Continuing Education Activity
Myocardial perfusion scan is a widely performed procedure to diagnose ischemic heart disease. This activity reviews the importance of myocardial perfusion scan and highlights the interprofessional team's role in performing this procedure.
Objectives:
Identify the indications for myocardial perfusion scan
Describe the technique of performing a myocardial perfusion scan.
Review the clinical significance of myocardial perfusion scan.
Summarize how employing an interprofessional team approach can improve patient outcomes when using myocardial perfusion scanning on appropriate patient populations.
Introduction
Myocardial perfusion single-photon emission computed tomography (MPS) is an important, cost-effective, and widely used non-invasive imaging modality. With the advancement in imaging techniques and for early detection of coronary artery disease, it is estimated that 9.1 million tests are performed annually in the United States.[1]
Myocardial perfusion scan plays a crucial role in diagnosing ischemic coronary artery disease, predicting prognosis, assessing myocardial viability and effectiveness of medical therapy.[2] The sensitivity of this test is improving continuously due to better technologies, new software, and radiotracers.[3]
During a myocardial perfusion scan, a gamma camera detects radiotracer which is injected intravenously to measure the distribution of coronary blood flow in the myocardium. By rotating the gamma camera at the regular angular interval in a 180-degree arc, multiple planar projections are collected. Myocardial uptake of tracer for scan dependent on two things.First transportation of radiotracer to the cell surface which is flow-mediated. Second, it requires the intact cell membrane to extract radiotracer. The extraction of radiotracer is directly dependent on blood flow.
The same phenomena which cause a reduction in oxygen delivery and ischemic ECG changes on a treadmill can be assessed by perfusion defect on MPS. However, reduced uptake of tracer to specific region help to diagnose culprit artery responsible for patient symptoms. The difference in radiotracer uptake both at rest and stress, help to differentiate fixed and reversible defect.[4]
Anatomy and Physiology
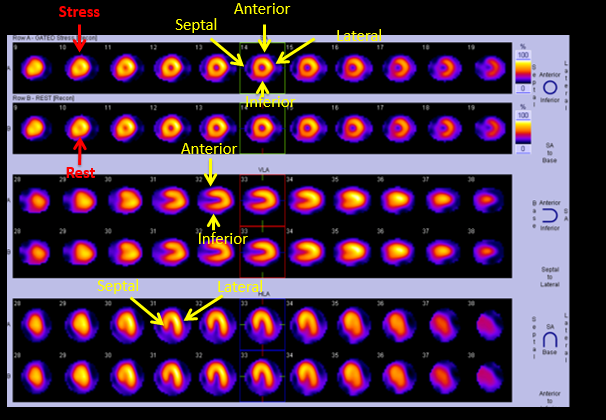
The myocardium is divided into 17 segments on the basis of a short axis and a long axis slice. On the short-axis view, there is a septal, anterior, lateral, and inferior wall. On the horizontal long axis, there are septal wall and lateral wall. On vertical long-axis view, there is an anterior and inferior wall.[4]
The anterior and septal wall is supplied by the left anterior descending artery, the lateral wall is supplied by the left circumflex artery, and the inferior wall is supplied by the right coronary artery. Perfusion is graded from 0-normal uptake, 1-mildly reduced uptake, 2-moderately reduced uptake, 3-severely reduced uptake, and 4-no uptake. If there is no defect in both stress and rest images, it is normal myocardium (see Image. Normal Myocardial Perfusion Scan Showing Location of Segments). If there is a defect on stress images and normal rest images, it is ischemic myocardium. If there is a defect both on rest and stress, it is either scar or hibernating myocardium. Stress-induced cavity dilation on scan indicates severe and extensive coronary artery disease, either multivessel or left main involved.
Indications
Diagnosis of Ischemic Heart Disease With Intermediate-risk for CAD and or Risk Stratification of Patients with an Intermediate or High Likelihood of CAD
- For identification of extent, severity, and location of myocardial ischemia
- Assess the functional significance of intermediate coronary artery stenosis
- Intermediate Duke Treadmill score (score between 4 and -11) on exercise stress test (ETT)
- Repeat testing in patients with a change in their ischemic symptoms
- Repeat testing in 1 to 3 years in patients with a high likelihood of coronary artery disease
- Severe coronary calcification on CT angiogram with unpredictable ECG
- Asymptomatic patients but with high-risk occupation( such as firefighters and pilots)
MPS is contraindicated for the screening of asymptomatic patients with a low likelihood of ischemic coronary artery disease
Assessment of Interventions and Therapy in Ischemic Heart Disease
- To assess patients 3 to 5 years after revascularization (either CABG or Coronary angioplasty) in high-risk asymptomatic patients
- Repeat testing to evaluate the therapeutic efficacy in patients with ischemic heart disease
MPS is contraindicated for routine assessment of patients after coronary angioplasty or CABG
Before Non-cardiac Surgery
- Intermediate-risk surgery or vascular surgery and risk factors with poor functional capacity (<4 METS)[5]
MPS is contraindicated in low-risk surgery and intermediate-risk surgery or vascular surgery and good functional class.
Contraindications
MPS is absolutely contraindicated in pregnant or breastfeeding patients, acute myocardial infarction (<2 days), acute myocarditis, acute pulmonary embolism, acute aortic dissection, acute symptomatic medical illness (such as metastatic cancer), severe symptomatic aortic stenosis, severe pulmonary artery hypertension, high-risk unstable angina, congestive heart failure, severe hypertension (>200/110 mmHg) and sustained cardiac arrhythmias.[6]
MPS is relatively contraindicated in patients with significant left main coronary artery disease, asymptomatic severe aortic stenosis (mean gradient > 40 mmHg, aortic valve area < 1cmsq, aortic jet velocity > 4 m/sec), hypertrophic obstructive cardiomyopathy, or forms of severe left ventricular outflow obstruction, complete heart block.
Equipment
The equipment required for a myocardial perfusion scan include:
- Treadmill machine for exercise
- Pharmacologic agents vasodilators and Ionotropes
- The antidote to reverse the effects of vasodilator and inotropes if required
- Radiotracer
- Myocardial perfusion gamma scan machine
Preparation
Patient preparation: Before the test, fasting for 3hours and caffeine-containing foods and drinks should be avoided for at least 12 hours. Blood pressure medications with antianginal properties (beta-blocker, calcium channel blocker, and nitrates) should be held 12 hours before the procedure.
Technique or Treatment
Stress
There are two ways to perform stress testing:
- Exercise
- Pharmacological
Exercise
This mode is preferable, as it also informs the functional capacity of the patient. The Bruce protocol is applied for exercise, and the patient walks on a treadmill until 85% of MPHR (Maximum predicted heart rate) is achieved. The achievement of target MPHR (maximum predicted heart rate) is not an indication to end the test earlier. The radiotracer injected as close to peak exercise as possible.
Patients should be encouraged to exercise for at least 1 minute after the radiotracer injection. However, exercise should be terminated early if patients start having moderate to severe chest pain, marked shortness of breath, extreme fatigue, ataxia, dizziness, or near-syncope, signs of decreased peripheral perfusion such as cyanosis and pallor, patient are not able to exercise further, drop in systolic blood pressure of greater than 10 mmHg from baseline, hypertensive response (systolic blood pressure >230 mmHg and/or diastolic pressure>115 mmHg), unable to monitor the electrocardiogram or systolic blood pressure and in patients with implantable cardioverter defibrillators, when the heart rate achieved is within 20 beats per minute of the lowest heart rate at which therapy (anti-tachycardia pacing or shock) is programmed to be delivered.
The recommendation to terminate exercise tests early on an electrocardiogram basis are excessive ST-segment depression (>2 mm from baseline), ST elevation (>1 mm), sustained supraventricular tachycardia, or ventricular tachycardia, development of LBBB or intraventricular conduction delay that cannot be differentiated from ventricular tachycardia.[7]
Pharmacologic Agents
Vasodilators: dipyridamole, adenosine, and regadenoson are three agents used as vasodilators for MPS. Vasodilator stress is recommended in all patients who are not able to exercise or submaximal exercise. It is preferable to do a stress test with a vasodilator instead of exercise if the patient has baseline LBBB.
Vasodilator test is contraindicated in high-grade AV block, patient with a history of severe reactive airway disease and history of intake of caffeinated drinks. The dose for myocardial perfusion scan of vasodilators are dipyridamole 0.56 mg/kg, adenosine 140 mcg/kg/min and regadenoson 0.4 mg.
Intravenous adenosine continuous infusion starts at 140 mcg/kg/min, radiotracer injection should be given at 3 minutes, and then adenosine infusion continued for the next 3 minutes. A single intravenous dose of 0.4 mg is given for regadenoson, followed by 5 ml normal saline flush, and radiotracer is given at 10 to 20 seconds after the normal saline flush.
For dipyridamole, continuous infusion is given at 0.56 mg/kg for 4 minutes, then it stops, and radiotracer should be given after 3 to 5 minutes of stoppage of dipyridamole infusion. To reverse the effects of vasodilators, aminophylline can be given 50 to 250-mg intravenously.[8]
Ionotropic: Iontropes indicated in patients who have contraindications to exercise and vasodilator. Dobutamine is a commonly used inotrope for MPS. Dobutamine infusion started at 5 to 10 mcg /kg/min and increases after every 2 mins until MPHR(Maximum predicted heart rate) is achieved. Radiotracer injected once MPHR (maximum predicted heart rate) achieved then dobutamine should be continued for the next minute. Dobutamine is contraindicated in patients with severe hypertension, unstable arrhythmia, and severe left main disease.
Radiotracer
There are two commonly used radiotracers for MPS.
- Thallium-201
- Technetium–99
Thallium-201 is a monovalent cation, property similar to potassium. It has a half-life of 73 hours and emits 80 keV photons. Its peak myocardial concentration achieves in 5 minutes and has the property of rapid clearance from the intravascular compartment. The differential washout-clearance of thallium 201 is more rapid from normal myocardium. As hyperinsulinemia stated, it reduces blood concentration and slow distribution of thallium 201, so fasting is essential. Thallium should be injected at peak stress, and images should be taken 10 to 15 mins of injection. Rest images after 4 hours of stress image.[9]
Advantages of thallium-201:
- Its redistribution property allows single-injection studies and viability assessment.
- It is less expensive.
- It has less abdominal and hepatic uptake during exercise
Technetium–99 has a half-life of 6 hrs and emits 140keV photons. Technetium–99 tracers bound by mitochondria, limited washout occurs, so imaging can commence later and can be repeated. Rest images are obtained after 15 to 45 minutes of stress.[10]
Advantages of technetium–99:
- It has a shorter half-life, which allows for a higher dose resulting in better count statistics
- It has less radiation exposure and attenuation effects
- It has higher energy levels, which allow improved resolution.
Complications
The complications from a myocardial perfusion scan are rare. Few possible complications are:
- Radiation exposure (low radiation exposure)[11][12]
- Myocardial infarction (rare)
- Arrhythmia (rare)
- Non-ischemic chest pain, especially from dipyridamole and adenosine
- Wheeze
Clinical Significance
Myocardial perfusion scan plays a vital role in diagnosing ischemic heart disease and assessing the effectiveness of medical management in patients with known coronary artery disease. It is a useful non-invasive test to assess the blood supply of the myocardium. It also helps in preoperative cardiovascular risk assessment of patients with poor functional class and intermediate-risk surgery. The risk of perioperative cardiovascular risk is directly proportional to the severity of perfusion defect on myocardial perfusion scan.
Enhancing Healthcare Team Outcomes
To perform a myocardial perfusion scan requires an interprofessional team that includes a nuclear cardiologist or radiologist, staff nurse, and nuclear technologist. It is essential to take a proper history and perform a physical examination before the procedure. The decision of which mode of stress should be selected depends upon the patient's functional class and comorbid. It is important to give a radiotracer and performs a scan at the appropriate time in order to get the best results.