Introduction
The World Health Organization (WHO) defines child abuse and child maltreatment as "all forms of physical and/or emotional ill-treatment, sexual abuse, neglect or negligent treatment or commercial or other exploitation, resulting in actual or potential harm to the child's health, survival, development or dignity in the context of a relationship of responsibility, trust or power."[1]
There are four main types of abuse:
- Neglect (physical or emotional)
- Physical abuse
- Psychological or emotional abuse
- Sexual abuse
There are significant morbidity and mortality associated with child abuse due to a child's inability to protect themselves. For the diagnosis of child abuse to be made, healthcare providers need to maintain a high index of suspicion.[2][3][4] The New York State government has established a legal obligation of mandated reporters to intervene if there is evidence or suspicion of abuse, maltreatment, or neglect of a child less than 18 years of age.
New York Legal Definitions for Abuse, Maltreatment, and Neglect (New York State Family Court Act)
The purpose of the New York State law is to establish procedures to protect children from injury or mistreatment and safeguard their physical, mental, and emotional well-being. It provides due process for determining when the state, through its family court, may intervene against the wishes of a parent on behalf of a child so that the child's needs are appropriately met. The following is a summary of key definitions:
- "Respondent": any parent or other person legally responsible for a child's care who is alleged to have abused or neglected the child.
- "Child": any person or persons < 18 years of age.
- “Abused child": a child whose parent or another person legally responsible for his care:
(i) inflicts or allows to be inflicted upon such child physical injury other than by accidental means which causes or creates a substantial risk of death, serious or protracted disfigurement, protracted impairment of physical or emotional health, or protracted loss or impairment of the function of any bodily organ; or
(ii) creates or allows to be created a substantial risk of physical injury to such child by other than accidental means which would be likely to cause death or serious or protracted disfigurement, protracted impairment of physical or emotional health, or protracted loss or impairment of the function of any bodily organ; or
(iii) (A) commits, or allows to be committed an offense against such child defined in article one hundred thirty of the penal law; (B) allows, permits, or encourages such child to engage in any act described in sections 230.25, 230.30, 230.32, and 230.34-a of the penal law; (C) commits any of the acts described in sections 255.25, 255.26, and 255.27 of the penal law; (D) allows such child to engage in acts or conduct described in article two hundred sixty-three of the penal law; or (E) permits or encourages such child to engage in any act or commits or allows to be committed against such child any offense that would render such child either a victim of sex trafficking or a victim of severe forms of trafficking in persons pursuant to 22 U.S.C. 7102 as enacted by public law 106-386 or any successor federal statute; (F) provided, however, that (1) the corroboration requirements contained in the penal law and (2) the age requirement for the application of article two hundred sixty-three of such law shall not apply to proceedings under this article.
- “Neglected child” or “maltreated child”: a child:
(i) whose physical, mental, or emotional condition has been impaired or is in imminent danger of becoming impaired as a result of the failure of his parent or other person legally responsible for his care to exercise a minimum degree of care
(A) in supplying the child with adequate food, clothing, shelter or education in accordance with the provisions of part one of article sixty-five of the education law, or medical, dental, optometrical or surgical care, though financially able to do so or offered financial or other reasonable means to do so, or, in the case of an alleged failure of the respondent to provide education to the child, notwithstanding the efforts of the school district or local educational agency and child protective agency to ameliorate such alleged failure prior to the filing of the petition; or
(B) in providing the child with proper supervision or guardianship, by unreasonably inflicting or allowing to be inflicted harm, or a substantial risk thereof, including the infliction of excessive corporal punishment; or by misusing a drug or drugs; or by misusing alcoholic beverages to the extent that he loses self-control of his actions; or by any other acts of a similarly serious nature requiring the aid of the court; provided, however, that where the respondent is voluntarily and regularly participating in a rehabilitative program, evidence that the respondent has repeatedly misused a drug or drugs or alcoholic beverages to the extent that he loses self-control of his actions shall not establish that the child is a neglected child in the absence of evidence establishing that the child's physical, the mental or emotional condition has been impaired or is in imminent danger of becoming impaired as set forth in paragraph (i) of this subdivision; or
(ii) who has been abandoned, in accordance with the definition and other criteria set forth in subdivision five of section three hundred eighty-four-b of the social services law, by his parents or other person legally responsible for his care.
The terms “maltreatment” and “neglect” are often used interchangeably but have different definitions. "Maltreatment" includes acts of omission and commission, whereas "neglect" only includes acts of omission. Maltreatment includes neglect, but neglect does not include maltreatment.[1]
- “Person legally responsible": the child's custodian, guardian, or any other person responsible for the child's care at the relevant time. Custodian may include any person continually or at regular intervals found in the same household as the child when the conduct of such person causes or contributes to the abuse or neglect of the child.
- “Impairment of emotional health/condition”: a state of substantially diminished psychological or intellectual functioning in relation to, but not limited to, such factors as failure to thrive, control of aggressive or self-destructive impulses, ability to think and reason, or acting out or misbehavior, including incorrigibility, ungovernability or habitual truancy, provided, however, that such impairment must be clearly attributable to the unwillingness or inability of the respondent to exercise a minimum degree of care toward the child.
- “Child protective agency”: the child protective service of the appropriate local department of social services or such other agencies with whom the local department has arranged for the provision of child protective services under the local plan for child protective services or an Indian tribe that has entered into an agreement with the state department of social services pursuant to section thirty-nine of the social services law to provide child protective services.
- “Parent”: a person who is recognized under the laws of the state of New York to be the child's legal parent.
- “Relative”: any person who is related to the child by blood, marriage, or adoption and who is not a parent, putative parent, or relative of a putative parent of the child.
- “Suitable person”: any person who plays or has played a significant positive role in the child's life or the life of the child's family.
Types of Abuse and Neglect
- Physical neglect
- Physical abuse
- Emotional neglect
- Emotional abuse
- Sexual abuse
Physical Neglect
Physical neglect is the most common form of abuse. It is the failure to provide a child with adequate food, shelter, clothing, education, hygiene, medical care, protection from hazards in the environment, basic needs, or supervision needed for normal growth and development.[5]
Physical Abuse
Physical abuse of a child includes any non-accidental physical injury of a child inflicted by a parent or a caretaker resulting in or risking serious disfigurement, impairment of physical or emotional health, and loss of bodily function or death. Physical abuse includes beating, burning, biting, shaking, and excessive corporal punishment.[5]
Emotional Neglect
Emotional neglect is the failure of a parent or caregiver to supply a child with the love and support necessary for healthy emotional development. Examples include failure to provide warmth, attention, supervision, affection, praise, or encouragement to a child.
Emotional Abuse
Emotional abuse is commonly defined as the non-physical maltreatment of a child that can seriously interfere with his or her positive emotional development. Patterns of abusive behavior can include constant rejection, terrorizing, exposing a child to corruption, violence or criminal behavior, irrational behavior, and verbal abuse (excessive yelling, belittling, and teasing). Emotional abuse has the potential to cause serious cognitive, affective, or other behavioral health problems.
Sexual Abuse [6]
Sexual abuse is the involvement of dependent, developmentally immature children in sexual activities that they do not fully comprehend, to which they are unable to give consent, or that violate the social taboos of family roles. Sexual abuse and maltreatment include situations in which the parent, caregiver, or another person legally responsible for a child under 18 years of age, commits or allows to be committed any one of the following activities:
- Touching a child’s mouth, genitals, buttocks, breasts or other intimate parts for the purpose of gratifying sexual desire; or forcing or encouraging the child to touch the caregiver, or other person legally responsible, in this way for the purpose of gratifying sexual desire.
- Engaging or attempting to engage the child in sexual intercourse or sodomy.
- Forcing or encouraging a child to engage in sexual activity with other children or adults.
- Exposing a child to sexual activity or exhibitionism for the purpose of sexual stimulation or gratification of another.
- Permitting a child to engage in sexual activity that is not developmentally appropriate and when such activity results in the child suffering from emotional impairment.
- Using a child in a sexual performance such as a photograph, play, motion picture, or dance regardless of whether the material itself is obscene.
In addition, it is a crime to give indecent material to a child. Sexual abuse and maltreatment include such criminal offenses as rape, sodomy, other non-consensual sexual conduct, and prostitution.
Social Service Laws Related to Care of Children in Residential Care
Abused
A person with a handicapping condition who is 18 years or older who is in residential care in one of the following facilities may be defined as an abused child:
- NYS School for the Blind (Batavia)
- NYS School for the Deaf (Rome)
- A private residential school which has been designed for special education
- A special act school district or a state-supported school for the deaf or blind with a residential component.
Neglected
In New York State, a neglected child in residential care (including facilities operated by the Department of Social Services [DSS], Division for Youth [DFY], Office of Mental Health [OMH], Office for People with Developmental Disabilities [OPWDD], or the State Education Department [NYSED]) means a child whose custodian impairs, or places in danger of impairment, the child's physical, mental or emotional condition:
- By intentionally administering to the child, any prescription drug not ordered.
- Failing to adhere to standards for the provision of food, clothing, shelter, education, medical, dental, optometric, or surgical care, or the use of isolation or restraint.
- Failing to adhere to standards for the supervision of children by inflicting or allowing to be inflicted physical harm or risk of harm.
- Failing to conform to applicable state regulations for appropriate custodial conduct.
Maltreated
The Social Services Act includes a maltreated child 18 years of age or older, who is neglected and resides in one of the special residential care institutions previously listed.
Abandoned Infant Protection Act
First enacted in July 2000 and later amended in August 2010, the “New York State Abandoned Infant Protection Act” allows a person to abandon their infant in a safe manner. This law designates specific locations as "safe-havens" for parents to relinquish their unharmed newborns, ensuring that unwanted infants are surrendered to persons who can guarantee the child's safety and well-being. It also protects parents who feel that they have no other alternative to protect their child from harm. While the law protects those that relinquish unharmed infants, the abandonment of newborn infants in unsafe places is an example of extreme neglect with criminal penalties.
Charges of abandonment may be incurred unless the following criteria are met:
- Infant < 30 days old
- Intent that the infant be safe from physical injury and receive appropriate care
- Infant left with an appropriate person or suitable location such as a hospital, police station, or fire department and notifies an appropriate person of the infant's location.
- Intent to abandon the infant by relinquishing responsibility for and rights wholly
Any mandated reporter who learns of abandonment must fulfill mandated responsibilities even if unsure of the name of the person abandoning the child.
Etiology
All races, ethnicities, and socioeconomic groups may be affected by child abuse, with boys and adolescents more commonly affected. Infants have increased morbidity and mortality with physical abuse. Factors that increase a child's risk of abuse include:
- Individual factors of respondent or child: a child's disability, single parent, maternal smoking, or a parent's depression
- Familial factors: domestic violence at home, > 2 siblings at home
- Community factors: lack of recreational facilities and other community support
- Societal factors: poverty
- Living in an unrelated adult's home
- Previous report to child protective services (CPS)
Risk Factors that Increase Child Abuse and Maltreatment (Center for Disease Control):[1][5]
- Alcoholism and substance abuse
- Community violence
- Children younger than 4 years of age
- Family disorganization, dissolution, and violence
- Family history of child abuse and maltreatment
- Intellectual disability
- Lack of understanding of development and needs
- Limited education
- A large number of dependent children
- Low income
- Mental health issues
- Parenting stress
- Parental emotions that tend to justify maltreatment
- Physical disability or illness
- Poor parenting skills
- Social isolation
- Single parenthood
- Transient caregivers
- Young age
- Unemployment rates
There are also “protective or preventive factors” that decrease the risk of child maltreatment, including:
- Family support
- Parental concern
- Parental education regarding child development and parenting
- Social support
- Parental resilience.[6][7][8]
Potential Long-term Sequela of Child Abuse[1][5]
- Physical and mental health conditions
- Low life potential
- Premature death
- Substance abuse
Epidemiology
Each year, over 3 million children are investigated nationally by Child Protective Services for child abuse and neglect. Of those, 20% are found to have evidence of maltreatment.[9]
There are over 150,000 referrals for abuse and neglect in New York State, with nearly half of them confirmed victims. Male and female percentage of victims are similar. The highest risk of abuse and neglect are in children < 3 years of age and in African American and Native American children. Of those abused, approximately 75% are neglected, 15-20% are physically abused, and 5-10% are sexually abused.[1][5][10]
History and Physical
Diagnosis of child abuse, neglect, or maltreatment may be difficult as the victim may be unable to provide information due to pre-verbal or nonverbal status, fear, or severe injuries. Also, the perpetrator rarely admits to the abuse, and witnesses are uncommon. Physicians may see children of maltreatment in a variety of situations that include:
- An adult or mandated reporter brings the child in for evaluation when they are concerned about abuse.
- A child or adolescent comes in disclosing the abuse.
- A perpetrator brings the patient for medical care with concern that the abuse is severe.
- A child presents for care unrelated to abuse, and abuse may be found incidentally.
Physical abuse should be considered in the evaluation of all injuries of children. A thorough history of present illness is vital to make a correct diagnosis. Information about the child's behavior before, during, and after the injury should be obtained. History-taking should include the interview of the verbal child and each caretaker separately. The parent or caretaker should be allowed to provide their history without interruptions to not be influenced by the physician's questions or interpretations.
Pediatric physical abuse should be considered in the following:
- Injury in a non-ambulatory infant
- Injury in a nonverbal child
- Injury inconsistent with the child's physical abilities
- A statement of harm from the verbal child
- Mechanism of injury not plausible
- Multiple injuries, particularly at varying stages of healing
- Bruises on the torso, ear, or neck in a child younger than 4 years of age
- Burns to genitalia
- Stocking or glove distributions or patterns of injury
- The caregiver is unconcerned about the injury.
- An unexplained delay in seeking care
- Inconsistencies or discrepancies in the histories provided
"TEN 4" is a useful mnemonic to recall which bruising locations are of concern in cases involving physical abuse: bruises of the Torso, Ear, or Neck in a child < 4 years of age or any bruising in a child < 4 months of age are concerning for abuse.
Other injuries that are highly suggestive of abuse include:
- Retinal hemorrhages
- Posterior rib fractures
- Classic metaphyseal lesions[1][5]
Signs And Symptoms Of Child Abuse
Physical Abuse[5]
Pediatric Abusive Head Trauma (PAHT)[11]
Pediatric Abusive Head Trauma (PAHT) or “shaken baby syndrome” is a common cause of abusive head injury in children and is associated with significant morbidity and mortality. PAHT is an injury to the intracranial contents or skull of an infant or young child inflicted by blunt impact or violent shaking. An evaluation may begin with a skull X-ray or head ultrasound but often requires a head CT for definitive diagnosis, particularly in an emergency setting or in an unstable child. Common head CT findings in PAHT include subdural hematomas and diffuse axonal injury. The evaluation should also include an ophthalmologic examination to evaluate for retinal hemorrhages.
Signs and symptoms of PAHT are often non-specific and may include:
- Absence of hair due to vigorous hair pulling
- Apnea
- Bulging fontanelles
- Coma
- Decreased appetite
- Irritability
- Unexplained injury to the frenulum, jaw, nose, or teeth
- Lethargy
- Retinal hemorrhages
- Seizures
- Vomiting
Long term sequela of PAHT includes:
- Blindness
- Cerebral palsy
- Developmental delay
- Hearing loss
- Learning difficulties
- Seizures
Glutaric aciduria type 1 is a rare metabolic disease that can cause retinal hemorrhages and subdural hematomas and may be mistaken for PAHT.
Skeletal Trauma
The majority of abusive fractures occur in non-ambulatory infants and toddlers < 18 months of age. Any unexplained fracture in a child should raise suspicion for child abuse. The following fractures may be concerning for physical abuse:
- Skull fractures
- "Bucket handle" fractures or "corner" fractures due to twisting of the ends of the long bones.
- Long bone fractures in a non-ambulatory child
- Greenstick fractures
- Posterior or lateral rib fractures
- Scapular fractures other than those caused by birth trauma
- Spinal fractures
- Sternal fractures
- Multiple fractures in various stages of healing
- Facial fractures
- Skeletal trauma with other injuries
Symptoms that raise suspicion for fracture include:
- Red, swollen, painful joint or limb
- Patient crying with pain or irritability
- Local tenderness to palpation
- Unwillingness to move the limb
Organic causes of fractures that may be mistaken for child abuse include:
- Osteogenesis imperfecta
- Osteopenia
- Metabolic bone disease: Rickets, vitamin C and copper deficiency
- Oncological disorders
- Ehlers-Danlos syndrome
- Injury sustained during resuscitation: rib fractures, internal organ contusions, retinal hemorrhages[12]
Abdominal Trauma:
Abdominal injury may result in significant morbidity and mortality. The most commonly injured organs are the spleen (over 60%), liver, pancreas, kidneys, and, less frequently, small bowel and bladder.[13] Overt findings may not always be present. Rapid screening, such as the Focused Assessment with Sonography for Trauma (FAST), may assist in evaluating for acute injury along with laboratory tests including amylase, lipase, liver function tests, and urinalysis. Any positive ultrasound or laboratory finding suggests the need for further workup or imaging, such as an abdominal and pelvic CT scan.
Bites
Human bites are a “2 to 5 cm oval or circular mark, made by two opposing concave arcs, with or without associated ecchymosis”.[14] Bitemarks can provide useful evidence in cases of physical assault of a child and can also be a source of the assailant’s DNA. Measurement of the inter-canine distance of the bite may help distinguish between an adult's bite (3.0 to 4.5 cm), a small adult’s bite (2.5 to 3.0 cm), or a child’s bite (2.5 cm, child's deciduous teeth). However, the data is not validated in clinical practice.
Bruising
A bruise is the most common soft tissue injury in cases of physical abuse. Bruises can be characterized as:
- Petechiae: very small, pinpoint erythematous, non-blanching bruises caused by broken capillaries.
- Purpura: small bruises occurring in groups or a single bruise up to 1 cm
- Ecchymoses: larger bruise > 1 cm.
Bruising in non-abused children is most commonly found on the knees, shins, and bony prominences. Bruising in non-ambulatory children is uncommon and is concerning for non-accidental trauma. Commonly in abuse, bruises will be found on the backside of the child, beginning at the neck and continuing down to the knees, including shoulders and the child's arms. This area has been referred to as the child's "primary target zone." The following pattern of bruises are potentially worrisome:
- Clustered or patterned
- Inconsistent with history
- Large or numerous
- Present in various stages of healing
- Present in non-ambulatory children[15]
A pediatrician needs to differentiate bruises from “pseudo-bruises" such as Mongolian spots (grey-blue, can be found anywhere on the body and have clear cut margins), maculae cerulae (bluish spot on the skin due to pubic lice), and allergic shiners (more brown than blue, may be confused with black eyes). Also on the differential diagnosis for bruises are bleeding disorders, vasculitides, hypersensitivity syndromes, and various cultural practices such as spooning, coining, and cupping.
Burns
Burns are often accidental and can lead to significant morbidity and mortality in children. Burns that cannot be explained by history, present with a significant delay in seeking care, have characteristic sharp lines of demarcation (also called the line of immersion), or have a symmetric pattern are concerning for child abuse. Other typical burns for child abuse include:
- Immersion burns: doughnut burns (as buttocks make firm contact with the base of a container) or zebra burns (a child immersed in a flexed position with spare the creases of child’s body giving a striped configuration)
- Glove-like or sock-like burns from immersion of child’s feet and hands
- Dry contact burns patterned like a household appliance, such as an iron, stove, heater, grate, radiator pipe, hot plate, or curling iron.
- Round cigarette burns
- Rope burns
The differential diagnosis of burns includes:
- Chemical and irritants: bleach, complementary and alternative therapies
- Infection: impetigo, blistering distal dactylitis, ringworm
- Stephens-Johnson Syndrome or toxic epidermal necrolysis
- Dermatological conditions: diaper dermatitis
- Scalded skin syndrome
Lacerations
Lacerations are a pattern of injury in which skin and the underlying tissues are cut or torn. Unexplained lacerations in the following areas are potentially concerning:
- Arms, eyes, genitalia, gums, legs, lips, mouth, and torso
Behavioral Signs of Physical Abuse
In addition to the history and physical examination, observation of the child's behavior, and the child-caregiver interactions during the encounter can provide clues to the potential for physical abuse.
Behavioral indicators of abuse in children include:
- Aggressive, destructive, or disruptive behavior
- Apprehensive when other children cry
- Compulsions, hypochondria, phobias, and obsessions
- Fear of going home
- Fear of caregiver
- Emotionless, passive, or withdrawn
- Habit disorders
- Lack of interest in activities for age
- Overly seeks affection
- Self-injurious behaviors
- Suicide attempts
- Return of bedwetting
- Unexpected sexual knowledge for age
- Unwilling to change clothes for physical education or sports
- Wearing concealing clothing
Behavioral indicators of abuse in caregiver include:
- Alcohol or drug abuse
- Concealment of injuries
- Disciplines harshly
- Describes child as evil
- Delays medical care
- History of abuse as a child
- Lack of emotional control
- Lack of parenting skills
- Lack of support network
- Multiple providers
- Overly protective or jealous
- Poor self-esteem
- Unconcerned about child's health or well-being
- Unclear or conflicting explanation of the child's injury
- Uses the child to meet emotional or physical needs
- Unrealistic expectations
Sexual Abuse
Sexual behaviors are rare in infants except for hand to genital contact. They become more prevalent in children 2-5 years of age as they become aware of their body parts, and then they become less common > 5 years as children become aware of social rules. However, if a child has inappropriate behaviors such as an older child touching other children's genitals, undressing in front of others, and looking at others undressing, there should be a concern.
Sexual abuse involves the coercion of a dependent, developmentally immature person to commit a sexual act with someone older, sometimes for financial gain (i.e., sex trafficking).[10][16][17][18]
A normal physical examination does not rule out sexual abuse, and the most common finding in sexual abuse is a normal physical examination. In most cases, evidence that sexual abuse has occurred is based on the child's statement. Suspicion should be raised if any of the following are present:
- Alcohol and drug addiction
- Adolescent pregnancy
- Agoraphobia
- Alopecia areas
- Anogenital trauma
- Anxiety
- Bruises
- Burns
- Bloody or torn underwear
- Bruises on the palate
- Depression and suicidal thoughts
- Diseases that are untreated or not diagnosed
- Fractures
- Head injuries
- Lacerations
- Ligature injuries
- Malnourishment
- Painful urination and bowel movements
- Painful sitting or walking
- Panic attacks
- Poor hygiene
- PTSD
- Recurrent urinary tract infections
- Sexually transmitted diseases and pelvic infections
Epidemiology
It may be a challenge to recognize sexual abuse as physical evidence may be overlooked or not present. Considerations include: [16][17][18]
- Every culture, class, and race is at risk.
- Boys are less likely to report their victimization.
- Children may be reluctant to disclose abuse by a family member or friend.
- A young child may not have the language skills to describe events.
- Girls are sexually abused more often than boys.
- Perpetrators are more commonly male.
- Most perpetrators are known to the victim.
There is no average profile of a child molester or victim; any community member may be an offender.
Long-term effects of sexual abuse include:
- Anxiety
- Difficulty concentrating
- Depression
- Self-injurious behaviors
- Substance abuse
- Suicide
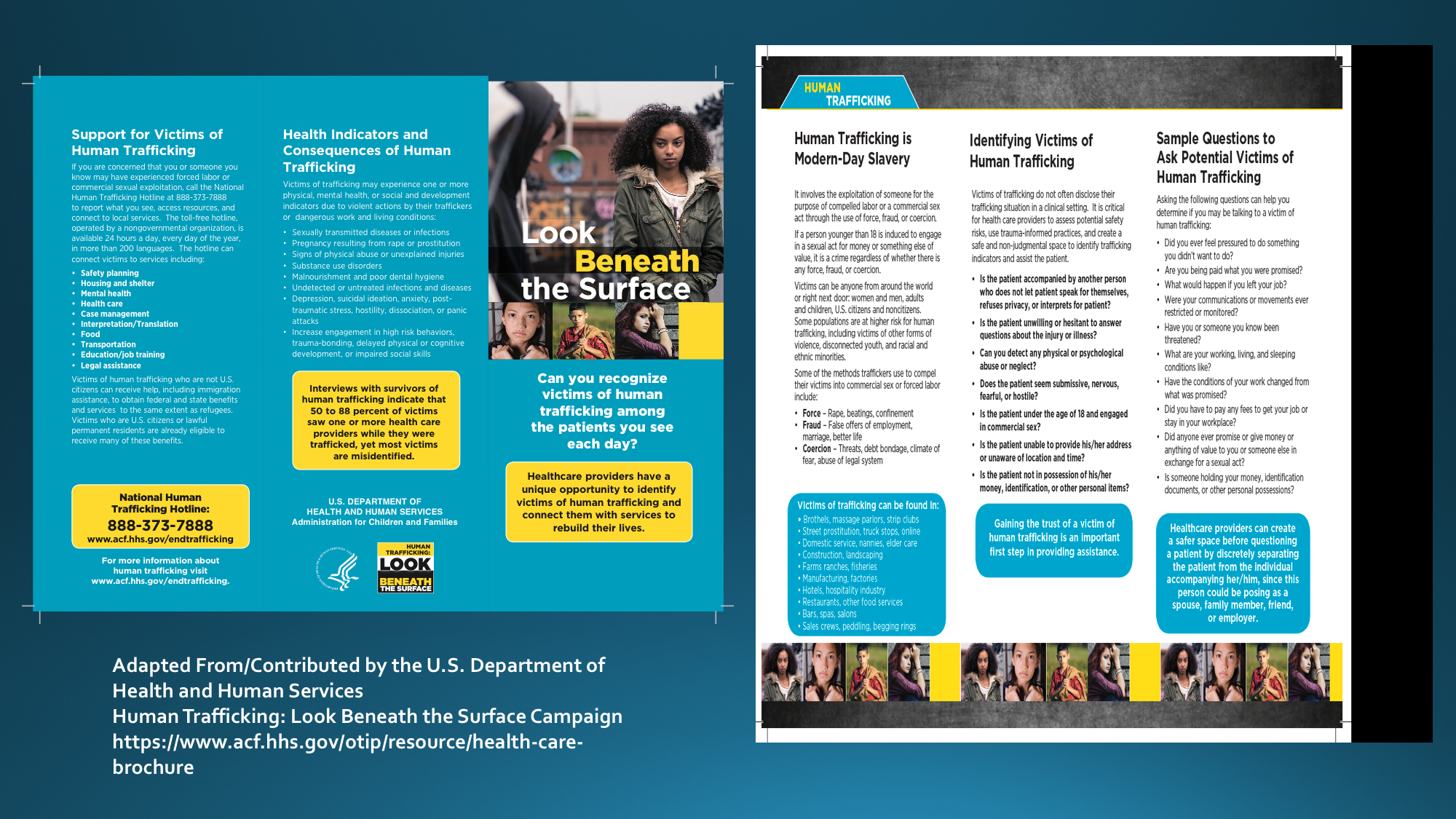
Sex Trafficking
The Trafficking Victims Protection Act defines "severe forms of trafficking in persons" as (a) sex trafficking in which a commercial sex act is induced by force, fraud, or coercion, or in which the person induced to perform such an act has not attained 18 years of age; or (b) the recruitment, harboring, transportation, provision, or obtaining of a person for labor or services, through the use of force, fraud, or coercion for the purpose of subjection to involuntary servitude, peonage, debt bondage, or slavery. Commercial sex act means any sex act on account of which anything of value is given to or received by any person.[10][19] Considerations include:
- The average age is of sex trafficking victims is 11 to 14 years.
- Frequently starts on the internet.
- The number of victims worldwide is in the millions, and half of the affected individuals are children.
- Women more commonly affected than men
Screening Questions
If sex trafficking is suspected, complete the physical examination in private, then consider the screening questions in the figure.[10][19][16][17][18]
Neglect
Physical examination may not only demonstrate signs of physical abuse but may show signs of neglect. The general examination may show poor oral hygiene with extensive dental caries, malnutrition with significant growth failure, untreated diaper dermatitis, or untreated wounds.
Indicators of physical neglect include:[5]
- Abandonment
- Drug withdrawal symptoms
- Delayed development
- Failure to thrive
- Hunger
- Inappropriate dressing
- Lack of supervision
- Poor hygiene
- Truancy
- Unattended physical problems
Emotional Neglect
Behavioral indicators of neglect in a child include:
- Alcohol or substance abuse
- Begging or stealing food
- Chronic fatigue
- Conduct disorders and delinquency
- Developmental delay
- Extended stays at school
- Habit disorders
- Hysteria
- Hypochondria
- Inhibition of play
- Absence of caretaker at home
- Obsessive-compulsive behaviors
- Overly compliant
- Overly demanding
- Passive-aggressive
- Phobias
- Runaway
- Sleep disorders
- Suicide attempt
Behavioral indicators of neglect in a legally responsible person include:
- Blaming the child for problems
- Inconsistent treatment
- Lack of caring
- Continued rejection
- Treating children unequally
Mandated Reporters:
All healthcare providers are mandated reporters, and, as such, they are required to make a report to child welfare when there is a reasonable suspicion of abuse or neglect. One does not need to be certain, but one does need to have a reasonable suspicion of the abuse. This mandated report may be lifesaving for many children. An interprofessional approach to the evaluation with the inclusion of a child-abuse specialist is optimal.
Forensic Evidence
If child abuse or neglect is considered, the history and physical examination findings may be used in legal proceedings. Photographs, diagrams, and detailed findings are helpful for recall at trial. Findings should be reported accurately and without bias. [16][17][18]
Photographs
New York Social Service Law allows any person or official required to take evidence for suspected abuse to take color photographs of visible trauma or radiographs. The images should be provided to Child Protective Services as soon as possible. Consent is not needed for a minor child to be photographed if child abuse is suspected and reported to the Statewide Central Register. A chain of custody should be maintained. The institutional protocol for releasing photographs should be followed.
Tips for taking photographs:
- Include the child's name, date of birth, medical record number, date and time of photographs, and name of the provider on an index card
- Take photos at various ranges: distant, mid-range, and close up.
- Use adequate lighting
- Include anatomic landmarks to identify the location of findings.
- Use a ruler placed on the skin to document the size of any findings.
- The child's face and body should be photographed for identification of the patient.
Victim Disclosures
If a child discloses abuse, they may only disclose part of what happened. Document in the child's own words and quote the child if possible. Avoid rushing the child or making promises you cannot keep. Explain to the child they may need to repeat the information. Methods to enhance disclosure include:[16][17][18]
- Ask who, what, where, and when
- Ask open-ended questions
- Avoid expressing emotion
- Be a good listener
- Remain calm
- Thank them for talking to you
- Use age-appropriate language
Indirect Hints
- Admitting to a problem but being unwilling to share
- My father, mother, brother, or sister would not let me sleep.
- My uncle, aunt, cousin, babysitter keeps bothering me.
Factitious Disorder[20][21]
Factitious disorder imposed on another or Munchausen syndrome by proxy is a form of child abuse. It typically occurs when a caretaker falsifies an illness in the child to gain attention. There generally are no obvious external monetary rewards.
Typical findings in factitious disorder include:[16][17][18]
- Deceptive behavior is evident in the absence of obvious external rewards.
- Falsification of physical or psychological signs or symptoms
- History of many hospitalizations with unusual signs and symptoms
- History of unusual death or illness in the family
- Improves when hospitalized but worsens when returns home
- Lab samples do not match the child.
- Not better explained by another mental disorder.
- Presents another individual to others as ill, impaired, or injured
- Signs and symptoms do not agree with the test results.
- Toxic or abnormal chemicals in the child's blood, stool, or urine
- Worsening of the child's symptoms by the perpetrator but not witnessed by healthcare professionals
Evaluation
Laboratory Tests
Laboratory evaluation may be performed to evaluate for other diseases as the causes of the injury. These laboratory tests can include:
- CBC: to evaluate for anemia and thrombocytopenia
- Coagulation profile: PT/INR, PTT
- Metabolic: glucose, BUN, creatinine, albumin, protein
- Liver: AST, ALT
- Pancreas: amylase, lipase
- Bleeding diatheses: von Willebrand antigen, von Willebrand activity, Factor VIII, Factor IX, and platelet function assays
- Bony disorders: calcium, magnesium, phosphate, alkaline phosphatase
Radiology
Any child < 2 years of age for whom there is a concern regarding physical abuse should have a complete skeletal survey obtained as part of the evaluation. Additionally, any sibling < 2 years of an abused child should also have a skeletal survey performed. A skeletal survey consists of 21 dedicated X-rays, as recommended by the American College of Radiology. The views include the skull, spine, chest/ribs, pelvis, femur, leg, foot, humerus, forearm, and hand. If the findings are abnormal or equivocal, either further dedicated X-rays of the area of concern and/or follow-up X-rays are indicated in 2 weeks to evaluate for healing fractures.
One should consider that the most common differential diagnosis of non-accidental injury is an accidental injury.[22][23][24][1][5]
Treatment / Management
Initial management of an abused child involves stabilization, including assessing the patient's airway, breathing, and circulation. Once ensured that the patient is stable, a complete history and physical examination are required. With the suspicion for any form of child abuse, CPS needs to be informed. The involvement of a child abuse specialist is important for optimal evaluation and management. If the patient is seen in an outpatient setting, transfer to an emergency department for laboratory and/or radiologic evaluation, and the appropriate continuation of care may be indicated. If a child is transferred to another physician or facility, the initial physician caring for the patient has the responsibility of reporting the case to CPS. It is the responsibility of the physician to recognize potential abuse, not to identify the perpetrator. The physician should continue to advocate for the child, ensuring that the patient receives the appropriate follow-up care and services.
Victims of sexual abuse should have their physical, mental, and psychosocial needs addressed. Baseline sexually transmitted infection (STI) and pregnancy testing should be performed, and empiric treatment for HIV, gonorrhea, chlamydia, trichomonas, and bacterial vaginosis infection for the adolescent victims should be offered. Also, emergency contraception to prevent unwanted pregnancy is most effective if given within 72 hours but may be offered up to 5 days after unprotected intercourse. Prepubertal patients are not provided with prophylactic treatment due to the low incidence of STIs in this age group. Urgent evaluation can prove extremely beneficial for patients needing prophylactic STI treatment, emergency contraception, managing anogenital injury, collecting forensic evidence, urgent child protection, or urgent care for suicidal ideation.[25][26][27][1][5][10]
Differential Diagnosis
The differential diagnosis for abuse depends on age, injury type, and signs and symptoms. The differential diagnosis of injury usually differentiates between accidental and inflicted trauma. An astute healthcare provider must carefully consider organic disease processes or accidental injury versus deliberately inflicted trauma.
- Accidental asphyxia[28]
- Accidental bruises
- Accidental fractures
- Accidental burns
- Accidental head injury
- Arteriovenous malformations
- Atopic dermatitis[29]
- Bleeding or hemorrhagic disorder[30][31]
- Birth trauma[32]
- Caffey disease[33]
- Chemical burn[34]
- Coining[35]
- Congenital syphilis[36]
- Contact dermatitis
- Cupping[35]
- Erythema multiforme[37]
- Factitious disorder
- Hemangioma[38]
- Henoch-Schönlein purpura[39]
- Hypervitaminosis A[40]
- Immune thrombocytopenic purpura[40]
- Impetigo[41]
- Inflammatory skin conditions
- Insect bites[42]
- Osteogenesis imperfecta[43]
- Osteomyelitis[44]
- Osteopenia
- Malignancy
- Meningitis[45]
- Menkes disease[46]
- Metabolic disease
- Mongolian spots[47]
- Nevi[48]
- Phytophotodermatitis[49]
- Rickets[50]
- Scurvy[51]
- Sunburn[52]
- Valsalva induced subconjunctival hemorrhage[53]
Complications
- Fractures
- Burns
- Disfigurement
- Emotional trauma
- Seizures
- Mental retardation
- PTSD
Consultations
- Neurosurgery
- Ophthalmologist
- Orthopedic surgeon
- Child protective services
- Social Work
- Psychiatrist
Deterrence and Patient Education
The following are some examples of deterrence and protective methods to reduce the incidence of children being abused, maltreated, or neglected. [1]
- Adequate housing
- Access to healthcare
- Access to social services
- Child monitoring
- Community support for abuse prevention and reporting
- Parental counseling
- Government or community sponsored child-parent centers
- Parental employment with available childcare
- Parent nurturing skill classes
- Parental role models
- Parent-child interaction therapy
- Parent screening in the primary care setting
- Social work or nurse family home visits
Pearls and Other Issues
Child abuse is a public health problem that leads to lifelong health consequences, both physically and psychologically. Physically, those who undergo abusive head trauma may have neurologic deficits, developmental delays, cerebral palsy, and other forms of disability. Psychologically, child abuse patients tend to have higher rates of depression, conduct disorder, and substance abuse. Academically, these children may have poor performance at school with decreased cognitive function.
Clinicians need to have a high index of suspicion for child maltreatment since early identification may be lifesaving. Once a child is believed to be in an abusive situation, procedures are in place under New York State Law.
Child Protective Custody
- Mandated reporters may place an alleged abused, maltreated, or neglected child in protective custody without parental consent or court order if there is imminent danger to the child's health or life.
- Individuals legally authorized to place a child in protective custody include a member of law enforcement such as a police or peace officer, a Department of Social Services employee, an agent of a duly incorporated society for cruelty prevention in children, or an individual in charge of a hospital or medical institution. The authorized individual must take the following actions based on the Family Court Act:
- As soon as possible, make a report of suspected child abuse or maltreatment and inform the court pursuant to Title 6 of the Social Services Law.
- Bring the child to a place designated by the family court unless the person is a treating clinician, and the child will be admitted to the hospital.
- Immediately notify local Child Protective Services, which shall begin a child protective proceeding in Family Court at the next regular weekday session or recommend that the child be returned to their parents or guardian.
- In neglect cases, the authorized person or entity may return a child prior to a child protective proceeding if it concluded that there is no imminent risk to the child's health.
- Make a reasonable effort to inform the individual legally responsible for the child's care of the location of the child and provide written notice of removal of the child from their care.
New York Laws and Guidelines for Reporters of Child Abuse, Maltreatment, or Neglect
Who
- Anyone may and should report if child abuse is suspected.
- Mandated reporters include:
- Coroner and medical examiner
- Daycare worker
- Director of day camp
- The district attorney or their investigators
- Foster care worker
- Health professionals (Physicians including trainees, nurses, Therapists, etc.)
- Any employee or volunteer in a residential care program for youth or any other child care or foster care worker
- Hospital personnel engaged in the admission, care, examination, or treatment.
- Police and peace officers
- Religious practitioner
- Social worker
- Substance abuse and alcoholism counselor
- Teachers and school officials
- Licensed Creative Arts Therapist
When
- *Reasonable cause to suspect abuse or maltreatment
- *Reasonable cause to suspect abuse or maltreatment if the parent or person legally responsible person for such child comes before them in their official or professional capacity and reports from personal knowledge facts, conditions, or circumstances
- Whenever a mandated reporter suspects child abuse or maltreatment while acting in their professional capacity
- *Reasonable Cause
- When a child is abused or maltreated if, considering the physical evidence, told about, or training and experience, it is possible that the injury or condition was caused by neglect or by non-accidental means.
- Certainty is not required; the reporter need only be able to entertain the possibility.
- Mandated reporters must make a report to the Statewide Central Register of Child Abuse and Maltreatment and immediately notify the person in charge of the agency, facility, institution, or school where they work or the designated agent of the person in charge that a report has been made
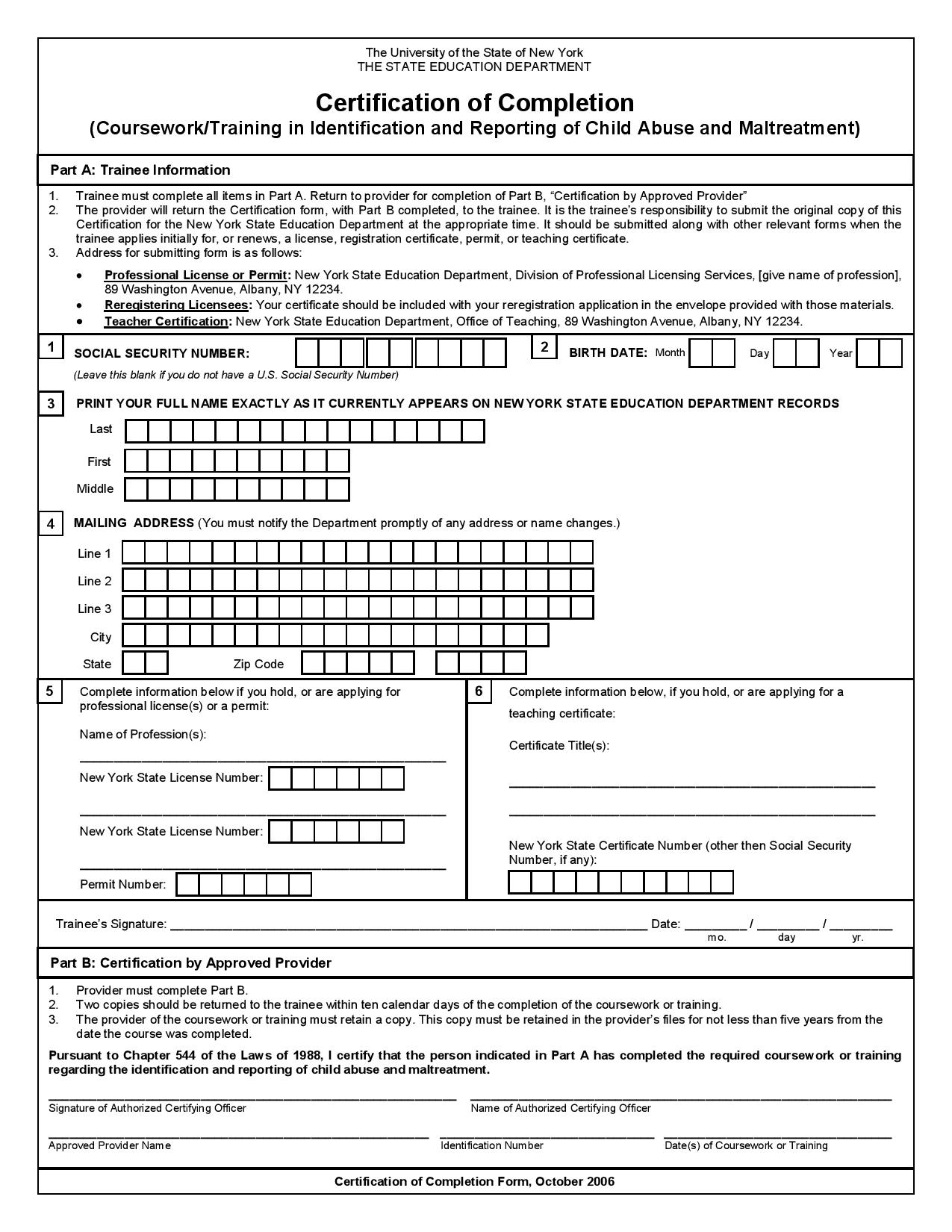
- Mandated reporters are required to make an oral telephone report immediately, and a written report must be filed within 48 hours of the oral report.
- Oral telephone reports call 800-635-1522
- Written reports are admissible as evidence in judicial proceedings and should be completed on Form LDSS-221A, signed, and filed within 48 hours to the Department of Social Services.
What
Child Protective Services will request the following information if available:
- Child
- Effect on child
- Location of victimization
- Names, addresses, age, gender, and race of the child
- Names of parents or other people responsible for the child's care
- Nature and extent of current or past injuries, abuse, maltreatment, including injuries in siblings
- Family composition
- Medications
- Need for interpreter
- Special needs
- Subject of Report
- Name, address, and contact information of the person or persons suspected of abuse, maltreatment, or injury
- The subject of the report means any parent, guardian, custodian, person 18 years of age or older, operator, employee or supervised by an authorized agency, daycare home, daycare center, the Division for Youth, the Department of Mental Hygiene who is legally responsible for a child and is allegedly responsible for causing or allowing infliction of abuse, maltreatment, or injury.
- Reporter
- Source and contact information
- Available photographs or radiographs
- Other
- Removal or keeping of the child
- Notification of the medical examiner or coroner
- Safety issues that may impact Child Protective Service investigations
- Any additional information deemed appropriate.
Once the report is made, the Department of Social Services Child Protective Services will begin an investigation within 24 hours of the report. The reporter is allowed to request the findings of their report.
Confidentiality
- The Commissioner of Social Services and the Department of Social Services are not permitted to release to the subject of a report any data that identify the person who made the report without permission of the person who made the report.
- The Health Insurance Portability and Accountability Act provisions do not affect the responsibilities of mandated reporters under New York Social Services Law.
Immunity Under Social Services Law
- To encourage prompt and complete reporting of suspected child abuse and maltreatment, any person, official, or institution that in good faith makes a report, takes photographs, or takes protective custody of a child has immunity from any liability, civil or criminal, that might result from such actions.
- All persons, officials, or institutions required to report suspected child abuse or maltreatment are presumed to have done so in good faith, providing they were done so in the discharge of their official duties and within the scope of their employment and not done so as a result from willful misconduct or gross negligence.
Failing to Report
- Any person, official, or institution required to report a case of suspected child abuse or maltreatment that willfully fails to do so can be:
- Charged with a Class A misdemeanor and subject to criminal penalties
- Sued in a civil court for monetary damages for any harm caused by such failure to report
Enhancing Healthcare Team Outcomes
Child abuse is a public health problem that leads to lifelong health consequences, both physically and psychologically. Physically, those who undergo abusive head trauma may have neurologic deficits, developmental delays, cerebral palsy, and other forms of disability. Psychologically, child abuse patients tend to have higher rates of depression, conduct disorder, and substance abuse. Academically, these children may have poor performance at school with decreased cognitive function. Clinicians need to have a high index of suspicion for child maltreatment since early identification may be lifesaving. Nurses, doctors, pharmacists, and other healthcare workers should not hesitate to report suspected child abuse.
When it comes to child abuse, all healthcare workers have a legal, medical, and moral obligation to identify the problem and report it. The majority of child abuse is identified in the Emergency Department; hence healthcare workers in the ED must be aware of the signs and symptoms of abuse. Allowing abused children to return home may lead to more violence and sometimes death. If child abuse is suspected, the social worker must be informed so that the child can be followed as an outpatient. The law favors the clinician for reporting child abuse, even if it is only a suspicion. On the other hand, failing to report child abuse can have repercussions on the clinician. Unfortunately, despite the best practices, many children continue to suffer from child abuse.[54][55][56][1][5][10][1] [Level 5]
Evidence-based Outcomes
Child abuse is a serious problem in many countries. While there is an acute awareness of the problem, many children fail to be referred or reported and consequently continue to suffer abuse, sometimes even death. In a busy emergency room, signs of child abuse may be missed; thus, healthcare workers must be vigilant of abuse in any child who presents with injuries.[3][57] [Level 5] Studies have shown that the incidence of morbidity and mortality can be decreased through prevention and treatment. The goal is to prevent abuse and neglect to allow a healthy childhood that will result in healthy adults. Society, community, and individual health providers must work together to provide a safe environment for children in New York. Reporting suspected child abuse is an obligation of all health professionals as it is an opportunity to improve a child's health, safety, and well-being. [Level 5]