[1]
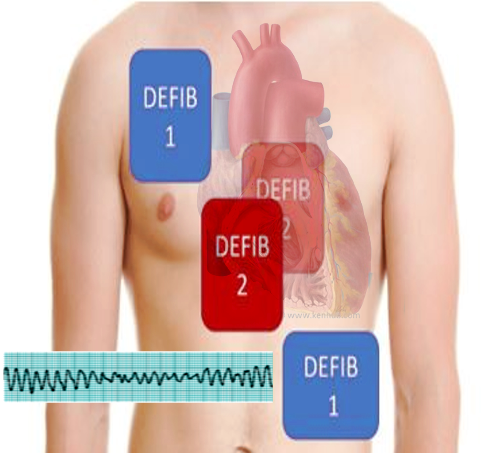
Hoch DH, Batsford WP, Greenberg SM, McPherson CM, Rosenfeld LE, Marieb M, Levine JH. Double sequential external shocks for refractory ventricular fibrillation. Journal of the American College of Cardiology. 1994 Apr:23(5):1141-5
[PubMed PMID: 8144780]
[2]
Eifling M, Razavi M, Massumi A. The evaluation and management of electrical storm. Texas Heart Institute journal. 2011:38(2):111-21
[PubMed PMID: 21494516]
[3]
Sakai T, Iwami T, Tasaki O, Kawamura T, Hayashi Y, Rinka H, Ohishi Y, Mohri T, Kishimoto M, Nishiuchi T, Kajino K, Matsumoto H, Uejima T, Nitta M, Shiokawa C, Ikeuchi H, Hiraide A, Sugimoto H, Kuwagata Y. Incidence and outcomes of out-of-hospital cardiac arrest with shock-resistant ventricular fibrillation: Data from a large population-based cohort. Resuscitation. 2010 Aug:81(8):956-61
[PubMed PMID: 20653086]
[4]
Sarkozy A, Dorian P. Strategies for reversing shock-resistant ventricular fibrillation. Current opinion in critical care. 2003 Jun:9(3):189-93
[PubMed PMID: 12771668]
Level 3 (low-level) evidence
[5]
Dorian P, Cass D, Schwartz B, Cooper R, Gelaznikas R, Barr A. Amiodarone as compared with lidocaine for shock-resistant ventricular fibrillation. The New England journal of medicine. 2002 Mar 21:346(12):884-90
[PubMed PMID: 11907287]
[6]
Windecker S. Percutaneous left ventricular assist devices for treatment of patients with cardiogenic shock. Current opinion in critical care. 2007 Oct:13(5):521-7
[PubMed PMID: 17762230]
Level 3 (low-level) evidence
[7]
Herlitz J,Bång A,Holmberg M,Axelsson A,Lindkvist J,Holmberg S, Rhythm changes during resuscitation from ventricular fibrillation in relation to delay until defibrillation, number of shocks delivered and survival. Resuscitation. 1997 Feb;
[PubMed PMID: 9051819]
[8]
Leacock BW. Double simultaneous defibrillators for refractory ventricular fibrillation. The Journal of emergency medicine. 2014 Apr:46(4):472-4. doi: 10.1016/j.jemermed.2013.09.022. Epub 2014 Jan 21
[PubMed PMID: 24462025]
[9]
Stiell IG, Walker RG, Nesbitt LP, Chapman FW, Cousineau D, Christenson J, Bradford P, Sookram S, Berringer R, Lank P, Wells GA. BIPHASIC Trial: a randomized comparison of fixed lower versus escalating higher energy levels for defibrillation in out-of-hospital cardiac arrest. Circulation. 2007 Mar 27:115(12):1511-7
[PubMed PMID: 17353443]
Level 1 (high-level) evidence
[10]
Koster RW, Walker RG, Chapman FW. Recurrent ventricular fibrillation during advanced life support care of patients with prehospital cardiac arrest. Resuscitation. 2008 Sep:78(3):252-7. doi: 10.1016/j.resuscitation.2008.03.231. Epub 2008 Jun 16
[PubMed PMID: 18556106]
[11]
Walsh SJ, McClelland AJ, Owens CG, Allen J, Anderson JM, Turner C, Adgey AA. Efficacy of distinct energy delivery protocols comparing two biphasic defibrillators for cardiac arrest. The American journal of cardiology. 2004 Aug 1:94(3):378-80
[PubMed PMID: 15276112]
[12]
Morgan JP, Hearne SF, Raizes GS, White RD, Giuliani ER. High-energy versus low-energy defibrillation: experience in patients (excluding those in the intensive care unit) at Mayo Clinic-affiliated hospitals. Mayo Clinic proceedings. 1984 Dec:59(12):829-34
[PubMed PMID: 6503363]
[13]
Chen B, Yin C, Ristagno G, Quan W, Tan Q, Freeman G, Li Y. Retrospective evaluation of current-based impedance compensation defibrillation in out-of-hospital cardiac arrest. Resuscitation. 2013 May:84(5):580-5. doi: 10.1016/j.resuscitation.2012.09.017. Epub 2012 Sep 20
[PubMed PMID: 23000364]
Level 2 (mid-level) evidence
[14]
White RD, Blackwell TH, Russell JK, Jorgenson DB. Body weight does not affect defibrillation, resuscitation, or survival in patients with out-of-hospital cardiac arrest treated with a nonescalating biphasic waveform defibrillator. Critical care medicine. 2004 Sep:32(9 Suppl):S387-92
[PubMed PMID: 15508666]
[15]
Pourmand A, Galvis J, Yamane D. The controversial role of dual sequential defibrillation in shockable cardiac arrest. The American journal of emergency medicine. 2018 Sep:36(9):1674-1679. doi: 10.1016/j.ajem.2018.05.078. Epub 2018 Jun 1
[PubMed PMID: 29880409]
[16]
Cabañas JG, Myers JB, Williams JG, De Maio VJ, Bachman MW. Double Sequential External Defibrillation in Out-of-Hospital Refractory Ventricular Fibrillation: A Report of Ten Cases. Prehospital emergency care. 2015 January-March:19(1):126-130
[PubMed PMID: 25243771]
Level 3 (low-level) evidence
[17]
Cortez E, Krebs W, Davis J, Keseg DP, Panchal AR. Use of double sequential external defibrillation for refractory ventricular fibrillation during out-of-hospital cardiac arrest. Resuscitation. 2016 Nov:108():82-86. doi: 10.1016/j.resuscitation.2016.08.002. Epub 2016 Aug 10
[PubMed PMID: 27521470]
[18]
El Tawil C, Mrad S, Khishfe BF. Double sequential defibrillation for refractory ventricular fibrillation. The American journal of emergency medicine. 2017 Dec:35(12):1985.e3-1985.e4. doi: 10.1016/j.ajem.2017.09.009. Epub 2017 Sep 8
[PubMed PMID: 28978402]
[19]
Hajjar K, Berbari I, El Tawil C, Bou Chebl R, Abou Dagher G. Dual defibrillation in patients with refractory ventricular fibrillation. The American journal of emergency medicine. 2018 Aug:36(8):1474-1479. doi: 10.1016/j.ajem.2018.04.060. Epub 2018 Apr 30
[PubMed PMID: 29730094]