Continuing Education Activity
Molluscum contagiosum, also called water warts, is a benign condition of the skin. The skin lesions of molluscum contagiosum are called mollusca. The typical lesion appears dome-shaped, round, and pinkish-purple in color. This activity reviews the cause and presentation of molluscum contagiosum and highlights the role of the interprofessional team in its management.
Objectives:
- Explain the cause of molluscum contagiosum.
- Describe the appearance of molluscum contagiosum.
- Outline the treatment of molluscum contagiosum.
- Review the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by molluscum contagiosum.
Introduction
Molluscum contagiosum, also called water warts, is a benign condition of the skin. The skin lesions of molluscum contagiosum are called mollusca. The typical lesion appears dome-shaped, round, and pinkish-purple in color.[1][2][3]
Etiology
A double-stranded DNA poxvirus called molluscum contagiosum virus (MCV) causes molluscum contagiosum. Four subtypes of the molluscum contagiosum virus are known, and the are MCV-1 (98% of cases) is mostly seen in children, while MCV-2 is mainly responsible for skin lesions in people living with HIV. MCV-3 and MCV-4 are present in Asia and Australia. Currently, it is not possible to have cultures of molluscum contagiosum virus.
Molluscum contagiosum lesions are transmitted by direct skin-to-skin (including sexual) or indirect (towels, underclothes, toys, razor, tattoo supplies) contact. Molluscum contagiosum may also disseminate by autoinoculation to normal skin after mollusca scraping by the patients. Transmission from sharing swimming pools and other wet environments is possible but not fully proven. In utero and prepartum transmissions are occasionally reported, resulting in congenital molluscum contagiosum or skin lesions developing during the early months of life.[4][5]
Epidemiology
Molluscum contagiosum is a common medical concern. In 2010, there were about 122 million cases. It occurs worldwide but seems to be more frequent in warm, humid regions. Molluscum contagiosum is diagnosed mainly in children aged two to five years, but also in sexually active teenagers and adults, and immunocompromised persons. Atopic dermatitis may increase the risk of developing molluscum contagiosum since it alters the skin barrier and immunity function. In people living with HIV (human immunodeficiency virus), the clinical prevalence of molluscum contagiosum may reach up to 18%. No gender predominance is noted.[6]
Pathophysiology
The incubation period ranges from two weeks to six months. Molluscum contagiosum virus infects only keratinocytes, and skin lesions are limited to the epidermis and do not have systemic dissemination. Molluscum contagiosum virus produces proteins inhibiting human antiviral immunity, thus preventing the development of innate immunity response, and contributing to the persistence of skin lesions.[7]
Histopathology
Molluscum contagiosum lesions have classic features under a microscope. The cup-shaped indentation of the epidermis into the dermis is usually seen. The proliferated rete ridges descend downwards and encircle the dermis. The epidermis is usually thickened and there is the presence of Henderson-Paterson bodies seen within the epidermis. It is these bodies that enclose the virus particles.
History and Physical
Molluscum contagiosum causes mainly cosmetic concerns. Mollusca is usually asymptomatic but may be painful or itchy. In atopic persons, eczema lesions may develop around mollusca weeks after their occurrence. An inflammatory reaction, secondary to scratching or occurring when mollusca start to resolve, is frequent and should be distinguished from secondary bacterial infection. When scratched or removed, molluscum contagiosum can lead to bleeding under every single element.
Evaluation
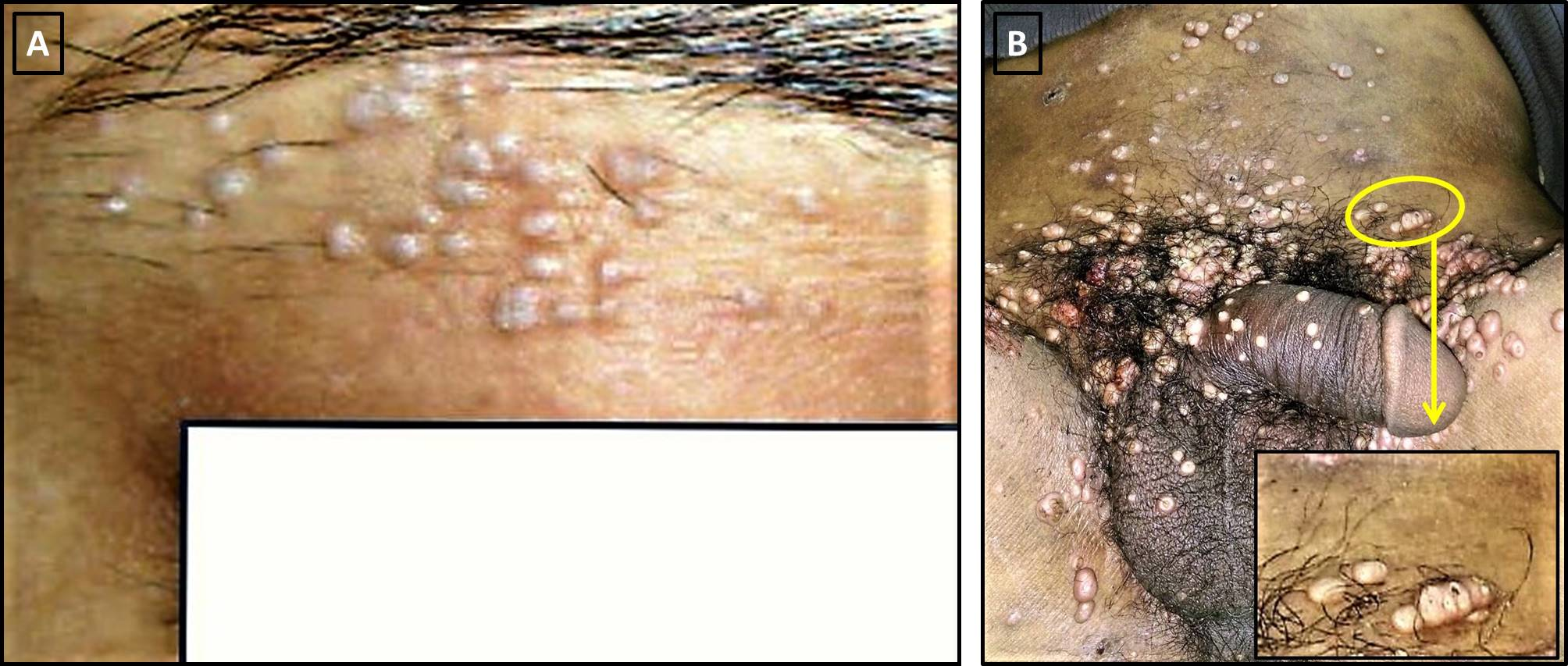
The diagnosis of molluscum contagiosum is based on clinical examination. Lesions are firm, white to flesh-colored, dome-shaped, pearly papules, having a central umbilication from which one can express a cheesy material. Mollusca is usually one millimeter to one centimeter in diameter.[8][9]
In children, mollusca are located on the face, trunk, limbs, and axillary areas. Palms and soles are not involved. In sexually transmitted forms, lesions are mainly observed in the anogenital area, abdomen, and inner thighs. There are rarely more than 20 to 30 elements over the skin and are usually grouped together. However, molluscum contagiosum may be extensive, mostly in immunocompromised persons.
The differential diagnosis of molluscum contagiosum in children includes syringoma, closed comedones (whiteheads), and warts (including anogenital ones).
In immunocompromised persons, molluscum contagiosum lesions may be atypical, have a greater size, and/or mimic malignancies, such as basal cell carcinoma or keratoacanthoma (for single lesions), or other infectious diseases, such as cryptococcosis and histoplasmosis (for extensive lesions).
In the case of a diagnosis difficulty, dermoscopy, reflectance confocal microscopy, and histopathology may be useful.
Dermoscopy of a molluscum shows a central white to a yellow amorphous area, with peripheral linear or branched vessels.
Reflectance confocal microscopy also shows a well-defined central area, which contains septa separating hypo-refractive roundish lobules. Histopathologically, these lobules consist of enlarged keratinocytes having an abundant cytoplasm containing viral inclusions (also called Henderson Paterson bodies) and a peripheral nucleus. The nearby epidermis shows marked acanthosis.
Treatment / Management
People frequently seek treatment for cosmetic reasons, to avoid social stigma, or because they have concerns of transmission to other individuals. The treatment depends on the patient’s (or their parent's) preferences. Because the condition is usually self-limiting, awaiting spontaneous resolution should be considered. However, the patients should be aware that the resolution of molluscum contagiosum may take several months. Even though many treatments had been proposed for molluscum contagiosum, none has proven its effectiveness. Current treatment options include physical removal of mollusca, topical medications, and systemic treatment.[10][11][12]
Physical removal is based mainly on cryotherapy with liquid nitrogen or curettage. Techniques might be associated. Laser treatment (carbon dioxide or pulsed dye laser) may also be used but not as first-line therapy. Physical removal is usually painful and may require local anesthesia. Postoperative scarring is possible. Topical trichloroacetic acid can be used to treat mollusca with minimal scarring.
Doctors recommend many topical treatments for molluscum contagiosum. Podophyllotoxin (contraindicated in pregnant women), potassium hydroxide, salicylic acid (associated or not with povidone-iodine), benzoyl peroxide, and tretinoin are used as home treatments and must be applied to each lesion. They are used with the aim to induce an inflammatory reaction, thus accelerating recovery. In a recent analysis, imiquimod, which is used as a modulator of the immune system, and cantharidin, a blistering topical applied by the physician, has not been found to be more effective than other vehicles.
The use of oral cimetidine has been described as a safe alternative to physical removal in children who fear pain (except for facial involvement). However, a recent meta-analysis did not show any difference with cimetidine. Cidofovir, a DNA polymerase inhibitor, has been used successfully in immunosuppressed persons, but it may induce nephrotoxicity and neutropenia when used intravenously. In people living with HIV/AIDS, molluscum contagiosum is best managed with highly active antiretroviral therapy (HAART).
Differential Diagnosis
- Keratoacanthoma
- Lichen planus
- Epidermal cyst
- Pyoderma
- Verruca vulgaris
- Folliculitis
- Cutaneous fungal disorders like histoplasmosis and sporotrichosis
- Basal cell cancer
- Condyloma acuminatum
- Varicella-zoster
Complications
- Inflammation or infection (cellulitis)
- Irritation
- Conjunctivitis if the lesions are on the eyelids
- Abscess
Pearls and Other Issues
Most molluscum contagiosum lesions in non-compromised persons resolve spontaneously within an average duration of six to 12 months. However, the course of molluscum contagiosum may take as long as four years. During that period, some mollusca may heal without any intervention, while others occur. Unlike other viruses, the molluscum contagiosum virus no longer exists within the body after healing. However, it remains possible to develop molluscum contagiosum again after repeated contact with an infected person or a contaminated fomite. Scarring is unusual in molluscum contagiosum unless lesions are scratched or scrapped. In immunocompromised persons, longer duration and resistance to therapy are common. Malignant transformation has never been reported.
Enhancing Healthcare Team Outcomes
The management of molluscum contagiosum is best done with an interprofessional team that also includes the primary care provider and nurse practitioner. The important thing is that these lesions spontaneously resolve in most patients; thus patient education is vital. Patients should be told that there is a small risk of autoinoculation or infection of others. For those who decide to be treated, more than one session may be required. This information is important for the patient as it prevents them from seeking unnecessary therapies and making unreasonable demands. Parents should not keep children out of school, but the infected skin area can be covered with a garment. Since this virus can be sexually transmitted, the patient should be encouraged to practice safe sex and use barrier methods for protection. [13][14][15](Level V)
Outcomes
In the majority of patients, molluscum contagiosum resolves without any residual scars. The disorder is benign and spontaneous resolution is the usual outcome, but it may take 12-24 months. In some individuals, the lesions may persist for 3-5 years and may be disfiguring. Recurrences occur in one-third of patients. In patients with HIV or those who are immunocompromised, the lesions are generalized and occur when the CD4 counts are low. In these patients, spontaneous resolution of the lesions is rare.[16][17][18] [Level 5]