[1]
Farzaneh MR, Jamshidiha F, Kowsarian S. Inhalational lung disease. The international journal of occupational and environmental medicine. 2010 Jan:1(1):11-20
[PubMed PMID: 23022777]
[2]
Xie M, Liu X, Cao X, Guo M, Li X. Trends in prevalence and incidence of chronic respiratory diseases from 1990 to 2017. Respiratory research. 2020 Feb 11:21(1):49. doi: 10.1186/s12931-020-1291-8. Epub 2020 Feb 11
[PubMed PMID: 32046720]
[3]
Furuya S, Chimed-Ochir O, Takahashi K, David A, Takala J. Global Asbestos Disaster. International journal of environmental research and public health. 2018 May 16:15(5):. doi: 10.3390/ijerph15051000. Epub 2018 May 16
[PubMed PMID: 29772681]
[4]
Cullinan P, Reid P. Pneumoconiosis. Primary care respiratory journal : journal of the General Practice Airways Group. 2013 Jun:22(2):249-52. doi: 10.4104/pcrj.2013.00055. Epub
[PubMed PMID: 23708110]
[5]
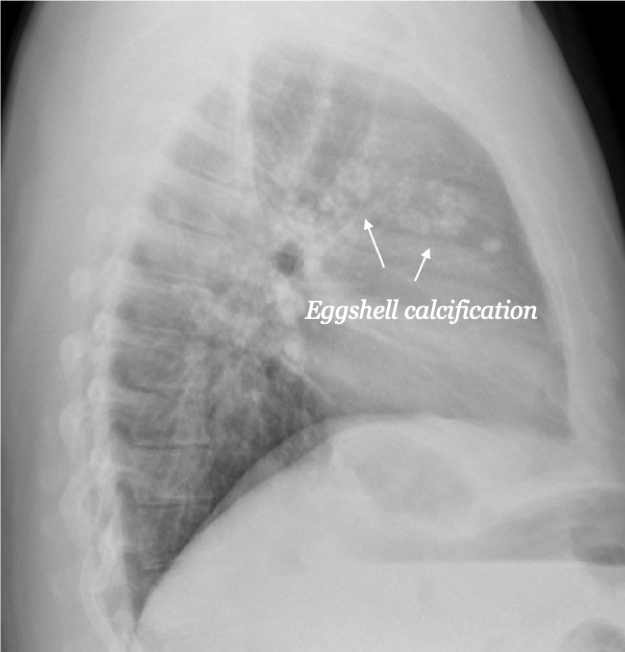
Chong S, Lee KS, Chung MJ, Han J, Kwon OJ, Kim TS. Pneumoconiosis: comparison of imaging and pathologic findings. Radiographics : a review publication of the Radiological Society of North America, Inc. 2006 Jan-Feb:26(1):59-77
[PubMed PMID: 16418244]
[6]
Perlman DM, Maier LA. Occupational Lung Disease. The Medical clinics of North America. 2019 May:103(3):535-548. doi: 10.1016/j.mcna.2018.12.012. Epub 2019 Mar 7
[PubMed PMID: 30955520]
[7]
Campbell H, Lyons JP, Gough J, Ryder R. Coalworkers' pneumoconiosis. British medical journal. 1973 Aug 11:3(5875):351
[PubMed PMID: 4723827]
[8]
Cohen RA, Petsonk EL, Rose C, Young B, Regier M, Najmuddin A, Abraham JL, Churg A, Green FH. Lung Pathology in U.S. Coal Workers with Rapidly Progressive Pneumoconiosis Implicates Silica and Silicates. American journal of respiratory and critical care medicine. 2016 Mar 15:193(6):673-80. doi: 10.1164/rccm.201505-1014OC. Epub
[PubMed PMID: 26513613]
[9]
Fujimura N. Pathology and pathophysiology of pneumoconiosis. Current opinion in pulmonary medicine. 2000 Mar:6(2):140-4
[PubMed PMID: 10741774]
Level 3 (low-level) evidence
[10]
Yang HY. Prediction of pneumoconiosis by serum and urinary biomarkers in workers exposed to asbestos-contaminated minerals. PloS one. 2019:14(4):e0214808. doi: 10.1371/journal.pone.0214808. Epub 2019 Apr 4
[PubMed PMID: 30946771]
[11]
Yang HY, Wang JD, Chen PC, Lee JJ. Pleural plaque related to asbestos mining in Taiwan. Journal of the Formosan Medical Association = Taiwan yi zhi. 2010 Dec:109(12):928-33. doi: 10.1016/S0929-6646(10)60142-8. Epub
[PubMed PMID: 21195893]
[12]
Perret JL, Plush B, Lachapelle P, Hinks TS, Walter C, Clarke P, Irving L, Brady P, Dharmage SC, Stewart A. Coal mine dust lung disease in the modern era. Respirology (Carlton, Vic.). 2017 May:22(4):662-670. doi: 10.1111/resp.13034. Epub 2017 Mar 30
[PubMed PMID: 28370783]
[13]
Li J, Yao W, Hou JY, Zhang L, Bao L, Chen HT, Wang D, Yue ZZ, Li YP, Zhang M, Yu XH, Zhang JH, Qu YQ, Hao CF. The Role of Fibrocyte in the Pathogenesis of Silicosis. Biomedical and environmental sciences : BES. 2018 Apr:31(4):311-316. doi: 10.3967/bes2018.040. Epub
[PubMed PMID: 29773095]
[14]
McBean R, Tatkovic A, Edwards R, Newbigin K. What does coal mine dust lung disease look like? A radiological review following re-identification in Queensland. Journal of medical imaging and radiation oncology. 2020 Apr:64(2):229-235. doi: 10.1111/1754-9485.13007. Epub 2020 Feb 11
[PubMed PMID: 32048474]
[16]
Li J, Liang C, Zhang ZK, Pan X, Peng S, Lee WS, Lu A, Lin Z, Zhang G, Leung WN, Zhang BT. TAK1 inhibition attenuates both inflammation and fibrosis in experimental pneumoconiosis. Cell discovery. 2017:3():17023. doi: 10.1038/celldisc.2017.23. Epub 2017 Jul 11
[PubMed PMID: 28698801]
[17]
Tsang EW, Kwok H, Chan AKY, Choo KL, Chan KS, Lau KS, Chan CCH. Outcomes of community-based and home-based pulmonary rehabilitation for pneumoconiosis patients: a retrospective study. BMC pulmonary medicine. 2018 Aug 9:18(1):133. doi: 10.1186/s12890-018-0692-7. Epub 2018 Aug 9
[PubMed PMID: 30092783]
Level 2 (mid-level) evidence
[18]
Laney AS, Weissman DN. Respiratory diseases caused by coal mine dust. Journal of occupational and environmental medicine. 2014 Oct:56 Suppl 10(0 10):S18-22. doi: 10.1097/JOM.0000000000000260. Epub
[PubMed PMID: 25285970]