Continuing Education Activity
Silent myocardial ischemia is a condition of reduced oxygen-rich blood flow to the heart that occurs without chest discomfort or other symptoms of ischemic heart disease, such as dyspnea, nausea, and diaphoresis. However, diagnostic studies are often abnormal. ST-segment changes may be evident on electrocardiography. Echocardiography may show regional wall motion abnormalities. Scintigraphy may reveal perfusion defects.
Stable coronary artery disease is a risk factor, though patients with silent myocardial ischemia may or may not have coronary artery disease. Individuals with this condition need an aggressive diagnostic and therapeutic approach due to the increased risk of developing new coronary events compared to people with clinically detected ischemia. The presence of silent ischemia is a strong mortality predictor.
This activity for healthcare professionals is designed to enhance learners' competence in identifying patients with silent myocardial ischemia and managing the condition. Participants gain a deeper understanding of the nuanced diagnostic and treatment approaches to this condition, enabling them to contribute meaningfully within an interprofessional team caring for patients with silent myocardial ischemia.
Objectives:
Screen patients at risk for silent myocardial ischemia.
Differentiate between silent and symptomatic myocardial ischemia based on clinical presentation and diagnostic test results.
Develop a personalized management strategy for a patient diagnosed with silent myocardial ischemia.
Implement effective collaboration and communication protocols within an interprofessional team caring for patients with silent myocardial ischemia to optimize outcomes.
Introduction
Silent myocardial ischemia refers to a condition where myocardial blood flow is reduced without causing noticeable symptoms like chest pain or discomfort. This disorder is the most common clinical presentation of coronary artery disease (CAD). [1] Electrocardiogram (ECG), echocardiography, and perfusion abnormalities detect silent myocardial infarction. Silent myocardial ischemia is common in patients with stable CAD, though some patients do not have a history of CAD.
The presence of silent ischemia is a strong mortality predictor. About 70% to 80% of transient ischemic episodes lack anginal chest symptoms (silent ischemia). Lack of pain in silent myocardial ischemia increases morbidity and mortality since patients do not seek medical treatment in a timely fashion.[2][3] Older patients with diabetes mellitus (DM) and those with prior myocardial infarction or revascularization history are susceptible.
The diagnosis requires objective evidence of ischemia, which can be one of the following: ECG changes diagnostic of ischemia during ambulatory monitoring or stress testing, segmental wall motion abnormalities on exercise or dobutamine stress echocardiogram, or resting perfusion defects on nuclear scintigraphy.
Heart Anatomy Overview
The heart is a muscular organ in the chest cavity, slightly left of the midline. The heart consists of 4 chambers: the right atrium and ventricle and the left atrium and ventricle. Blood returns to the heart via the atria, while the ventricles pump blood out of the heart to the lungs and the rest of the body. The heart is enveloped by its protective sac, the pericardium.
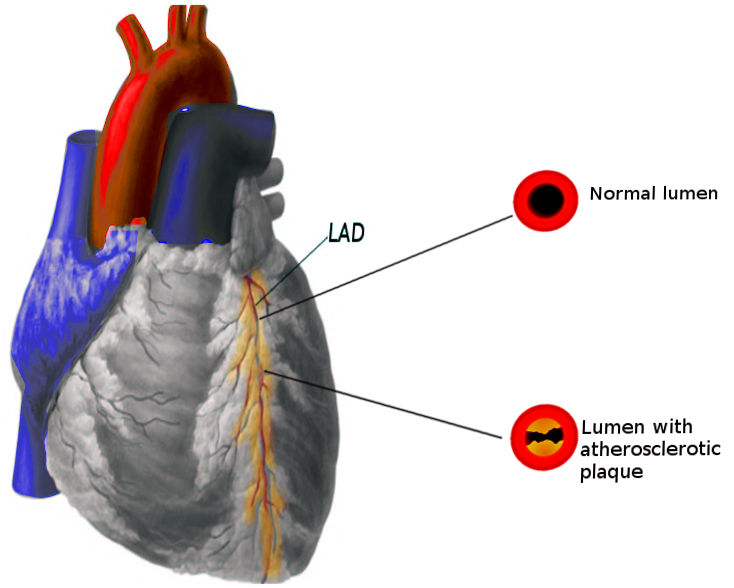
The coronary arteries branch off the aorta and supply oxygen-rich blood to the heart muscle (myocardium). The left coronary artery divides into 2 main branches: the left anterior descending and circumflex arteries. The left anterior descending artery supplies blood to the left ventricle's anterior wall and portions of the septum. The left circumflex artery provides blood to the left ventricle's lateral wall. The right coronary artery supplies the right atrium and ventricle and the left ventricle's inferior wall.
The coronary arteries penetrate the myocardium, forming an arterial anastomosis that delivers oxygen and nutrients essential for the heart's function. Disrupting the blood flow through these arteries from conditions like atherosclerosis or CAD can lead to regional wall motion abnormalities.
The myocardium consists of specialized muscle tissue responsible for the heart's contraction and relaxation. The myocardium's coordinated contraction ensures efficient systemic blood distribution. Regional wall motion impairment, observed through diagnostic tests like echocardiography, may indicate dysfunction or damage to specific cardiac areas. This dysfunction may be caused by inadequate blood supply due to coronary artery blockages, leading to conditions such as myocardial infarction or ischemic heart disease.
The heart's electrical activity originates from the sinoatrial node, which generates the electrical impulses responsible for initiating each heartbeat. These impulses spread through the atria, resulting in atrial depolarization, represented by the P wave on the ECG. After a brief delay at the atrioventricular node, the impulse travels through the bundle of His, bundle branches, and Purkinje fibers, leading to ventricular depolarization, depicted by the QRS complex on the ECG. Ventricular repolarization follows, represented by the ECG's T wave.
Silent myocardial ischemia typically arises due to coronary arterial obstruction, hindering adequate blood flow to the myocardium without producing noticeable symptoms. Understanding the intricate relationship between the anatomy of the heart and coronary arteries and myocardial function is crucial in evaluating and determining treatment strategies for patients with silent myocardial ischemia.
Etiology
Silent myocardial ischemia's most common causes include atherosclerotic plaque rupture, coronary vasospasm, coronary vasculitis, trauma, coronary embolism, sympathomimetic drugs like cocaine, and supply-demand mismatch. The associated risk factors play a significant role in causation. The following risk factors increase susceptibility to asymptomatic ischemic episodes and are pertinent to developing silent myocardial ischemia:
Diabetes Mellitus
DM is a significant risk factor for CAD and correlates with a higher incidence of silent myocardial ischemia. Cardiac autonomic dysfunction is the main culprit in patients with DM, which involves pain receptors, afferent neurons, or higher brain areas.[4][5] Studies have shown that atherogenic dyslipidemia strongly correlates with an increased risk of silent myocardial ischemia and CAD in patients with DM. Atherogenic dyslipidemia management may help reduce the high residual burden of cardiovascular disease.[6]
Perioperative Myocardial Infarction
The geriatric population has a relatively high perioperative myocardial infarction incidence. Studies have shown that patients who underwent coronary artery bypass grafting (CABG) had episodes of silent myocardial ischemia detected by Holter monitoring. Perioperative silent myocardial ischemia is usually asymptomatic. Hence, ECG monitoring is recommended during this period. Risk factors like prior myocardial infarction history and the presence of peripheral artery disease increase the odds of perioperative myocardial infarction.[7]
Older Patients
Older patients are particularly susceptible to silent myocardial ischemia. A study of 678 healthy men and women with no prior atherosclerotic cardiovascular disease revealed that the prevalence of silent myocardial ischemia, detected by Holter monitoring, was 11.4%. Silent ischemia in this population was associated with 3 times the risk of adverse cardiovascular events after adjusting for other risk factors.[8]
Intensive Care
Critically ill patients in the intensive care unit admitted for noncardiac causes are also at risk of acute myocardial ischemia. Transient myocardial ischemia and advanced age are significant predictors of cardiac events.
Sleep Apnea
Obstructive sleep apnea carries correlations with myocardial ischemia (silent or symptomatic), cardiac arrhythmias, pulmonary hypertension, heart failure, transient ischemic attack, and stroke.
Epidemiology
Patients with Prior Coronary Artery Disease
At least 15% to 30% of patients with acute myocardial infarction have evidence of prior silent myocardial ischemia, and at least 30% to 40% of those with unstable angina had prior myocardial infarction. Around 20% to 50% of patients with stable angina have a previous history of myocardial infarction.[9][10] A greater prevalence of multivessel CAD is apparent in patients with silent ischemia detected on stress testing. At least 20% out of 937 patients with stable CAD had inducible silent ischemia on stress testing.[11]
Patients without Prior Coronary Artery Disease
Silent myocardial ischemia is infrequent in patients without CAD. For example, the adjusted prevalence of silent myocardial ischemia was 0.89% in a cohort of 4842 patients undergoing serial ischemia evaluation.[12] However, this condition's prevalence varies with the presence and number of associated risk factors. For example, a prevalence of 22% was observed in a cohort of 631 asymptomatic patients with DM and 2 additional risk factors.[13] Further, the coronary artery's calcium score predicts individuals with silent myocardial ischemia, and a higher score is associated with an increased chance of ischemia.[14]
Studies show that silent myocardial ischemia's incidence rate is higher in men than women. Both men and women with silent myocardial ischemia experience an elevated risk of coronary heart disease deaths and all-cause mortality. However, women are anticipated to face a more significant increase in risk.[15]
Pathophysiology
Silent myocardial ischemia resembles the pathophysiology of myocardial infarction from any cause. An imbalance between oxygen demand and supply can produce the condition.
Myocardial infarction primarily results from atherosclerotic plaque rupture in the coronary arteries. Atherosclerotic plaque formation involves inflammatory cell migration, cholesterol engulfment leading to macrophage transformation into foam cells, and growth factor release inducing fibrin and smooth muscle incorporation. Plaques may have a thin or thick fibrous cap. Plaque rupture causes devastating ischemic injury in regions where it occurs (see Image. Coronary Artery Disease Pathophysiology).[16]
Meanwhile, the following explanations are suggested for why certain patients experience silent myocardial ischemia: inability to reach the person's pain threshold, brief ischemic episodes going unnoticed, higher β-endorphin levels, more cytokines blocking pain transmission, and altered or defective pain perception.[17][18] Silent myocardial ischemia follows a circadian rhythm, with greater incidences in the early morning hours. This phenomenon may be attributed to certain hemodynamic or physiological factors with circadian variation, including increased heart rate and blood pressure, higher vasomotor tone, elevated adrenergic levels, and enhanced platelet aggregation.[19]
Histopathology
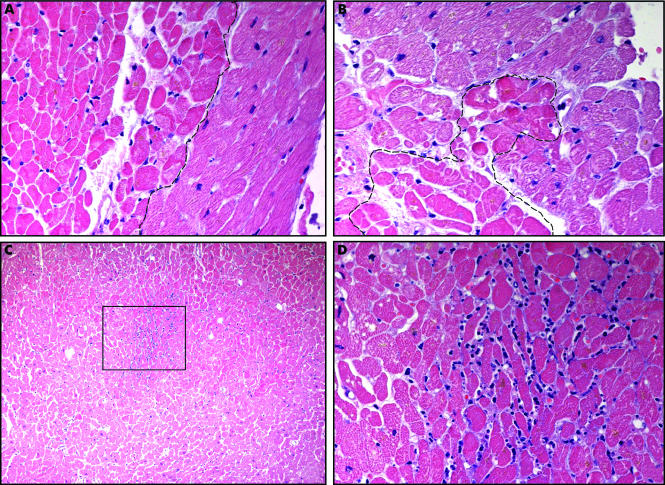
Histological findings become evident if the ischemic state remains long enough to initiate myocardial damage. The following findings may be appreciated in the setting of acute myocardial infarction.
- Characteristic histological features within the first 24 hours of insult include cardiomyocyte coagulation necrosis, neutrophilic infiltration, and interstitial edema and erythrocyte accumulation (see Image. Coagulative Necrosis in Myocytes During Silent Myocardial Infarction). Eosinophilic-appearing ischemic cardiomyocytes are evident with loss of the cross-striations and nuclei. Coagulative necrosis is established within the next 24 to 48 hours. After 3 to 5 days, myocyte nuclei and striations typically disappear in the infarct's central portion. After 5 to 7 days, macrophages and fibroblasts appear. At 1 week, neutrophil numbers start to decline, and granulation tissue forms with lymphocytic and plasma cell infiltration.
- Healing continues and may be complete as early as 4 weeks or require 8 weeks or longer, depending on the extent of necrosis. Occasionally, larger infarcts may heal at the borders, leaving the central area with mummified myocytes for extended periods.
- Reperfusion within 4 to 6 hours may result in a subendocardial infarct without transmural extension. Macrophages appear by day 2 to 3, and fibroblasts appear by day 3 to 5, with early signs of healing. Subendocardial infarcts heal earlier than nonreperfused infarcts. These lesions may undergo complete healing in 2 to 3 weeks. Infarcts that take longer than 6 hours to be reperfused produce extensive hemorrhage areas.[20][21]
Both myocardial infarction and silent myocardial ischemia involve hypoxic damage. However, myocardial infarction's histopathological features typically reflect more severe and irreversible tissue damage compared to silent myocardial ischemia, which may exhibit milder and more localized changes.
History and Physical
Patients with silent myocardial ischemia may have one of the following clinical presentations:
- Type I: Asymptomatic without prior myocardial infarction. Silent myocardial ischemia is detected on ambulatory monitoring or stress testing.
- Type II: Asymptomatic with a prior history of symptomatic myocardial ischemia
- Type III: Patients with known symptomatic or asymptomatic CAD, the largest group
Ischemic chest pain is the hallmark manifestation of acute coronary syndromes. Patients have either no history of prior myocardial infarction or angina, a previous myocardial infarction episode, or both angina and asymptomatic ischemic episodes.
The history of present illness and physical examination provide an immediate source of information for clinicians to stratify the patients for further workup. Pertinent comorbidities include DM, hypertension, dyslipidemia, and CAD or the presence of other CAD risk factors. The physical examination may be benign in these patients or suggest signs of ventricular dysfunction, such as S3, or ischemia, such as S4.
Evaluation
A 1-mm downsloping or horizontal ST depression is suggestive of myocardial ischemia in patients with previously normal ECG. Cardiac biomarkers like troponin-I and ambulatory ECG monitoring help detect postoperative myocardial infarction. These modalities may also help screen older individuals and patients with DM presenting to the hospital for unrelated complaints but are at risk of CAD. Radionuclide imaging is instrumental in detecting ischemia in asymptomatic individuals.
The following combination of tests is used to detect silent myocardial ischemia.[22][23]
- Bedside ECG monitoring is used for continuous cardiac electrical activity assessment and detection of ischemic changes.
- Cardiac markers measure the levels of enzymes or proteins released into the bloodstream during myocardial injury.
- Ambulatory ECG monitoring tracks cardiac activity during daily activities, providing valuable information on silent myocardial ischemia episodes.
- Exercise stress testing evaluates cardiovascular response to physical exertion to detect exercise-induced ischemic changes.
- Radionuclide imaging techniques provide functional assessment of myocardial perfusion to identify ischemic regions.
- Continuous intracardiac monitoring offers real-time assessment of cardiac function and ischemic events, which is particularly useful in high-risk patients.
- Computed tomography provides detailed anatomical imaging of the coronary arteries and myocardial structure.
These tests can provide valuable information about the presence and severity of myocardial ischemia to guide treatment decisions and risk stratification. Combining these tests can enhance diagnostic accuracy and improve care and outcomes.
Treatment / Management
Medical Therapy
β-blockers are the most efficacious option for enhancing outcomes in individuals with silent myocardial ischemia, significantly reducing the number and duration of ischemic episodes. Calcium channel blockers (CCBs) are also effective. CCB monotherapy is often primarily used in patients with CCB-responsive conditions, eg, vasospastic angina, or intolerance to β-blockers. Aspirin for antiplatelet therapy and statins for lipid lowering are also used. The combination of β-blockers, nitrates, and CCBs may be prescribed in patients who demonstrate ischemia on ambulatory monitoring or radionuclide scans.
Revascularization
Decisions on the necessity of coronary artery revascularization are not solely guided by findings consistent with silent myocardial ischemia, as data supporting the effectiveness of this intervention in treating silent ischemia is limited. A study showed no significant mortality difference between the groups who underwent revascularization and those who continued medical therapy (19.1% and 18.3%, respectively).[24][25] However, revascularization should be attempted in patients with high-risk features, such as ischemia to a large myocardial area, detected by ambulatory or noninvasive testing.
Psychosocial Stress Management
Mental stress can provoke silent ischemia, especially in patients with underlying CAD. Data suggests a possible benefit from behavioral stress reduction in individuals with CAD.
Differential Diagnosis
The differential diagnosis should include the following:
- Aortic dissection: Tear in the aortic intimal layer, causing layer separation and potentially life-threatening bleeding. Chest pain is prominent.
- Pleurisy: Inflammation of the pleura, resulting in sharp chest pain exacerbated by breathing or coughing. This condition may be accompanied by breathlessness and chest pain.
- Pulmonary embolism: Blockage of lung arteries, often by a blood clot, leading to sudden shortness of breath and chest pain.
- Myocarditis: Heart muscle inflammation that can cause fatigue, chest pain, and shortness of breath.
- Lung pathologies: Various diseases affecting the lungs, such as pneumonia, pulmonary fibrosis, and lung cancer, presenting with respiratory symptoms.
- Musculoskeletal etiology or those involving the gastrointestinal tract: Conditions affecting the muscles, bones, or gastrointestinal system, which can cause chest pain or discomfort, such as costochondritis, gastroesophageal reflux disease, or esophageal spasm.[26]
In contrast, silent myocardial ischemia is asymptomatic. However, chest pain and respiratory distress may arise if silent myocardial ischemia develops into an acute myocardial infarction. A thorough clinical history and judicious diagnostic evaluation can help differentiate silent myocardial ischemia from these conditions.
Prognosis
Silent myocardial ischemia's outcomes depend on the patient's risk factor profile and comorbid conditions like ischemic heart disease. Patients with a prior history of stable angina have a worse prognosis. Inducible ischemia in the absence of reported symptoms has twice the risk of a consequent ischemic event.[27] Patients with silent but documented ischemia on ambulatory monitoring also have greater chances of cardiac death.[28] Silent ischemia after an acute coronary syndrome episode is also associated with an increased risk of subsequent adverse events. In patients without CAD, the presence of silent ischemia, whether inducible or detected through ambulatory monitoring, correlates with an increased risk of adverse cardiovascular events and mortality.
Individuals with a history of silent myocardial ischemia have a higher incidence of new coronary events than people without silent ischemia, suggesting that an aggressive diagnostic and therapeutic approach must be employed for these patients. Older people present with atypical symptoms associated with acute myocardial infarction, including confusion, nausea, vomiting, and abdominal pain. Managing modifiable risk factors and adopting lifestyle changes can enhance patients' quality of life.[22]
Deterrence and Patient Education
Primary prevention of silent myocardial ischemia involves comprehensive management of cardiovascular risk factors to reduce the likelihood of developing CAD and subsequent ischemic events. Preventive measures include adopting healthy lifestyle habits, such as regular physical activity, maintaining a balanced diet low in saturated fats and cholesterol, achieving and maintaining a healthy weight, and avoiding tobacco use. Additionally, managing hypertension and DM and optimizing lipid levels also reduce the risk of developing this condition. Regular medical check-ups and screenings for cardiovascular risk factors, along with appropriate management of any identified risk factors, are crucial for early detection and intervention to prevent the onset of silent ischemia and its associated complications.
In patients already diagnosed with asymptomatic or symptomatic ischemia, cardiac rehabilitation programs are highly recommended to manage modifiable risk factors, handle stress, anxiety, and depression, and improve exercise capacity after hospitalization. This approach can help decrease morbidity and mortality. CAD risk factors should be treated aggressively in a patient with DM. The best approach is to perform screening ECG during yearly follow-ups.[29] Patients with silent myocardial ischemia tend to be older with multiple comorbidities. An interprofessional approach is required to manage such patients until rehabilitation.
Pearls and Other Issues
Silent myocardial ischemia is a condition characterized by reduced blood flow to the myocardium without causing noticeable symptoms like chest pain or discomfort. This condition's asymptomatic nature makes it particularly dangerous, as individuals may not be aware of the underlying heart condition until complications arise. The risk factors for silent myocardial ischemia align closely with those for symptomatic CAD, including hypertension, diabetes, smoking, hypercholesterolemia, obesity, lack of physical activity, and a family history of heart disease. Mechanistically, silent myocardial ischemia arises from processes similar to symptomatic ischemia, such as reduced blood flow to the heart due to coronary arterial obstruction, often from atherosclerosis.
Diagnosing silent myocardial ischemia presents challenges due to the absence of noticeable symptoms, often requiring incidental detection during routine medical evaluations or through diagnostic tests such as electrocardiograms (ECGs), stress testing, or coronary angiography. Despite the absence of symptoms, silent myocardial ischemia elevates the risk of serious complications such as myocardial infarction, heart failure, and sudden cardiac death. Screening individuals with CAD risk factors is essential to detect silent myocardial ischemia early.
Management strategies address underlying risk factors and improve coronary blood flow through lifestyle modifications, medications (including aspirin, statins, β-blockers, and CCBs), and, in some cases, invasive procedures like angioplasty or CABG. The prognosis depends on factors such as the extent of underlying CAD, treatment effectiveness, and coexisting medical conditions. Early detection and proper management are crucial for improving outcomes and reducing complication risks. Patient education plays a vital role in raising awareness about silent myocardial ischemia, emphasizing the importance of regular medical check-ups, lifestyle modifications, and medication adherence to mitigate complication risks, especially in individuals with cardiovascular risk factors.
Enhancing Healthcare Team Outcomes
An interprofessional approach is best for optimizing treatment outcomes for people with silent myocardial ischemia. The team typically includes cardiologists, primary care physicians, nurses, pharmacists, and dietitians.
Cardiologists play a central role in diagnosing and managing silent ischemia, utilizing diagnostic tests such as ECG, stress testing, and coronary angiography to assess cardiac function and ischemic burden. These providers also prescribe medications, such as β-blockers and antiplatelet agents, and may recommend invasive procedures like angioplasty or CABG when indicated. Primary care physicians coordinate overall patient care, provide preventive services, manage comorbidities, and refer patients to specialists as needed. Radiologists or nuclear medicine specialists interpret imaging studies to assess myocardial perfusion and detect ischemic regions.
Nurses are crucial in educating patients, monitoring symptoms, coordinating follow-up care, and ensuring adherence to treatment plans and lifestyle modifications. Pharmacists review medications, assess drug interactions, and provide medication counseling to optimize therapy and improve patient outcomes. Dietitians offer nutritional counseling, helping patients adopt heart-healthy dietary habits to manage risk factors such as hypertension and hyperlipidemia.
Besides the core team members, other healthcare professionals may be involved in caring for patients with silent myocardial ischemia. Mental health specialists may provide psychosocial support and address any psychological stressors or mental health concerns impacting patient well-being and treatment adherence. Physical therapists may develop tailored exercise programs to improve cardiovascular fitness and diminish the risk of ischemic events. Thoracic and cardiovascular surgeons may perform invasive procedures like CABG to bypass obstructed coronary arteries, restoring blood flow to the ischemic myocardium and alleviating symptoms. These providers may also perform other surgical interventions such as valve repair or replacement if concurrent structural heart disease is present.[30]