologists is crucial in providing complete patient care and appropriate imaging workup. Collaborative multidisciplinary tumor boards allow for discussion with all treatment team members, ensuring up-to-date workup and oncologic and surgical management of breast cancer patients, including the appropriate use of PET/CT.