Continuing Education Activity
Use of medical abbreviations in medicine is not new. Since the development of mainstream medicine nearly 200 years ago, abbreviations have been used. While initially, the abbreviations were limited to the writing of prescriptions, today, abbreviations have become very common in all aspects of medical documentation. Medical abbreviations are used in all medical and surgical departments, during surgery, the emergency room, and at discharge. One area where medical abbreviations are used most often and are a cause for concern is when writing drug orders. Until recently, the use of abbreviations has never been regulated, and there is no universal rule as to which abbreviations can be used and which ones cannot. In fact, over the past 3 decades, some healthcare workers have been making up abbreviations. The long-standing practice of writing medical abbreviation has become so entrenched in healthcare that even the most junior medical and nursing school graduates are very accustomed to writing them. In fact, many healthcare institutions have specialized lists of abbreviations that can be used. Now, with a more formalized practice of medicine, there is a concern that rampant use of medical abbreviations may pose a danger to the patient. While there are anecdotal examples of medical abbreviations that have caused harm to a few patients, good clinical evidence to support the belief that medical abbreviation use is dangerous or is causing problems in the delivery of standard of care is lacking. In any case, the potential for harm to the patient from improper communication as a result of medical abbreviations cannot be understated. This activity reviews the inappropriate use of medical abbreviations and discusses the role of the interprofessional team in avoiding acting on orders that are unclear due to the use of an abbreviation.
Objectives:
Describe the errors reported by the ISMP and Joint Commission related to inappropriate medical abbreviations.
Outline methods to avoid acting on inappropriate and unclear medical abbreviations.
Identify examples of potential harm that can result from inappropriate medical abbreviations.
Summarize the inappropriate use of medical abbreviations and highlight the role of the interprofessional team in avoiding acting on orders that are unclear due to the use of an abbreviation.
Introduction
The use of medical abbreviations in medicine is not new. Since the development of mainstream medicine nearly 200 years ago, abbreviations have been used. While initially, the abbreviations were limited to the writing of prescriptions, today, abbreviations have become very common in all aspects of medical documentation. Medical abbreviations are used in all medical and surgical departments, during surgery, in the emergency room, and at discharge. One area where medical abbreviations are used most often and are a cause for concern is when writing drug orders. Until recently, the use of abbreviations has never been regulated, and there is no universal rule as to which abbreviations can be used and which ones cannot. In fact, over the past three decades, some healthcare workers have been making up abbreviations. The long-standing practice of writing medical abbreviations has become so entrenched in healthcare that even the most junior medical and nursing school graduates are accustomed to writing them. In fact, many healthcare institutions have specialized lists of abbreviations that can be used. The use of medical abbreviations is not only an American phenomenon but a global problem.
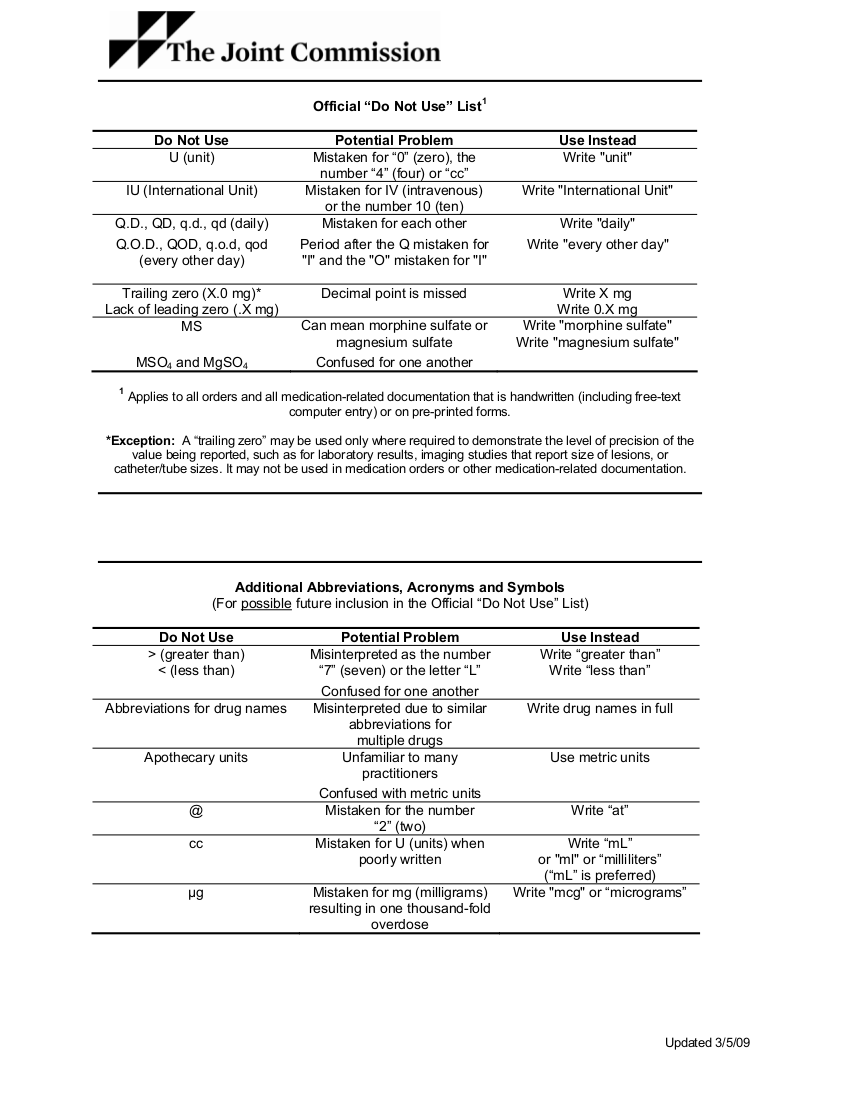
For the past three decades, healthcare leaders have been encouraging less use or even eliminating medical abbreviations in medicine. The US Institute of Safe Medication Practices (ISMP) has regularly received a continual stream of reported errors, some of which have resulted in adverse events due to misinterpretation of some dangerous medical abbreviations. The Joint Commission has regularly issued updates and regulations on the safe use of medical abbreviations and, in fact, has also published a short list of dangerous medical abbreviations and dose expressions that should never be used. However, despite many key organizations condemning the use of medical abbreviations, they continue to be used at an alarming rate. Medical abbreviations are almost routine in any medical chart or drug prescription. This can often place junior healthcare staff who are supposed to decipher the drug orders at significant risk because often the healthcare provider who writes the medical abbreviations may not be around, and the junior staff or nurse may use their limited knowledge to determine what the abbreviations exactly mean. The other alternative is to refuse to carry out any order where the abbreviations do not make sense, but this refusal can also jeopardize a patient's healthcare.
Now, with a more formalized practice of medicine, there is a concern that the rampant use of medical abbreviations may pose a danger to the patient. While there are anecdotal examples of medical abbreviations that have caused harm to a few patients, good clinical evidence to support the belief that medical abbreviation use is dangerous or is causing problems in the delivery of standard of care is lacking. In any case, the potential for harm to the patient from improper communication due to medical abbreviations cannot be understated.[1][2]
Issues of Concern
Who writes the most medical abbreviations?
The limited publications show physicians are responsible for writing the vast majority of medical abbreviations. In private practice, it is usually the physician who writes medical abbreviations, but in large teaching hospitals, the medical and surgical residents write the most medical abbreviations since they are the ones tasked with the writing of orders. However, other healthcare professionals who also regularly write medical abbreviations include dietitians, nurses, occupational and physical therapists, and social workers, albeit not in great numbers.
One of the biggest problems leading to medical errors is the failure to communicate, and this is made worse with the use of medical abbreviations, which can have multiple meanings. Further communication lapses are often the result of using medical abbreviations, especially when writing medication orders for junior staff. The staff responsible for reading, interpreting, and processing the medication order may misconstrue the abbreviation or may not even recognize it, leading to an erroneous meaning. For example, one very commonly reported misinterpretation of dosing is the use of a decimal point after a dose. For example. 5.0 is often mistaken for 50; if the dot is not seen, this can result in ten times the dose.[3]
How common is medical abbreviation usage?
The exact number of healthcare professionals who use medical abbreviations or the frequency of usage is unknown, but the numbers are numerous. Pick up any medical chart or a drug prescription in any healthcare institution, and one will see at least one abbreviation per page in the patient’s medical chart. But is the use of medical abbreviation really dangerous, and how many patients have actually suffered an adverse event because of it?
The National Medication Error Reporting program is run by the US pharmacopeia MedMarx. This program permits subscribing healthcare institutions to report and track medication errors in a standard format. From 2004 through 2006, there were 643,151 medication errors reported to MedMarx from 682 facilities, of which 4.7% (29,974) were attributed to the use of medical abbreviations.
From these data, the most common medical abbreviation error was the use of QD (once daily), accounting for 43.1% of all errors, followed by U for units, cc for ml, and other decimal errors. The most common drug abbreviation name that led to an error was the use of MS or MS04 for morphine sulfate. At least 81% of the errors were noted to occur at the time of ordering the medication, while errors at the transcribing and dispensing area occurred at a lower frequency. The administration, procurement, and monitoring processes were associated with less than 2% of the total errors. Overall, it appears that the three most common errors due to medical abbreviations were errors in prescribing, improper dose/quantity, and incorrect preparation of the medication. However, the consequences of using these medical abbreviations were not completely reported.
But irrespective of whether medical abbreviations are causing harm, no one argues that they can result in miscommunication because the other healthcare staff who are responsible for reading and processing orders may not be familiar with or even recognize these abbreviations, which can result in gross errors in dispensing or administration of a medication or a test. Several studies have looked at critical incidents and adverse events in hospitals. In many cases, it was observed that some medical abbreviations were dangerous, resulting in inappropriate dose administration or frequency.[4]
Clinical Significance
Within the past two decades, there have been many reports about medication errors, and patient safety remains a concern. It is estimated that medication errors alone account for anywhere from 7000 to 10,000 deaths annually in the United States. While medication errors have many causes, one of the ways to reduce these errors is by improving written communication, whether electronic or written. In 2004, the Joint Commission developed the "Do Not Use" list of medical abbreviations as part of the requirements for meeting the National Patient Safety Goal, which primarily addresses the effectiveness of communication between healthcare workers. The Joint Commission has also recommended that all healthcare institutions create a standard list of acronyms, abbreviations, and symbols that should not be used. However, despite the development of "Do Not Use" lists, compliance is not 100%.
Further, the Joint Commission has banned the use of medical abbreviations in documents that pertain to patient rights, informed consent forms, discharge instructions, and all other documents that a patient and the family may receive from the healthcare institution.
The Joint Commission has also recommended having a uniform and standardized list of symbols, codes, and abbreviations that can enhance communication and understanding among healthcare workers, leading to improved patient safety. Many healthcare workers have consistently reported that they have a great deal of difficulty interpreting medical abbreviations, even in their own hospitals.
To prevent any misunderstanding and jeopardize patient safety, the Joint Commission now requires healthcare institutions to develop a list of approved and not approved medical abbreviations. In addition, there should be a system or an audit process to ensure that there is compliance.
The healthcare institution must ensure that the medical abbreviation in the approved list is also not on the Do not use a list or vice versa. Further, if a medical abbreviation is permitted, then it can have only one universal meaning. For example, DOA can mean Date of Admission or Dead on Arrival.
The Joint Commission also recommends that healthcare institutions not use abbreviations on any patient-related documents. It is important to ensure that the patient and the family can understand the information provided to them without having to guess. Often patients have difficulty understanding discharge instructions, which can affect their ability to look after themselves or follow instructions.
The information in the discharge instructions must be clear and unambiguous; many times, the patient may feel embarrassed to ask questions about abbreviations, and this can impact the quality of care.
Sometimes laboratory results are sent to the patient, but this information often contains abbreviations. Whenever test results are provided to the patient, the healthcare provider should make a concerted effort to explain the results to the patient. While the use of imaging test names like CT and MRI are often abbreviated, it is essential for the healthcare provider to spell out other not well-known tests; for example, instead of "BE," the patient should be told "BE" means a barium enema.
How can healthcare institutions reduce or eliminate medical abbreviation usage?
Today some hospitals recommend that junior staff refuse to carry out orders that use medical abbreviations. In addition, physicians who write medical abbreviations are reprimanded. However, instead of enforcing authoritarian rules, the tide has now turned towards using more intensive and focused educational strategies to increase compliance with hospital rules (Abushaiqa et al., 2007). To encourage compliance, the following education interventions may help reduce medical abbreviations.
- Describe the abbreviation and provide a rationale for why and how it can lead to an error
- When an abbreviation is encountered, speak to the healthcare provider
- Teach junior staff and students about the dangers of using medical abbreviations
- Develop a list of prohibited medical abbreviations and post them on every medical floor
- If a medical abbreviation is to be used, then provide the dose designation and correct terminology
- Develop a list of medication abbreviations that can pose a risk to patient safety
- Develop posters and stickers on prohibited medical abbreviations that can be placed on medical charts, medicine cabinets, order sheets, and in the pharmacy
- Have regular in-service education sessions for physicians, nursing staff, pharmacists, and other healthcare professionals
- Perform regular audits on the charts to determine who is still using medical abbreviations and what is the frequency
- Develop a system where nursing and other healthcare staff report the use of medical abbreviations by other staff. This is not meant to be as a whistleblower, but to identify the individual and punish them and to educate them about the dangers of medical abbreviation.[5][6][7]
Other Issues
Formation of a Hospital Committee
Most hospitals have now developed a committee that oversees the use of medical abbreviations. The committee is in charge of implementing a list of prohibited abbreviations. The committee usually consists of a physician, nurse, pharmacist, and personnel from risk management and patient safety (Traynor, 2004). This committee is also tasked with the role of performing chart audits to ensure that healthcare workers are compliant. The committee should also set policies for those who do not comply. One of the means may include ceasing order writing privileges for repeat offenders. Finally, the committee should encourage all staff to report other healthcare staff who continue to write medical abbreviations (Cowell, 2007).
Discussion
The use of medication abbreviation has persisted in healthcare despite recommendations by the Joint Commission that such usage may adversely affect patient care. Most serious medication abbreviations are written while writing drug orders, and the junior staff is often left with the responsibility of understanding and deciphering the abbreviation. With the wide adoption of electronic technology, these medical abbreviations are often repeated in the medical chart and continue to pose a threat to patient safety. All healthcare institutions have now started to formulate guidelines restricting the use of medical abbreviations. While few studies have quantified the extent of medical abbreviation usage and its adverse effects, the Joint Commission feels that the problem is widespread and has the potential to cause severe patient harm. Thus, the Joint Commission has released a list of prohibited medical abbreviations for all healthcare institutions. One way to reduce the use of medical abbreviations will be through continuous reporting and education of healthcare workers. But on rare occasions, enforcement by limiting ordering privileges may be necessary. Although the risk of actual patient harm from using medical abbreviations is low, the aim is to achieve zero risk.
Pearls of Wisdom
To minimize the use of medical abbreviations, the following guidelines are recommended:
- Develop a regular campaign to erase the use of medical abbreviations in your institution completely
- Develop a committee to oversee and regulate the use of medical abbreviations
- Create a list of "do not use" abbreviations and post them on medical and surgical floors, patient charts, pharmacies, computer screens, intranet sites, hospital newsletters, and healthcare lounges.
- Initiate educational programs for all staff on the dangers of using abbreviations
- Reward healthcare staff who are compliant
- Minimize the use of abbreviations even at conferences, seminars, and lectures- practice what you preach
- Ensure that all drug names, dosages, and frequencies are spelled out
- Prohibit the use of medical abbreviations on all patient charts, discharge forms, consent forms, and prescriptions
- Encourage junior staff to communicate with senior staff who write the abbreviations before carrying out the order
- Encourage junior staff to report staff who regularly use abbreviations
- Perform regular audits to check for compliance
- Circulate Joint Commission guidelines on the use of medical abbreviation usage
- For repeat offenders, remove privileges to write to orders[7][8][9]
Enhancing Healthcare Team Outcomes
The Joint Commission
The Joint Commission strongly believes that completely removing dangerous medical abbreviations is a far better option than healthcare institutions undertaking secondary measures like quality control or restricting the use of only certain abbreviations. In many hospitals, many prescriptions written by clinicians have to be clarified and/or corrected by pharmacists to prevent errors. To avoid this type of recurrence, the rule should be that no prescription should have any medical abbreviations. Nurses should ask healthcare workers to rewrite orders that contain abbreviations. All interprofessional healthcare team members should be on the same page regarding the non-use of medical abbreviations.
Other remedies to counter medical abbreviation usage include education, a reward for non-usage, accountability for habitual offenders, and education. The healthcare staff who continue to use medical abbreviations need to be identified and cautioned. This applies to all clinical staff, including physicians, pharmacists, and nursing. Furthermore, the use of stickers and posters on the dangers of medical abbreviations should be posted on the chart and the nursing floors. Sometimes education may not be adequate to change the writing habits of certain healthcare professionals. In such cases, these individuals may have to be reprimanded, or their ordering privileges be suspended.