Introduction
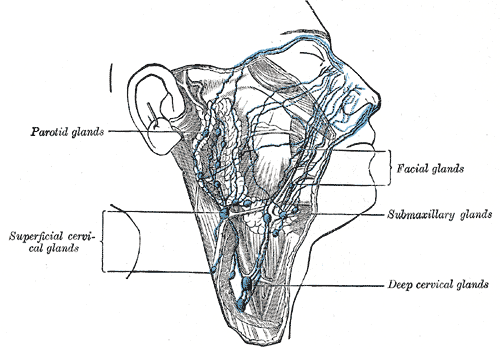
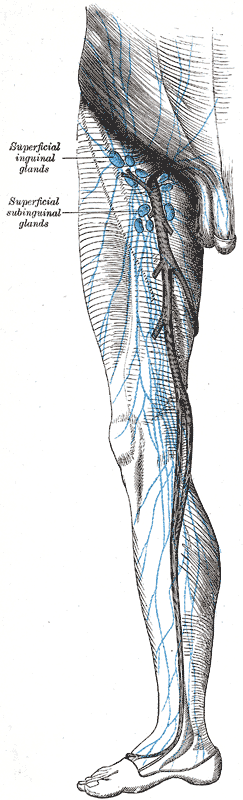
The lymphatic system, or lymphoid system, is one of the components of the circulatory system, and it serves a critical role in both immune function and surplus extracellular fluid drainage. Components of the lymphatic system include lymph, lymphatic vessels and plexuses, lymph nodes, lymphatic cells, and a variety of lymphoid organs. The pattern and form of lymphatic channels are more variable and complex but generally parallel those of the peripheral vascular system. The lymphatic system partly functions to convey lymphatic fluid, or lymph, through a network of lymphatic channels, filter lymphatic fluid through lymph nodes and return lymphatic fluid to the bloodstream, where it is eventually eliminated. Nearly all body organs, regions, and systems have lymphatic channels to collect the various byproducts that require elimination. Liver and intestinal lymphatics produce about 80% of the volume of lymph in the body.[1]
Notable territories of the body that do not appear to contain lymphatics include the bone marrow, epidermis, as well as other tissues where blood vessels are absent. The central nervous system was long considered to be absent of lymphatic vessels until they were recently identified in the cranial meninges.[2][3] Moreover, a vessel appearing to have lymphatic features was also discovered in the eye.[4][5] The lymphatic system is critical in a clinical context, particularly given that it is a major route for cancer metastasis and that the inflammation of lymphatic vessels and lymph nodes is an indicator of pathology.
The lymphatic system includes numerous structural components, including lymphatic capillaries, afferent lymphatic vessels, lymph nodes, efferent lymphatic vessels, and various lymphoid organs.
Lymphatic capillaries are tiny, thin-walled vessels that originate blindly within the extracellular space of various tissues. Lymphatic capillaries tend to be larger in diameter than blood capillaries and are interspersed among them to enhance their ability to collect interstitial fluid efficiently. They are critical in the drainage of extracellular fluid and allow this fluid to enter the closed capillaries but not exit due to their unique morphology. Lymphatic capillaries at their blind ends are composed of a thin endothelium without a basement membrane. The endothelial cells at the closed end of the capillary overlap but shift to open the capillary end when interstitial fluid pressure is greater than intra-capillary pressure. This process permits lymphocytes, interstitial fluid, bacteria, cellular debris, plasma proteins, and other cells to enter the lymphatic capillaries. Special lymphatic capillaries called lacteals exist in the small intestine to contribute to the absorption of dietary fats. Lymphatics in the liver contribute to a specialized role in transporting hepatic proteins into the bloodstream.[1] The lymphatic capillaries of the body form large networks of channels called lymphatic plexuses and converge to form larger lymphatic vessels.
Lymphatic vessels convey lymph, or lymphatic fluid, through their channels. Afferent (toward) lymphatic vessels convey unfiltered lymphatic fluid from the body tissues to the lymph nodes, and efferent (away) lymphatic vessels convey filtered lymphatic fluid from lymph nodes to subsequent lymph nodes or into the venous system. The various efferent lymphatic vessels in the body eventually converge to form two major lymphatic channels: the right lymphatic duct and the thoracic duct.
The right lymphatic duct drains most of the right upper quadrant of the body, including the right upper trunk, right upper extremity, and right head and neck. The right lymphatic trunk is a visible channel in the right cervical region just anterior to the anterior scalene muscle. Its origin and termination are variable in morphology, typically forming as the convergence of the right bronchomediastinal, jugular, and subclavian trunks, extending 1 to 2 centimeters in length before returning its contents to the systemic circulation at the junction of the right internal jugular, subclavian, and/or brachiocephalic veins.
The thoracic duct, also known as the left lymphatic duct or van Hoorne's canal, is the largest of the body's lymphatic channels. It drains most of the body except for the territory of the right superior thorax, head, neck, and upper extremity served by the right lymphatic duct. The thoracic duct is a thin-walled tubular vessel measuring 2 to 6 mm in diameter. The length of the duct ranges from 36 to 45 cm. The thoracic duct is highly variable in form but typically arises in the abdomen at the superior aspect of the cisterna chyli, around the level of the twelfth thoracic vertebra (T12). The cisterna chyli, from which it extends, is an expanded lymphatic sac that forms at the convergence of the intestinal and lumbar lymphatic trunks extending along the L1-L2 vertebral levels. The cisterna chyli is present in approximately 40-60% of the population, and in its absence, the intestinal and lumbar lymphatic trunks communicate directly with the thoracic duct at the T12 level.[6][7]
As a result, the thoracic duct receives lymphatic fluid from the lumbar lymphatic trunks and chyle, composed of lymphatic fluid and emulsified fats, from the intestinal lymphatic trunk. Initially, the thoracic duct is located just to the right of the midline and posterior to the aorta. It exits the abdomen and enters the thorax via the aortic hiatus formed by the right and left crura of the diaphragm, side by side with the aorta. The thoracic duct then ascends in the thoracic cavity just anterior and to the right of the vertebral column between the aorta and azygous vein. At about the level of the fifth thoracic vertebra (T5), the thoracic duct typically crosses to the left of the vertebral column and posterior to the esophagus. From here, it ascends vertically and usually empties its contents into the junction of the left subclavian and left internal jugular veins in the cervical region.
To ensure that lymph does not flow backward, collecting lymphatic vessels and larger lymphatic vessels have one-way valves. These valves are not present in the lymphatic capillaries. These lymphatic valves permit the continued advancement of lymph through the lymphatic vessels aided by a pressure gradient created by vascular smooth muscle, skeletal muscle contraction, and respiratory movements. However, it is important to note that lymphatic vessels also communicate with the venous system through various anastomoses.
Lymph nodes are small bean-shaped tissues situated along lymphatic vessels. Lymph nodes receive lymphatic fluid from afferent lymphatic vessels and convey lymph away through efferent lymphatic vessels. Lymph nodes serve as a filter and function to monitor lymphatic fluid/blood composition, drain excess tissue fluid and leaked plasma proteins, engulf pathogens, augment an immune response, and eradicate infection.
Several organs in the body are considered to be lymphoid or lymphatic organs, given their role in the production of lymphocytes. These include the bone marrow, spleen, thymus, tonsils, lymph nodes, and other tissues. Lymphoid organs can be categorized as primary or secondary lymphoid organs. Primary lymphoid organs are those that produce lymphocytes, such as the bone marrow and thymus. Bone marrow is the primary site for the production of lymphocytes. The thymus is a glandular organ located anterior to the pericardium. It serves to mature and develop T cells, or thymus cell lymphocytes, in response to an inflammatory process or pathology. As individuals age, both their bone marrow and thymus reduce and accumulate fat. Secondary lymphoid organs serve as territories in which immune cells function and include the spleen, tonsils, lymph nodes, and various mucous membranes, such as in the intestines. The spleen is a purplish, fist-sized organ in the left upper abdominal quadrant that contributes to immune function by serving as a blood filter, storing lymphocytes within its white pulp, and being a site for an adaptive immune response to antigens. The lingual tonsils, palatine tonsils, and pharyngeal tonsils, or adenoids, work to prevent pathogens from entering the body. Mucous membranes in the gastrointestinal, respiratory, and genitourinary systems also function to prevent pathogens from entering the body.
Lymphatic fluid, or lymph, is similar to blood plasma and tends to be watery, transparent, and yellowish in appearance. Extracellular fluid leaks out of the blood capillary walls because of pressure exerted by the heart or osmotic pressure at the cellular level. As the interstitial fluid accumulates, it is picked up by the tiny lymphatic capillaries along with other substances to form lymph. This fluid then passes through the lymphatic vessels and lymph nodes and finally enters the venous circulation. As the lymph passes through the lymph nodes, both monocytes and lymphocytes enter it.
Lymph is composed primarily of interstitial fluid with variable amounts of lymphocytes, bacteria, cellular debris, plasma proteins, and other cells. In the GI tract, lymphatic fluid is called chyle and has a milk-like appearance that is chiefly due to the presence of cholesterol, glycerol, fatty acids, and other fat products. The vessels that transport the lymphatic fluid from the GI tract are known as lacteals.
The development of the lymphatic system is known from both human and animal, especially mouse studies. The lymphatic vessels form after the development of blood vessels, around six weeks post-fertilization. The endothelial cells that serve as precursors to the lymphatics arise from the embryonic cardinal veins.[8] The process by which lymphatic vessels form is similar to that of the blood vessels and produces lymphatic-venous and intra-lymphatic anastomoses, but diverse origins exist for components of lymphatic vessel formation in different regions.[9][10][11][12]
Six primary lymph sacs develop and are apparent about eight weeks post-fertilization. These include, from caudal to cranial, one cisterna chyli, one retroperitoneal lymph sac, two iliac lymph sacs, and two jugular lymph sacs. The jugular lymph sacs are the first to develop, initially appearing next to the jugular part of the cardinal vein.[12] Lymphatic vessels then form adjacent to the blood vessels and connect the various lymph sacs. The lymphatic vessels primarily arise from the lymph sacs through the process of self-proliferation and polarized sprouting.[13]
Stem/progenitor cells play a huge role in forming lymphatic tissues and vessels by contributing to sustained growth and postnatally differentiating into lymphatic endothelial cells.[13] Lymphatic channels from the developing gut connect with the retroperitoneal lymph sac and the cisterna chyli, situated just posteriorly. The lymphatic channels of the lower extremities and inferior trunk communicate with the iliac lymph sacs. Finally, lymphatic channels in the head, neck and upper extremities drain to the jugular lymph sacs. Additionally, a right and left thoracic duct form and connect the cisterna chyli with the jugular lymph sacs and form anastomoses that eventually produce the typical adult form. The lymph sacs then produce groups of lymph nodes in the fetal period. Migrating mesenchyme enters the lymph sacs and produces lymphatic networks, connective tissue, and other layers of the lymph nodes.